IJCRR - 7(15), August, 2015
Pages: 68-73
Date of Publication: 11-Aug-2015
Print Article
Download XML Download PDF
PROFILE OF PATIENTS OF VENOUS THROMBOSIS IN MEDICAL WARDSAN OBSERVATIONAL STUDY
Author: Cheena Garg, Arjun Agarwal, Dhruva Chaudhry
Category: Healthcare
Abstract:Introduction: Venous thrombosis is not an uncommon entity in medicine wards. Clinically, in majority of patients of venous thrombosis one or the other risk factor can be identified. Radiological investigations like-Duplex sonography, Coronary Transhepatic Pulmonary Angiography(CTPA) and Magnetic Resonance Imaging (MRI) venography have revolutionized the diagnosis of these disorders. There is an urgent need and scope to identify factors contributing to thrombophilia. Method: A prospective observational study over a period of 7 months including all the patients admitted in one unit of medicine. Results: Overall prevalence of venous thrombosis was 4.18% (26 out of 622 patients). The mean age of patients was 40.7 \? 16.2 years. Patients were divided into two groups. Group 1 (19 patients) consisting of patients with venous thrombosis (11 patients) and pulmonary thromboembolism (8 patients). Whereas group 2 (7 patients) had patients with cortical venous thrombosis (CVT). CVT and Deep Vein Thrombosis (DVT) were predominantly seen in females while pulmonary embolism was common in males. While in Group 1, Dyspnoea and pedal oedema were the commonest features. In group 2, headache followed by focal neurological deficit was common. All the cases were confirmed by necessary radiological investigations. All patients received enoxaparin. Thrombololysis was additionally given to 5 patients of group 1.11 (42%) patients had one or more risk factors. Overall mortality was 26%.
Conclusion: Significant number of patients of venous thrombosis had one or the other risk factors. In this highly selective group wherever the tests were done, they demonstrated presence of thrombophilic state. It reinforces the belief that thrombophilias are prevalent in our population.
Keywords: Venous thrombosis, Pulmonary embolism, Cortical vein thrombosis, Thrombophilias
Full Text:
INTRODUCTION
Venous thrombosis is the formation of a clot or thrombus inside the veins, obstructing the flow of blood through the circulatory system caused as a consequence of Virchow’s triad. Venous thrombosis of the extremities is the commonest, followed by lungs (Pulmonary Thromboembolism) and brain. Venous Thromboembolic (VTE) disease is a common and potentially life threatening complication that incorporates signs and symptoms of 2 interrelated but distinct clinical conditions, Deep venous thrombosis(DVT) and Pulmonary embolism(PE). Signs and symptoms of VTE are non-specific like- swelling and pain in limbs, breathlessness, chest pain, cough and hemoptysis. Thus, making diagnosis difficult. Several risk factors have been advocated includingmalignancy, major orthopaedic surgery, spinal cord trauma, advanced age, obesity, immobilization, previous history of thrombosis, Ischaemic Heart Disease, smoking, atrial fibrillation, inherited causes- FactorV Leiden, hyperhomocysteinemia, deficiencies of Antithrombin III, Protein C and S.1,2 Cortical venous thrombosis(CVT), is also a challenging condition because of its myriad presentation. It is not so rare, but an alarming disease usually beginning with severe headache and may lead to seizures, neurological deficits and even death. It has been reported to cause 10-20% young strokes in India.3,4 A multitude of risk factors have been associated with CVT, including- all the prothrombotic states mentioned earlier, pregnancy, puerperium, infection and some other causes still remaining unknown(20-25%).5.
MATERIALS AND METHODS
Ours was a prospective observational clinical study carried out over a period of seven months in a medicine unit. Inclusion criteria-All confirmed cases of venous thrombosis in the medicine unit were eligible for the study. Venous thrombosis was defined to include- Deep Vein thrombosis of legs, Cortical vein thrombosis, Venothromboembolic diseases, Axillary vein thrombosis, Mesentric vein thrombosis.
RESULTS
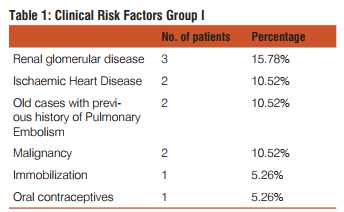
Out of total 622 patients admitted in the hospital unit, 26 (4.18%) suffered from venous thrombosis. For the study, they were further divided into two groups: Group I – Patients having venous thromboembolic (VTE) disease (19 patients) (73.1%) including deep venous thrombosis (DVT, 11 patients i.e. 58% ) and pulmonary thromboembolism (PTE, 8 patients i.e. 42% ). Group II – patients with cortical venous thrombosis (CVT) (7 Patients i.e. 26.9%). There was a variable distribution of age with a very wide range from 20-75 years with mean age of 40.7±16.2 years. Nearly 3/4th of the patients were in the range of 20-50 years (73.1%). In group I 14 patients and in group II 6 patients were in the said range, respectively. There was almost equal no. of males and females in group I. However, there were more females (7 out of 11) in the DVT subgroup and more males (6 out of 8) in the PTE subgroup. In group II all the patients were females except one. In group I, the mean age of presentation was 43.42±16.1 years. Majority of patients had breathlessness and swelling feet. While others had distended abdomen, ascites, chest pain, cough and pain in legs. There was only 1 patient with hemoptysis. Majority of patients had pallor on general physical examination (12 patients) (63.15%), followed by pedal edema, facial puffiness and cyanosis. 4 patients (21.05%) had raised Jugular Venous Pressure. Clubbing was present in only 1 patient who had carcinoma lung. All patients were hemodynamically stable, however most patients were tachypnoeic.3 patients (15.78%) had systolic murmurs (one had ejection systolic murmer in Pulmonary area, other in both Pulmonary area and Tricuspid area and third one had Pan Systolic Murmer in Mitral area and Tricuspid area). 6 patients (31.57%) had basal crepts, 4 patients (21.05%) had reduced air entry and 2 had (10.52%) spasm on inspiration. Collaterals on abdomen with flow below upwards were seen in 2 patients (10.52%) of IVC thrombus. One of them had Budd chiari syndrome and other one had ovarian carcinoma. Around 60% of the patients had one or the other clinical risk factor for VTE. (Table 1)
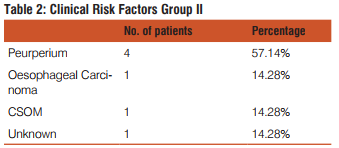
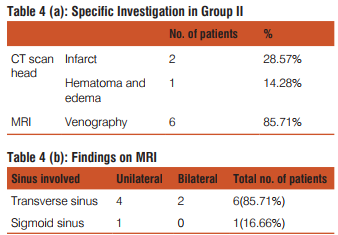
In group II, the mean age of presentation was 33.29±15.12 years. Majority of patients presented with headache followed by weakness of limbs and abnormal mentation. All patients were hemodynamically stable. There was no tachypnea.4 patients (57.14%) had abnormal higher mental function. Almost all patients had plantar silent or extensor. Hemiparesis incidently all left sided was observed in 3 patients. 2 had (28.57%) signs of meningeal irritation. Fundus examination showed papilloedema in one patient.
Risk factors were found clinically in all except one. (Table 2)
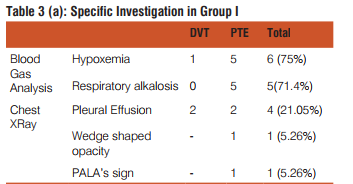
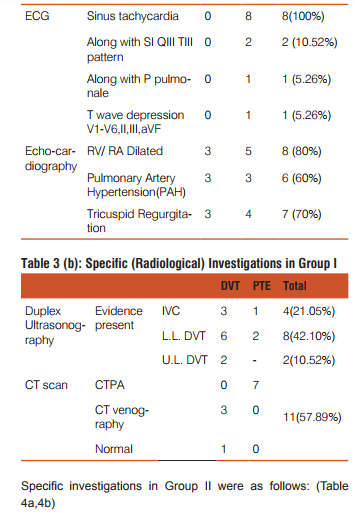
Baseline routine investigations were carried out in all the patients in both the groups and were insignificant statistically. Specific investigations in group I were as follows: (Table 3a, 3b)
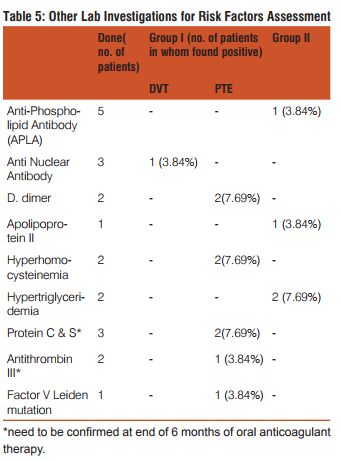
Laboratory evaluation of risk factor was done wherever possible to further investigate the cause of venous thrombosis.(Table 5)
The following treatment was given to the patients: Thrombolysis- 5 patients of VTE were thrombolysed, which included 4 patients of PTE and 1 of DVT. 4 patients were given Urokinase 1 patient had been previously thrombolysed with streptokinase was then thrombolysed with Tissue plasminogen activator (tPA Alteplase). Anticoagulant therapy20 (76.92%) patients were treated with low molecular weight heparin and 6 (23.07%) received heparin. All patients were given coumarin derivatives after thrombolysis and heparin or Low molecular weight Heparin therapy. Antiplatelet therapy-Clopidogrel was given in 8 patients (30.76%). Out of 26 patients, 19 (73.1%) patients were discharged after treatment while 7 (26.9%) patients expired
DISCUSSION
Thromboembolic events in India are still an under reported entity .In our study, the prevalence of venous thrombosis was 4.18% in the population studied (out of which 3.05% patients were diagnosed as VTE and 1.13% patients as CVT). According to a study, a prevelance rate of 10-20% of DVT has been reported amongst the medical patients. 6 The overall incidence of venous thromboembolism was reported as 1.83 per thousand per year (1.69 to 1.98) in the western population. 7 Whereas pulmonary embolism has an average annual incidence of 1 case per 1000 in the western population.8 Studies in India are too meagre in this respect and prevelance of VTE in our population is not known. Epidemiological data though is available on CVT from India, its exact incidence is debatable. During the last 40 years, there have been clinical series from India suggesting higher incidence of CVT in the subcontinent than the western world.9.10 In group I which included VTE patients ,the mean age of presentation was 43.42±16.1 years against 39±12.1 years in a study of pulmonary embolism patients from north India.11 Many other studies also reported increased risk of VTE in patients >40 years age.12,13,14 Thus, our study supports the fact that VTE is more common around 40 years. The same study of PE from north India showed that 17 males and 7 female patients were affected i.e. males were twice more predisposed to develop PTE than females. In our study also, nearly 3/4th patients of PTE (6 out of 8 patients of PE) were males However, DVT was commoner in females( 7 out of 11) as compared to males (4 out of 11)in the present study. Breathlessness and swelling foot were the commonest complaints in contrast to the previously mentioned study11, which demonstrated dyspnoea and cough as the main presenting symptoms. This could probably be because the above referred study was done purely on patients of PE while our study included both PE and DVT, thus, more patients with swelling foot. In the present study majority (57.8%) of the patients had at least one risk factor known to predispose to VTE. However, they showed scattered distribution among the local population with no difference from literature. The risk factors observed were IHD, previous history of VTE, underlying renal glomerular disease , carcinoma ,intake of Oral Contraceptives and immobilization. Hypercoagulability in cancer patients may indicate an aggressive change in the tumor and is associated with tumor progression.15 VTE incidence is around 40-100 cases per 1000 person-years in lung carcinoma patients.16 Gastrointestinal and gynaecological malignancies have also been found to be associated with hypercoagulation more frequently.17 Interestingly, 3 patients who had venous thrombosis associated with malignancy, one patient each had lung, ovarian and esophageal carcinoma. Many studies published in the last decade, reported that the incidence of venous thromboembolism (VTE) was higher in women who used oral contraceptives (OCs).18, in more so with third generation , as was seen in one of our subjects. In group II , the mean age of presentation was 33.29±15.12 years which was similar to a previous study from India on CVT (had mean age as 33.27 years).19 It had 41% female patients whereas in our study nearly all patients (85.7%) were females. All the patients had some or the other risk factor predisposing to CVT. Most of the females were in their pospartal periods. Puerperium has a strong relationship with CVT probably due to increased levels of clotting factors during pregnancy and hormonal changes. 10It is further complicated by local customs of not hydrating the mother adequately. Therefore, it was not a surprise to observe young females mostly in their postpartal periods with CVT. On laboratory tests, positive APLA and hypertriglyceridemia were revealed in a patient each. Several researches all over the world indicate that APLA20,21,22 hypertriglyceridemia 23,24 are proven prothrombotic states .In patient of CSOM with mastoiditis, direct extension of infection to the ipsilateral transverse sinus is supposed to be the cause of venous thrombosis. Headache was the commonest presenting symptom in 71.42% of the cases. It was primarily due to raised intracranial tension secondary to impaired drainage of CSF and venous sinuses. Headache has been constantly found to be the commonest complaint 2,19,10 However, the incidence of seizures was lower(28.57%) in our study than Pillai et al (42%)19.This was due to more common involvement of Superior Saggital sinus in their study, while most of our patients had transverse sinus involvement(6 out of 7). Hemiparesis was also a common presentation in our study owing to the same reason.MRI venography due to ready availability was the main modality for diagnosis of CVT in our institution. MR venography not only seems to offer an important advantage as a non-invasive tool in diagnostic procedures but also seems useful as a follow-up instrument for documentation of thrombus regression, recanalisation and venous collateralisation.25 In group I, echocardiography showed PAH in 60% patients and dilated right ventricle and atrium in 80% patients, primarily suspected to have VTE as compared to 83.3% and 62.5% , respectively in the PGIMER study.11 .73.68% patients had evidence of DVT on Duplex ultrasonography in the present study. Lower limb DVT was more common as with many other studies .The sensitivity and specificity of duplex for proximal vein thrombosis is 98%. Further, it helps to differentiate venous thrombosis from hematoma, Baker’s cyst, abscess, other causes of leg pain and edema.6 7 out of 8patients of PTE were confirmed on CT pulmonary angiography. The use of spiral CT pulmonary angiography(CTPA) is a major advancement in the diagnosis of PE with sensitivity and specificity greater than 90%.26. Therefore, the present study confirms the utility of CTPA in the diagnosis of PE. In our hospital thrombolysis was carried out in 5 patients, of which 3 had right ventricular dysfunction and one had IVC thrombus. Thrombolysis is being used more commonly now a days, not only for treating massive PE with shock but also in patients with echocardiographic evidence of right ventricular dysfunction.27,28,29 Such therapy has been shown to preserve the pulmonary microcirculation after pulmonary embolism and to decrease the incidence of the post-thrombotic syndrome following deep venous thrombosis27 Certain specific investigations like-factor V leiden, APLA,ATIII levels, Protein C and S levels, etc. were carried out in some cases .These tests though promising, but due to their non-availability in the hospital and for economic considerations were not carried out in every case on presentation. Moreover, majority of the investigations like- Protein C and S are more relevant when done after 6 months of anticoagulation therapy as their levels may be initially falsely low due to consumption of clotting factors.
CONCLUSION
Our study has demonstrated that venous thrombosis is not an uncommon entity in medicine wards. It affects predominantly when people are economically most productive. Clinically, in majority of patients of venous thrombosis have one or the other risk factor can be identified. Radiological investigations like-Duplex sonography, CTPA and MRI venography have revolutionized the diagnosis of these disorders. They should be used at first instance wherever clinical probability is high. There is an urgent need and scope to identify factors contributing to thrombophilia.
ACKNOWLEDGEMENT
Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
1. Clagett GP, Anderson FA, Jr, Heit J, et al. Prevention of venous thromboembolism. Chest 1995;108 (Suppl 1):31234.
2. Bick RL, Haas S. Thromboprophylaxis and thrombosis in medical, surgical, trauma, and obstetric/gynecologic patients. Hematol Oncol Clin North Am 2003;17:21758.
3. Srinivasan K. Ischemic cerebrovasular disease in the young: Two common causes in India. Stroke 1984;15;733-5.
4. Nagaraja D, Sarma GR. Treatment of cerebral sinus/venous thrombosis. Neurol India 2002;50;2:114-6.
5. Deschiens M. Coagulation studies, factor V leiden, and anticadiolipin antibodies in 40 cases of cerebral venous thrombosis. Stroke 1996;27;1724-30.
6. Parakh R, Somaya A, Todi SK, Iyengar SK. Consensus Development Recommendations for the Role of LMWHs in Prophylaxis of Venous Thromboembolism : An Indian Perspective. SUPPLEMENT OF JAPI _ JANUARY 2007 _ VOL. 55.
7. Incidence of venous thromboembolism: a community-based study in Western France. Thromb Haemost. 2000 May ;83 (5):657-60 10823257.
8. Wells PS, Rodger M. Diagnosis of pulmonary embolism: when is imaging needed? Clin Chest Med2003:24:13-28.
9. Padmavati S, Gupta S, Singh B.A clinical study of 44 cases of hemiplegia in adult women. Neurol India 1957;5:59-65.
10. Srinivasan K.Cerebral venous and arterial thrombosis in pregnancy and puerperium:a study of 135 patients. Angiology 1983;34:731-46.
11. Agarwal R, Gulati M, Mittal BR, Jindal SK.Clinical profile, diagnosis and management of patients with symptomatic PE, PGIMER Chandigarh. Original article. Indian J Chest Dis Allied Sci 2006;48:111-114.
12. Nicolaides AN, Irving D. Clinical factors and the risk of deep venous thrombosis. In: Nicolaides A, editor. Thromboembolism Etiology. Advances in Prevention and Management. Baltimore, MD: University Park Press; 1975: 193–204.
13. Gillum RF. Pulmonary embolism and thrombophlebitis in the United States, 1970–1985. Am Heart J. 1987; 114: 1262–1264
14. Gjores JE. The incidence of venous thrombosis and its sequelae in certain districts in Sweden. Acta Chir Scand. 1993; 111 (Suppl 206): 16–24.
15. Ten Cate-Hoek AJ, Prins MH. Low molecular weight heparins in cancer Management and prevention of venous thromboembolism in patients with malignancies. [Epub ahead of print] Thromb Res. 2007 Nov 7.
16. Margot Tesselaar, ET, Susanne Osanto, Department of Clinical Oncology, Leiden University Medical Center, The Netherlands .Current Opinion in Pulmonary Medicine. 13(5):362-367, September 2007.
17. TAHRI A, El Hattaoui M,Charei N, El Belghiti M, Mahmal L, Tahiri F, Bouras N. Journal of Clinical Oncology, 2007 ASCO Annual Meeting Proceedings Part I. Vol 25, No. 18S (June 20 Supplement), 2007: 19672.
18. Farmer RD, Lawrenson RA, Thompson CR, Kennedy JG, Hambleton IR. Population-based study of risk of venous thromboembolism associated with various oral contraceptives. Department of Public Health and Primary Care, Charing Cross and Westminster Medical School, University of London, Chelesa, UK.Lancet,1997 Jan 11;349(9045):83-88.
19. Pillai Lalitha V, Ambike Dhananjay P, Nirhale Satish, Husainy S M K, Pataskar Satish. Cerebral venous thrombosis: An experience with anticoagulation with low molecular weight heparin. Critical Care Department, Lokmanya Hospital, Chinchwad, Pune, India. IJCCM 2005;9:14-18.
20. Petri, M. Epidemiology of the antiphospholipid antibody syndrome. J Autoimmun. 2000; 15: 145–151.
21. Schved JF, Dupuy-Fons C, Biron C, et al. A prospective epidemiological study on the occurrence of antiphospholipid antibody: the Montpellier Antiphospholipid (MAP) Study. Haemostasis. 1994; 24: 175–182.
22. Bick RL. Hypercoagulability and thrombosis. Med Clin North Am. 1994; 78: 635–665.
23. Carine J.M. Doggen; Nicholas L. Smith; Rozenn N. Lemaitre; Susan R. Heckbert; Frits R. Rosendaal; Bruce M. Psaty. Serum Lipid Levels and the Risk of Venous Thrombosis. Arteriosclerosis, Thrombosis, and Vascular Biology:Volume24(10)October 2004pp 1970-1975.
24. Larsen LF; Bladbjerg EM; Jespersen J; Marckmann P. Effects of dietary fat quality and quantity on postprandial activation of blood coagulation factor VII. Arterioscler Thromb Vasc Biol (United States) Nov 1997, 17 (11) p2904-9.
25. Dormont D, Axionnat R et al. MRI in cerebral venous thrombosis. J Neuroradiology 1994; 21 (2): 81-99.
26. Padley SPG.Lung scintigraphy vs spiral CT in the assessment of pulmonary emboli.Br J Radiol 2002:75:5-8.
27. Linn BJ, Mazza JJ, Friedenberg WR. Treatment of venous thrombotic disease. Postgrd. Med. 1988 79(6): 171-80.
28. South path S.A. thrombolytic therapy for venous thrombosis and pulmonary embolism. Baillieres clin hematol 1998. 11(3): 663-73.
29. Fattahi O.H. Thrombolytic Therapy for Deep Vein Thrombosis and Pulmonary Embolism. Shiraz E-Medical Journal. October 2001, Vol. 2, No. 4.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License