IJCRR - 7(15), August, 2015
Pages: 36-39
Date of Publication: 11-Aug-2015
Print Article
Download XML Download PDF
PREDICTION OF SIGNIFICANT HYPERBILIRUBINEMIA IN TERM NEWBORNS USING CORD BLOOD BILIRUBIN
Author: Ram Prasad Banasia, Hemant Jain
Category: Healthcare
Abstract:Aims: The present study was done to assess the usefulness of the cord blood bilirubin estimation as a predictor of subsequent neonatal hyperbilirubinemia in a healthy term infants who require phototherapy. Setting and Design: A prospective cohort study was conducted at tertiary care centre. 100 term newborn delivered by LSCS was included in this study.
Methods and Materials: 5ml of blood was collected from umbilical cord during delivery. It was used for estimation for conjugated, unconjugated, total serum bilirubin levels and blood group. All enrolled babies were followed up for 5 days and clinically assessed for jaundice according to Kramer dermal scale. In these babies, bilirubin estimation was done on samples collected at birth (cord blood), at 72 hrs. of life (3rd day), at 120 hrs. of life (5th day). Results: Cord blood bilirubin level of more than 2.15mg/dl has a sensitivity of 65% and specificity of 65% % in prediction of neonatal hyperbilirubinemia. Babies having serum cord bilirubin level of >2.15mg/dl can be followed up in the hospital for 5 days, the time of peak neonatal hyperbilirubinemia to prevent the babies discharged early and later readmission for neonatal hyperbilirubinemia. Conclusion: It is recommended to have cord blood bilirubin estimation of all healthy term babies delivered in an institution to prevent the dangerous consequences of neonatal hyperbilirubinemia like Kernicterus6
Keywords: Neonatal hyperbilirubinemia, Cord blood bilirubin
Full Text:
INTRODUCTION
Neonatal Hyperbilirubinemia1 is one of the most common cause for admissions in neonatal unit. Early discharge of healthy term babies from the hospitals is increased due to medical, social and economic reasons. The risk of readmission22 due to jaundice is increasing. The recognition, follow up and early treatment of jaundice has been difficult as a result of early discharges. The American Academy of Pediatrics5 recommends that newborns discharged within 48 hours should have a follow-up visit after 2-3 days to detect significant jaundice and other problems. This recommendation is not possible in our country due to limited follow up facilities in the community. The concept of early prediction of jaundice would facilitate safe and cost- effective targeted intervention and follow-up. The timely detection of neonatal hyperbilirubinemia9-12 and optimal management are crucial to prevent brain damage and subsequent neuromotor retardation due to bilirubin encephalopathy6 . Examination of newborns, cord blood bilirubin level is a non invasive procedure and can increase early detection to prevent severe hyperbilirubinemia.
MATERIAL AND METHOD
A prospective cohort study was conducted in department of pediatrics at tertiary care centre. 100 term newborn delivered by LSCS was included in this study. Newborn with congenital malformation were excluded. Other exclusion criteria include infant born to diabetic mother, neonatal sepsis, Rh incompatibility13 and conjugated jaundice.5ml of blood was collected from umbilical cord during delivery. It was used for estimation for conjugated, unconjugated, total serum bilirubin levels and blood group. All enrolled babies were followed up for 5 days and clinically assessed for jaundice according to Kramer dermal scale2 . In these babies, bilirubin estimation was done on samples collected at birth (cord blood), at 72 hrs. of life (3rd day), at 120 hrs. of life (5th day). Maternal variables like history of jaundice, first trimester bleeding, gestational hypertension, mode of delivery and uses of drugs during pregnancy were collected. Medication during labour, details of delivery, APGAR score and maternal blood group were recorded. Babies were examined daily and looked for evidence of jaundice, sepsis, illness or birth trauma. Weight of the newborn was recorded and gestational age calculated. All the babies were followed up daily for first 5 postnatal days. Serum bilirubin estimation was done within 12 hours of collection of sample by Diazotized sulfanilic test (Jendrassik modified method). The main outcome of the study was inferred in terms of hyperbilirubinemia. Serum bilirubin ≥12.9 mg/dl after 72 hours of life was taken as hyperbilirubinemia needing phototherapy and treatment is advised to all those full term healthy babies as per the American academy of pediatrics practice parameter. So in the present study babies with serum bilirubin level of ≥12.9 mg/dl are considered hyperbilirubinemia. ANALYSIS AND
RESULTS
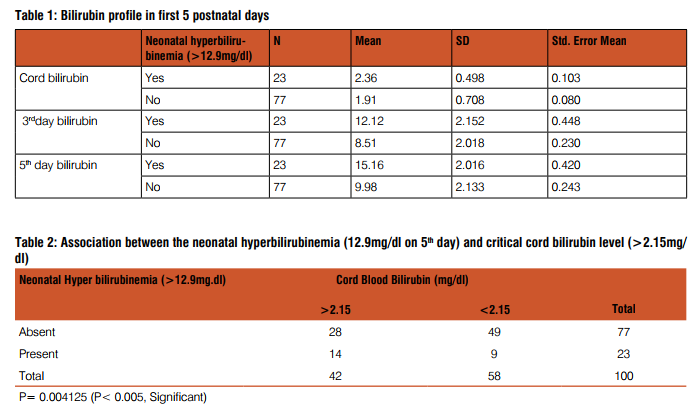
Statistical analysis- Statistical data were analyzed with the independent sample t test and the descriptive analysis and chi-square tests. Sensitivity, specificity, negative and positive predictive value of the test was calculated. The critical cord bilirubin level having the highest sensitivity and specificity was determined with the Receiver operating characteristics (ROC) curve analysis. Cord serum bilirubin concentration was used for developing ‘prediction test’. The sensitivity and specificity were calculated for predicting hyperbilirubinemia. The present study infers that cord serum bilirubin level of babies with neonatal hyperbilirubinemia (>12.9mg/dl on 5th day) is significantly higher (mean-2.36 mg/dl) than without hyperbilirubinemia (mean-1.91 mg/dl). Out of 100 newborn 23 newborn had significant hyperbilirubinemia on 5th day (mean-15.16 mg/dl). Bilirubin profile of first 5 days of post natal life (table 1) infers that babies with neonatal hyperbilirubinemia has significantly higher bilirubin level compared to babies without hyperbilirubinemia. Cord bilirubin level of >2.15 mg/dl cut off value is chosen based on the receiver operating characteristics (ROC) analysis. In the present study cord serum bilirubin level of >2.15 mg/ dl (table 2) has sensitivity and specificity both 65%, positive predictive value 65% and the negative predictive value of 64% in prediction of neonatal hyperbilirubinemia. So the cord serum bilirubin level of >2.15 mg/dl can be used as an early predictor of neonatal hyperbilirubinemia (p=0.004125). 3rd day bilirubin level of >10.15 mg/dl cut off value is chosen based on the receiver operating characteristics (ROC) analysis. In the present study 3rd day serum bilirubin (table 3) level of >10.15 mg/dl has sensitivity 87%, specificity 80%, positive predictive value 86% and negative predictive value of 81%. So the 3rd day serum bilirubin level of >10.15 mg/dl can also be used as an early predictor of neonatal hyperbilirubinemia (> 12.9mg/dl).
DISCUSSION
In this study, study group is uniformly distributed with 53 male and 47 female babies. There is no significant correlation (p 0.200) in the serum bilirubin levels and the sex of the newborn. Hence the present study infers that the neonatal hyperbilirubinemia (≥ 12.9mg/dl) is independent of the sex of the newborn. In this study, the timing of initiation of breast feeding is significantly (P=0.0183) associated with neonatal hyperbilirubinemia. Early introduction have less chance of hyperbilirubinemia. There is no significant association between the neonatal hyperbilirubinemia and maternal gestational hypertension with p value=0.476. On ROC curve analysis critical cord bilirubin level (≥2.15mg/ dl) with high sensitivity and high specificity is selected. The probability that a neonate with cord bilirubin ≥2.15mg/dl would later become hyperbilirubinemia (positive predictive value) was 65%. The negative predictive value, the probability of non-hyperbilirubinemia given a cord bilirubin lower than 2.15mg/dl was 64%. If a child become hyperbilirubinemic, the probability that the cord bilirubin was ≥2.15mg/ dl was 65% (sensitivity). Given a non-hyperbilirubinemic child, the probability that the cord bilirubin was 2.15mg/dl) and neonatal hyperbilirubinemia (>12.9mg/dl) on 5th day (p = 0.0041)18-21.
In this study, on ROC curve analysis critical 3rd day bilirubin level with high sensitivity and high specificity ≥10.15mg/dl is selected. The probability that a neonate with 3rd day bilirubin higher than ≥10.5mg/dl would later become hyperbilirubinemia (positive predictive value) was 86%. The negative predictive value, the probability of non-hyperbilirubinemia given a 3rd day bilirubin lower than ≥10.15mg/dl was 81%. If a child become hyperbilirubinemic, the probability that the 3rd day bilirubin was ≥10.15mg/dl was 87% (sensitivity). Given a non-hyperbilirubinemic child, the probability that the 3rd day bilirubin was <10.15mg/dl was 80% (specificity).
CONCLUSION
In the present study infants with neonatal hyperbilirubinemia had significantly higher levels of cord bilirubin. So it is possible to define a group of neonates at risk of developing jaundice needing phototherapy at birth. Simple knowledge of an increased risk of neonatal hyperbilirubinemia in a child could influence a decision of early discharge vs. prolonged observation.
ACKNOWLEDGEMENT
We acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. We are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
Ethical Clearance: Obtained from ethical committee.
Conflictof Interest: None.

References:
1. MacDonald, Mhairi G.; Seshia, Mary M. K.; Mullett, Martha D. Chapter 35-Jaundice, Physiologic Mechanisms of Neonatal Jaundice, Avery’s Neonatology. 6th Edition. Lippincott Williams and Wilkins; 2005: 773.
2. Kramer LI et al, advancement of dermal icterus in jaundiced newborn. Am J Dis Child 1969; 118: 454-458.
3. Martin CR, Cloherty JP, Eicchenwald EC, Stark AR. Manual of neonatal care: 7th ed: Wolters Kluwer, 2012; 304-339.
4. Niki papavramidou, Elizabeth Fee and Helen ChristopoulouAletra. Jaundice in the Hippocratic Corpus. Springer New York, Journal of Gastrointestinal Surgery 2007; 11(12) : 1728-1731.
5. American Academy of Pediatrics Subcommittee on Hyperbilirubinemia: Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004; 114: 297- 316
6. Brown AK. Kernicterus past, present and future. Neoreviews. 2003; 4: e33.
7. Bracken H. The Midwives Companion. Book 3, London 1737.
8. Gottlieb R. Bilirubin formation and the reticuloendothelial system, The Kupffer cells and their relation to the reticuloendothelial system. CMAJ 1934 Mar: 256-58.
9. Murchison C. Clinical Lectures on Diseases of the Liver, Jaundice and Abdominal Dropsy. Third Edition. William Wood and Co. New York 1885.
10. Hansen TWR. Pioneers in the Scientific Study of Neonatal Jaundice and kernicterus. Pediatrics. Aug 2000; 106(2):e15
11. Holt LE. Diseases of Infancy and Childhood. First Edition, D Appleton Co. New York 1897.
12. Ottenberg R. The etiology of eclampsia : historical and critical notes. J Amer Med Ass 1923; 81: 295.
13. Diamond LK, Allen FII, Thomas WO. Isoimmunisation Fetalis, VII Treatment with exchange transfusion. N Eng J Med. 1951: 244.
14. Landsteiner K. Wiener AJ. An agglutinable factor in human blood recognized by immune sera for rhesus blood. Proc Soc Exp Biol and Med 1940; 74: 309.
15. Hart AP. Familial icterus gravis of the newborn and its treatment. Canad Med Assn J 1925; 15: 1008.
16. Halbrecht I. Icterus precox: Futher studies on its frequency, etiology, prognosis and the blood chemistry of the cord blood. J Pediatr. 1951 Aug; 39:185-90.
17. Cremer RJ, Perryman PW, Richards DH. Influence of light on hyperbilirubinemia of infants. Lancet. 1958; 1094-97.
18. Amar Taksande, Krishna Vilhekar, Manish Jain, Preeti Zade, Suchita Atkari, Sherin Verkey. Prediction of the development of neonatal hyperbilirubinemia by increased umblical cord blood bilirubin. Ind Medica 2005; 9(1): 5-9.
19. Risenberg HM, Mazzi E, Macdonald MG, Peralta M, Heldrich F. Correlation cord bilirubin levels with hyperbilirubinemia in ABO incompatibility. Arch Dis Child 1977; 57: 219-222.
20. Rosenfeld J. Umbilical cord bilirubin levels as predictor of subsequent hyperbilirubinemia. J Fam Pract 1986; 23: 556-58.
21. Knudsen A. Prediction of the development of neonatal jaundice by increased umbilical cord blood bilirubin. Acta Paediatr Scand 1989; 78: 217-221.
22. Maisels MJ, Kring E Length of stay, Jaundice and hospital readmission. Pediatrics 1998; 101: 995-998.
23. Shally Awasthi and Hasibur Rehman. Early Prediction of Neonatal Hyperbilirubinemia. Indian J Pediatr 1998 ; 65 : 131-139.
24. Bhutani VK, Johnson L, Sivieri EM. Predictive ability of a predischarge hour specific serum bilirubin for subsequent significant hyperbilirubinemia in healthy term and near-term newborns. Pediatrics 1999; 103: 6-14.
25. IAP-NNF Guidelines 2006 on Jaundice in Newborn. 188-209.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License