IJCRR - 7(15), August, 2015
Pages: 49-55
Date of Publication: 11-Aug-2015
Print Article
Download XML Download PDF
ANATOMIC VARIATIONS OF PARANASAL SINUSES IN PATIENTS WITH CHRONIC SINUSITIS AND THEIR CORRELATION, WITH CT SCAN STUDY
Author: Kate Sarika P., Mandke N. D. , Bahetee B. H.
Category: Healthcare
Abstract:The study of anatomic variation of paranasal sinuses is important to understand the pathophysiology of chronic sinusitis. The rate of anatomic variations in chronic sinusitis varies according to different studies but the data in Indian population is lacking. The purpose of this study is to assess the frequency of anatomic variations in chronic sinusitis in the subset of Indian patients presented to Medical Colleges and hospitals from 2011 to 2013. A total of 90 patients were included. We found concha bullosa
in 23% patients with higher incidence in inferior turbinate, nasal septal deviation in 65% patients with higher incidence on right side. 85% patients suffered from maxillary sinusitis. Haller cell was found only in 1 patient while Onodi and Agger nasi cells were not seen in any patient. To conclude, in view of the presence of these significant variations, we reemphasize the need for proper preoperative assessment in every patient in order to accomplish a safe and effective endoscopic sinus surgery. The present
study is a step to provide suggestive findings to surgeons regarding various parameters involved and our contribution to the enormous work of other research workers.
Keywords: Paranasal sinuses, Chronic sinusitis, Computed tomographic (CT) scan
Full Text:
INTRODUCTION
Complications are always a proven risk in any surgery, but location of few structures or relations make things still worst in the human body. This is well implicated to the location of ethmoids which is so complex and has always been an area of challenge to the operating surgeon. This very fact interested me to explore the anatomy and its variations in the region of paranasal sinuses through my proposed present study. Drainage and ventilation of paranasal sinuses are important for the normal function which in turn depends on effective mucociliary clearance. (1) Drainage of secretions in paranasal sinuses follows definite course.(2) The frontal and maxillary sinuses communicates with middle meatus through prechambers. Mucosa of prechambers are closely opposed and clearance of is through ciliary action. These narrow prechambers are blocked by mucosal inflammation which affects ciliary clearance. It establishes a vicious cycle of infection and stasis causing chronic sinusitis.(2) The key region for these changes is that part of the lateral nasal wall that encloses the sinus ostia and their adjacent mucosa and prechambers. There is considerable anatomical variation in this area that may interfere with normal nasal function and predispose to recurrent or chronic sinusitis(3) Functional endoscopic sinus surgery restores normalcy by working on the key regions rather than on the larger sinuses. Good knowledge of anatomy is required for effective surgery. This is most true during endoscopic sinus surgery because of the intimate association with such vital structures as the orbit, optic nerve, anterior and posterior ethmoidal vessels, skull base and internal carotid artery. Anatomical variations in paranasal sinuses is more common in patients with chronic sinusitis which may be due to improper drainage. CT scan is standard imaging for detecting diseased paranasal sinuses along with their anatomical variations.(4)
AIMS AND OBJECTIVES
The complex anatomy of paranasal sinuses was explored by many researchers. The present study is an effort to contribute to their works. Our study is proposed to -
1. Evaluate the anatomical variations of paranasal sinuses by CT scan in chronic sinusitis patients
2. Study the proportion of anatomical variations of paranasal sinuses in patients with chronic sinusitis.
MATERIAL AND METHODS
The study was conducted at Medical colleges and Hospitals in Pune. We included patients who were referred for CT scan of PNS during a period of 18 months from December 2011 to May 2013. Unenhanced CT of the PNS was performed for 90 patients in the coronal plane, complemented by axial views. The investigations were performed by using SIEMENS SOMATOM SPIRIT single slice spiral CT machine. For coronal studies, patients were put in prone position. Taking the hard palate as reference axis, the plane of section was perpendicular to this structure. Direct scans 3 mm in thickness were made, from the anterior walls of the frontal sinuses to the posterior wall of the sphenoid sinus. For the axial scans, which were 5 mm thick, the orbitomeatal line was taken as reference with the patient in supine position. The exposure settings used were 130 kVp and 80 to 100 mAs. In all cases, systematic studies of the nasal sinus region were performed in coronal complemented by axial views in selected cases. Analysis of anatomical variants was performed both using a soft parts window and a bone density window
INCLUSION CRITERIA
Adult patients presenting with history of nasal obstruction, headache and who are subjected to radiological investigations after a clinical examination and diagnosis as chronic sinusitis were included in the study.
EXCLUSION CRITERIA
1. Paediatric age group( 0-15 years)
2. Patients with history of road traffic accidents of head, neck and face, sinonasal malignancy or past history of surgery in the paranasal region were not included in this study.
PARAMETERS RECORDED
The scans procured from various hospitals were then saved and evaluated for following structures and anatomical variations.
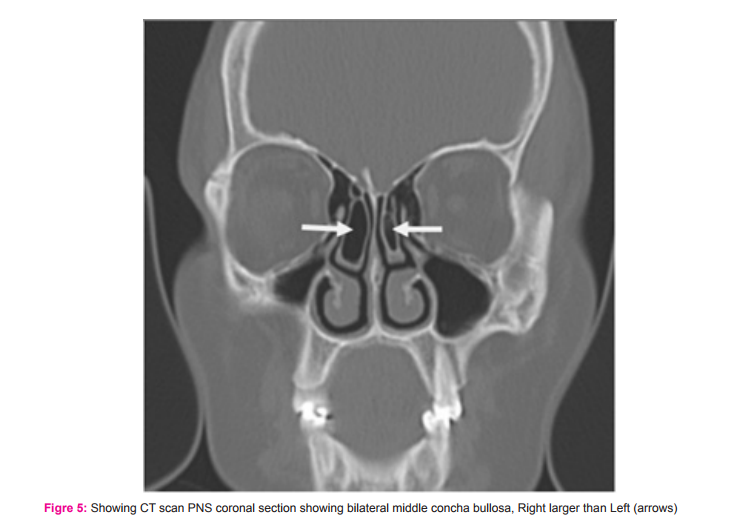
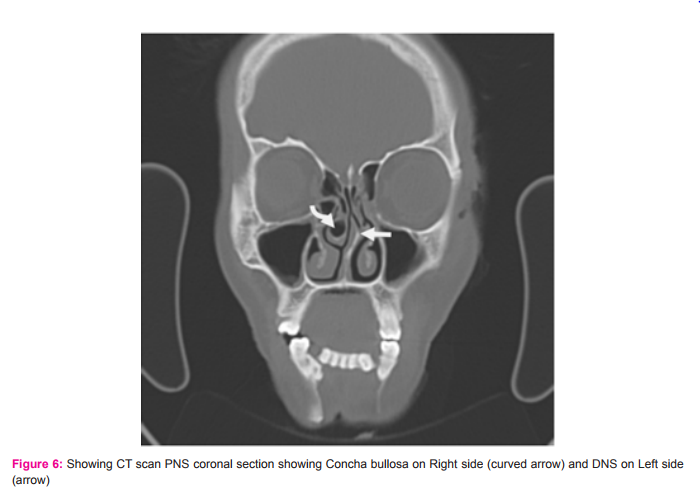
1. Turbinates: superior concha bullosa, middle concha bullosa, inferior concha bullosa
2. Nasal septum: septal deviation.
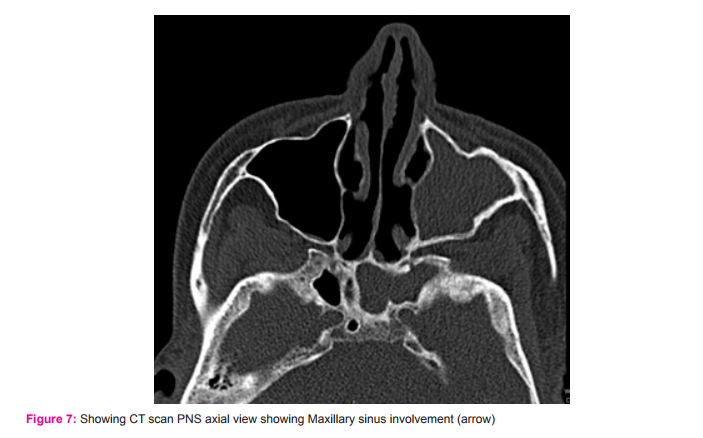
3. Sinus involved: Frontal ,maxillary, Anterior ethmoid, Middle ethmoid and Posterior ethmoid, Sphenoid.
4. Ethmoid air cells: Agger nasi cells, Haller’s cells, Onodi cells (extramural sphenoid cells).
STATISTICAL METHODS
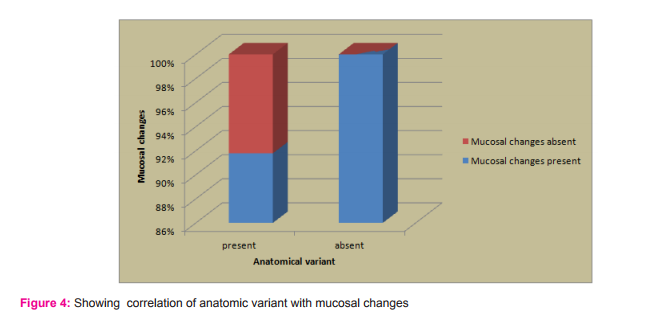
Percentage is taken into consideration in sex distribution, the presence of concha bullosa, incidence of deviated nasal septum, distribution of sinusitis, correlation of anatomic variants with mucosal changes.
RESULTS
1. Patients included in our study ranges between16 -76 years old. More patients lie in 21 to 30 years of age.
2. Out of 90 patients ,males were 52 (57.77%) while females were 38 (42.23%). So the present study has limitation of sex wise co-relation.
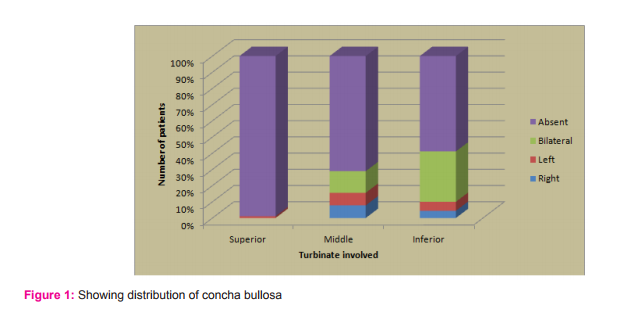
3. Out of 90 patients evaluated, averagely 23% patients show concha bullosa. Higher incidence is seen in Inferior turbinate (41%) while Superior turbinate was least involved.
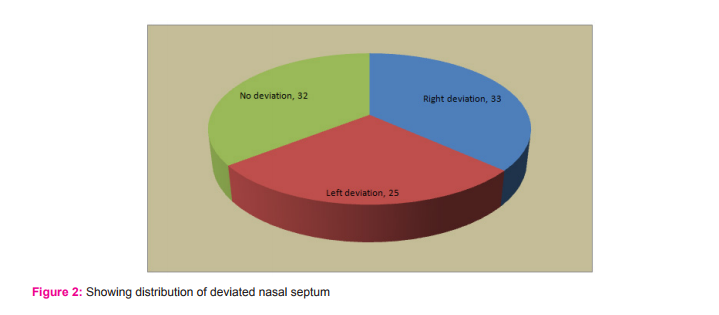
4. Out of 90 patients evaluated, right sided nasal deviation was seen in 33 (36%) patients. No deviation seen in 32 (35.52%) patients.
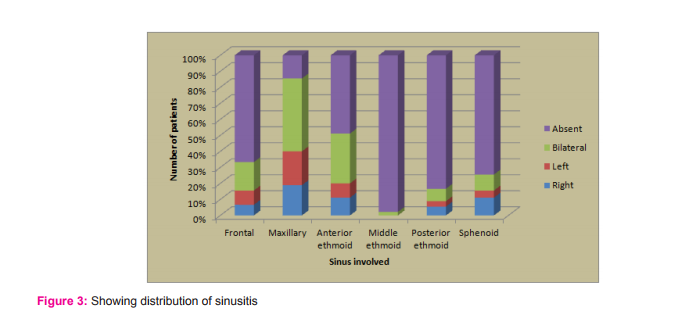
5. Out of 90 patients evaluated, the highest incidence of sinusitis was seen in maxillary sinus which was 85%(77 patients) while middle ethmoid 2%(2 patients) was least involved.
6. Anatomical variations were seen in 73(81.11%) patients out of which 67(74.44%) had mucosal changes. While Anatomical variations were absent in 17(18.84%) patients but they still suffered from chronic sinusitis.
7. Onodi cells and Agger nasi cells were not found in any patient.
8. Pansinusitis is present in 5 patients out of 90
9. Haller cell found only in1 patient out of 90.
DISCUSSION
In a study done in 90 subjects, paranasal region shows high percentage of anatomical variability, the variations most often observed were, in order, deviation of the nasal septum, the presence of a concha bullosa.
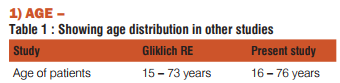
In our study patients age ranged from 16 to 76 years which was consistent with study done by Gliklich RE.
More patients lie in age group between 21 to 30 years.
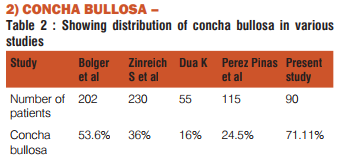
Concha bullosa (pneumatised turbinate) has been implicated as a possible aetiological factor in the causation of recurrent chronic sinusitis. It is due to its negative influence on PNS ventilation and mucociliary clearance in the middle meatus region. The presence of a concha bullosa has ranged between 4% and 80% in different studies; our data gave 71% which is more compared to Bolger(53.6%) ,Zinreich S et al (36%) and Dua K (16%) and Peres et al (24.5%). Such a wide range of incidence is due to the criteria of pneumatization adopted(1,5,11). 3)
DEVIATED NASAL SEPTUM –
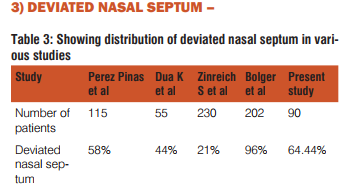
In our study deviated nasal septum seen in 58 patients( 64.44%) which is somewhat consistent with Peres Pinas et al while incidence seen by Dua K et al and Zinreich et al lies on lower side. Finding of Bolger et al lies on higher side.
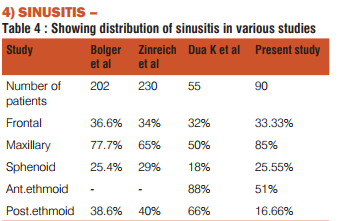
Various studies have reported the incidence of sinusitis in paranasal sinuses. In our study maxillary sinus was involved in 85 %, anterior ethmoids in 51%, sphenoid sinus in 25.55%, posterior ethmoids in 16.66 % and frontal sinus in 33.33% patients. The extent of involvement reported by other authors was also in the same range. Zinreich published maxillary sinus involvement in 65%, posterior ethmoids in 40%, frontal in 34%and sphenoid sinus involvement in 29%(9).Bolger reported maxillary sinus involvement in 77.7%, posterior ethmoids in 38.6%, frontal sinus in 36.6% and sphenoid sinus in 25.4%(5).
Pansinusitis was seen in 5.55 %.
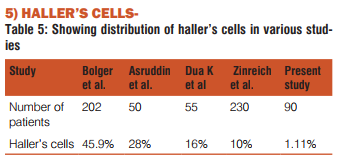
Haller’s cells are ethmoid air cells that project beyond the limits of the ethmoid labyrinth into the maxillary sinus. They are considered as ethmoid cells that grow into the floor of orbit and may narrow the adjacent ostium. The Haller’s cells in our study was seen in 1 patient (1.11%).It is less than that reported by Kennedy and Zinreich (10%) ,Bolger(45.9%) and Asruddin (28%)(5, 11, 12). The clinical significance of anatomical variants of the nasal sinus region is controversial. Most CT anatomical studies of the sinus region have been made in patients suspected of a clinical syndrome suggesting inflammatory sinus pathology.
Zinreich found that 62% of his patients presented at least one anatomic variant, against 11% in the normal control group(5). These findings seem to suggest a positive correlation between anatomical variants and the appearance of inflammatory sinus pathology. However, Bolger et al., in a series of 202 patients studied by CT, observed 131 anatomical variants, but found the incidence in patients with sinus pathology was similar to that in persons studied for other reasons(7). Bolger et al. and Stammberger and Wolf detected the presence of anatomical variants both in patients studied for sinus problems and in those studied for other reasons(8,6). They concluded that the simple presence of variants does not mean a predisposition to sinus pathology, except when other associated factors are present. This opinion is not shared by Yousem, who claimed that the anatomical variants may be predisposing factors, depending on their size (9). Anatomical variation were seen in 73(81.11%) patients out of which 67(74.44%) had mucosal changes.17(18.84%) patients showed absence of Anatomical variations but still suffered from chronic sinusitis. This suggests that patients may have mucosal changes without the presence of Anatomic variations. From this observation our study also reveals that the presence of anatomical variants does not mean a predisposition to sinus pathology. However, it is important for surgeon to be aware of variations that may predispose patients to increased risk of intraoperative complications. The radiologist must pay close attention to anatomical variants in the preoperative evaluation and help avoid possible complications and improve success of management strategies.
CONCLUSION
Computed Tomography of the paranasal sinus has improved the visualization of paranasal sinus anatomy and has allowed greater accuracy in evaluating paranasal sinus disease. It evaluates the osteomeatal complex anatomy which is not possible with plain radiographs. Improvement in Functional Endoscopic Sinus Surgery and CT technology has concurrently increased interest in the paranasal region anatomy and its variations. The present study has it’s own limitations of having less sample size and it is suggested to increase sample size to give significant contribution for clinical implications. Clinical studies shown that prevalence of concha bullosa in general population is more but very few subjects are symptomatic. To conclude, In view of the presence of these significant variations, we reemphasize the need for proper preoperative assessment in every patient in order to accomplish a safe and effective endoscopic sinus surgery. The present study is a step to provide suggestive findings to surgeons regarding various parameters involved and our contribution to the enormous work of other research workers.
ACKNOWLEDGEMENT
Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors/ editors/publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
1. Perez-Pinas I, Sabate J, Carmona A, Catalina H C J, Jimenez C J. Anatomical variations in the human paranasal sinus region studied by CT. Journal of Anatomy 2000;197(2):221–227.
2. Kopp W, Stammberger H, Fotter R. Special radiologic image of the paranasal sinuses. European Journal of Radiology 1998;8:152-156.
3. Blaugrund SM. Nasal septum and concha bullosa. Otolaryngol Clinics of North America 1989;22:291-306.
4. Clerico DM. Pneumatized superior turbinate as a cause of referred migraine headache. Laryngoscope 1996;106:874-879.
5. Zinreich S. Imaging of inflammatory sinus disease. Otolaryngol Clin North Am 1993;26:535-547.
6. Stammberger H, Wolf G. Headaches and sinus disease: the endoscopic approach. annals of otology, rhinology and laryngology 1988;97:3-23.
7. Bolger W E, Butzin C A and Parsons D S, Paranasal sinus bony anatomic variations and mucosal abnormalities: CT analysis for endoscopic sinus surgery. Laryngoscope 1991;101:56–64.
8. Bolger W E, Woodruff W and Parsons D S, CT demonstration of pneumatization of the uncinate process. Am. J. Neuroradiol 1990;11:552.
9. Yousem D. Imaging of sinonasal inflammatory disease. Radiology. 1993;188:303-314.
10. Zinreich J, Mattox DE, kennedy DW, Chisholm HI, Diffey DM, Rosenbaum AE. Concha bullosa: CT evaluation. Journal of computer assisted tomography 1988;12:778-784.
11. Dua K, Chopra H, Khurana AS, Munjal M. CT Scan variations in Chronic Sinusitis. Ind J Radiol Imag 2005;15:315-320.
12. Asruddin, Yadav SPS, Yadav RK, Singh J. Low dose CT in chronic sinusitis. Indian Journal of Otolaryngology and Head Neck Surgery 2000; 52: 17-21.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License