IJCRR - 7(15), August, 2015
Pages: 32-35
Date of Publication: 11-Aug-2015
Print Article
Download XML Download PDF
NATURAL RESISTANCE ASSOCIATED MACROPHAGE PROTEIN 1 POLYMORPHISM SUSCEPTIBILITY TO MULTI DRUG RESISTANCE TUBERCULOSIS IN SOUTH INDIAN POPULATION: A CASE -CONTROL
STUDY
Author: Rooth Vasantha M., G. Sudhakar, S. Sridevi
Category: Healthcare
Abstract:Aim: To know the association of NRAMP1 gene polymorphisms in MDR-TB Patients. Methodology: Studies on NRAMP1 (Natural Resistance Associated Macrophage Protein1 or SLC11A1 revealed its function on macrophage activation and its association with infectious diseases. A case-control study was carried out to find the association of NRAMP1 gene with MDR-TB belonging to Visakhapatnam district of Andhra Pradesh, India. Genetic polymorphisms of NRAMP1 gene 3'UTR and 274 CT were analysed using Polymerase Chain Reaction-Restriction Fragment Length Polymorphism (PCR-RFLP).
Results: Significant statistical difference in the 3'UTR polymorphism between MDR-TB patients and healthy controls was observed. (P=0.001, OR=0.691,95%CI=0.077-6.208). But no significant association was found between the disease and 274 CT polymorphism (P>0.05). Conclusion: Significant association of MDR-TB with 3'UTR polymorphism of NRAMP1 gene was identified, while no significant association was observed in 274CT polymorphism of NRAMP1 gene. Further study with large sample size is required to confirm the above results.
Keywords: NRAMP1, 3’UTR, 274CT, MDR-TB
Full Text:
INTRODUCTION
According to World Health Organisation Global Tuberculosis report 2014, nine million people developed TB in 2013 and 1.5 million died of the disease(WHO, 2014(1)). The number of people developing the disease is declining by an average of 1.5% a year. However the report underlines that many lives are being lost to a curable disease and confirms that TB is the second largest killer disease from single infectious agent-Mycobacterium tuberculosis. Although routine surveillance efforts are increased yet millions of people who fall ill from TB are missed by health system each year, because they are not diagnosed or they diagnosed but not reported. The association of tuberculosis with HIV and increasing multi-drug resistant tuberculosis (MDR-TB) frames a serious issue especially in the developing nations (WHO 2014(2)) Increase in population rate along with disorders, linked with several socio-economic factors are operational in India, than in any other developing country. The proportion of patients with MDR-TB is increasing day by day due to insufficient treatment facilities. The progression of molecular study up to gene level in research has attributed much to the identification of the individual strains of MTB. The reason that many TB patients who are in the course of anti-TB treatment are stopping to take medicines, is that after seven weeks of using the drug, major symptoms of TB reduce and the patients assume that their health has improved. Thus a man made public hazard has become prominent (3). Treatment of MDR-TB has become difficult as the MTB became resistant to two most powerful anti-TB drugs Rifampicin and Isoniazid. MDR-TB patients who are not responding to the treatment are a constant source of transmission of multi-drug resistant MTB. In India many people have the habit of spitting the sputum in public places. If patients with TB and MDR-TB cough and spit in public places then the infection is transmitted by air through droplets of sputum dispersed into the environment. The amount of germs in the phlegm is also massive. Molecular study on Tuberculosis affected patients reveals that acquisition of TB does not occur due to horizontal transfer of resistance bearing genetic elements, but due to mutations (nucleotide substitution, insertions, or deletions in specific resistance determining region of the genetic targets. In humans, drug-resistance mutation in MTB occurs mainly within the lung cavities, where high loads of bacteria are present. Here active mycobacterial replication and reduced exposure to host defence mechanism was reported. Chromosome 2q35 was mapped with NRAMP1 gene (4). Many polymorphisms in this gene alter its function.NRAMP1 controls the replication of intracellular parasites by altering the intra vacuolar environment of the microbe containing phagolysosome (5,6). Mutations in this gene may play an important role in rapid screening of drug resistance among MDR-TB patients and early treatment can be initiated.
MATERIALS AND METHODS
33 In patients diagnosed with multidrug resistant TB were taken into study. Diagnosis was based on clinical and laboratory data retrieved from the clinical records maintained by Chest and Tuberculosis Hospital in Visakhapatnam between the time periods of July 2012 to Dec 2012. Diagnosis of the patients was done within the hospital laboratory using Lowenstein Jensen (L-J) medium. All the patients were under Anti-TB therapy. Patients were identified to have MDRTB if they were resistant to both Isoniazid and Rifampicin anti TB drugs. Data of these patients on basis of age, gender, drug resistance, habitual smoking and drinking, irregular treatment, details of prior treatment with anti-TB medication were recorded. Among the 33 MDR-TB patients, 27 were males and 6 were females. 100 healthy contacts were taken as controls. Written consent was obtained from all individuals taken into study. This study was carried out only after getting ethical approval from Institutional ethical committee, Andhra University.
DNA extraction
Isolation of Genomic DNA using salting out procedure was done in the Human Genetics Department laboratory of Andhra University, Visakhapatnam. After quantity and quality analysis using spectrophotometer and Agarose Gel electrophoresis, the isolated DNA was stored at -4o c.
Molecular analysis
3’UTR and 274 CT genotype analysis of NRAMP1 gene was carried out using Thermocycler. Primers used for the detection of SNP’s were purchased from Thermo scientific, restriction enzymes Fok1(NEB) and Mnll (Thermo scientific). PCR was performed in a total volume of 20µl of a solution containing 2µl of genomic DNA, 2.0 µl of 10×PCR buffer, 0.8 µl dNTPs, 0.5 µl of recombinant Taq polymerase (Invitrogen), 1 µl of Forward primer, 1 µl of reverse primer and 12.7 µl of sterile water. PCR amplification was carried out by operating the thermal cycler for 3’UTR NRAMP1/SLC11A1 polymorphism using the following conditions. 95o c for 5 mins,30 cycles of 95 oc for 30s, 52 oc for 30s and 72 oc for 30 sec with a final extension at 72 oc for 10 min. Primer sequence for 3’UTR, Forward: GCA TCT CCC CA TTC ATG GT. Reverse: AAC TGT CCC ACT CTA TCC TGC (Rahayu Anggraini et al., 2010(7). A region of 240 bp was amplified and genotyping was performed using restriction fragment length polymorphism analysis. The amplified PCR product was digested at 37o c for 2 hours with Fok1. The digested products were run on 2% agarose gel which is stained with Ethidium bromide and visualised under UV transilluminator. Primer sequence for 274 CT of NRAMP1 gene Forward: TGC CAC CAT CCC TAT ACC CAG. Reverse: TCT CGA AAG TGT CCC ACT CAG (Rahayu Anggraini et al., 2010). A region of 167 base pairs was amplified with annealing temperature of 56o c for 30 sec. The amplified PCR product is then digested at 37o c for 2 hours with Mnll restriction enzymes. The digested products were then run on 2% agarose gel stained with Ethidium bromide and visualised under UV transilluminator.
RESULTS
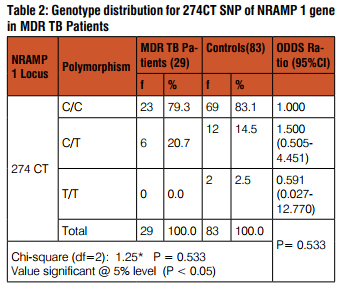
The observed results in Agarose gel electrophoresis for 3’UTR show genotype TGTG++ at 211bp and 33bp;TGTG+/ del genotype at 244bp,211bp, and 33bp;genotype TGTG del/ del at 244bp. Here the normal allele is TGTG+ and the mutant allele is TGTG del. For 274 CT polymorphism CC genotype at 102bp, 65bp, 37bp, and 12bp; CT genotype at 167bp, 102bp, 65bp, 37bp and 12bp; TT genotype at 167bp, 37bp, and 12bp.Here C is the normal allele and T is the mutant allele. Some of the PCR samples did not get amplified due to unseen reasons, so the sample size decreased to 29 MDR-TB and 89 healthy controls. A significant difference between the genotype frequencies of 3’UTR polymorphism of NRAMP1 gene in patients with MDR-TB and those in control group was observed.
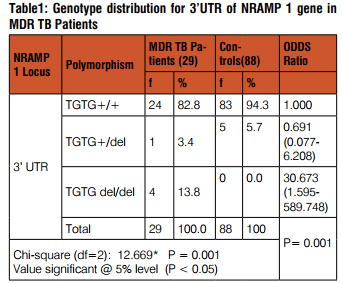
Among the MDR TB patients, about 83 percent are found to be homozygous for the genotype TGTG/TGTG for the 3’UTR region of NRAMP1gene. The frequency of heterozygous type (TGTG/TGTG del) is only 3 percent among MDR TB patients, The remaining 14 percent are homozygous for TGTG del/TGTG del type.(P= 0.001;Odds ratio0.691;95%CI=0.077-6.208)
Among the MDR TB patients, 79 percent are found to be homozygous for the genotype C/C for the 274 CT SNP of NRAMP1 gene. The frequency of heterozygous type (C/T) is 21 percent among MDR TB patients. The homozygous type T/T is not found in the present patient sample. (P=0.533;odds ratio=1.500;95%CI=0.505-4.451)
DISCUSSION
MDR-TB is a severe health problem in the world today. Nearly estimated 29% of the global tuberculosis cases come from India. Out of which 0.5% to 3.2% have MDR-TB. Gujarat state showed high rate of prevalence in India (8, 9, 10). The reason for MDR-TB emergence is due to drug discontinuation in middle of the treatment and the bacteria becoming susceptible to TB drugs. Hence Anti-TB drugs should be individually tailored for each MDR-TB patient as the standard treatment for drug-resistant TB is not known. And even after administering the treatment less percentage of cases showed favourable outcome. HIV is also expected to cause an increase in the percentage of MDR-TB (11, 12, 13) But HIV patients were not included in the present study. Natural mutation in NRAMP1 gene impairs early immunity to several intra cellular pathogens including mycobacterium. Increased frequency of specific NRAMP1 mutation among patients and control is observed in various studies. The distribution of NRAMP1 3’UTR polymorphism did not deviate from the Hardy Weinberg Equilibrium (P>0.05) the frequency of 3’UTR in MDR TB patients was 17.2% and that of controls is 5.7%. No significant association was found between MDR-TB patients and controls in 274 CT polymorphism of NRAMP1.3’UTR of NRAMP1 studies on Thais,(14) Chinese,(15) and Koreans(16) show significant difference in Pulmonary TB patients. Polymorphisms of SLC11A1 /NRAMP1 gene are known to influence phagolysosomal function of macrophages in iron transport, maintenance of acidity, and production of nitric oxide(NO)(17-20). The change in the phagolysosomal function of NRAMP1 gene may affect the viability of phagocytosed MTB leading to the development of drug resistant strains of MTB. Variations in 3’UTR leading to mutations could be one of the independent risk factor for MDR-TB and possible basis for drug penetration. This study suggests that NRAMP1/ SLC11A1 polymorphisms in part are associated with the emergence of multi drug resistance and extensive pulmonary involvement. Further study is necessary to confirm the association of 3’UTR of NRAMP1 gene with more number of MDR-TB patient samples.
CONCLUSION
The results obtained in the study suggest that variation in the NRAMP1/SLC11A1 gene is associated with the emergencef Susceptibility to multidrug resistance TB. Further study with larger sample size is required to confirm the association.
ACKNOWLEDGEMENTS
The authors are thankful for the UGC RGNF fellowship from the government of India, for funding of the research work. The author also acknowledges the published articles of the scientists and other dignitaries on Tuberculosis.
Conflict of interest: The authors declared no conflict of interest
References:
1. WHO .2013.Global tuberculosis report.
2. WHO.2014.Multi Drug and Extensively drug-resistance TB 2014. Global Report on Surveillance and Response 2014.
3. Article on Tuberculosis in Hindu Newspaper Magazine dated March 15/2015.Pg:4
4. Blackwell J et al., 1995. Genomic Organisation and Sequence of the Human NRAMP gene: Identification and mapping of a promoter region polymorphism. Mol Med.1:194–205.
5. Gruenheid S et al., Natural resistance to infection with intracellular pathogens; the NRAMP1 protein is recruited to the membrane of the phagosome. J. Exp Med 1997; 4:717-30.
6. Hackam D et al., Host resistance to intracellular infection: mutation of natural resistance associated macrophage protein 1(Nramp1) impairs phagosomal acidification. J.Exp Med 1998; 188:351-64.
7. Rahayu Anggraini et al., 2010. Polymorphism of Natural-resistance-Associated Macrophage Protien1 (NRAMP1)D543N gene and expression of NRAMP1 on Lung Tuberculosis Patients and Nurses in Surabaya. Folia Medica Indonesiana.Vol.46 No.2:78- 87.
8. Mendez AP et al., Global Surveillance for anti tuberculosis dug resistance, 1994-1997. N.Eng J Med.1998; 338:1641-49.
9. Jawahar MS. Multi drug resistance tuberculosis. ICMR bull 1999. 29:10-11.
10. Ramachandran R, Balasubramanian R. Chemotherapy of Resistant tuberculosis; the tuberculosis research center experience over 40 years. Indian J Tub 2000;47:201-10.
11. H.S. Subhas et al., Clinical characteristics and treatment response among patients with multi drug resistant tuberculosis; A retrospective study. India chest Dis Allied Sci 2003, 45:97-103.
12. Gilad J, Borer A, Riesenberg K, Peled N, schlaeffer F. Epidemiology and ethnic distribution of multidrug resistant tuberculosis in southern Israel,1992-1997. Chest 2000;117:738-43.
13. Suchindran S, Brouwer ES, Van Rie A .2009. Is HIV Infection a Risk Factor for Multi-Drug Resistant Tuberculosis? A Systematic Review PLoS One 4 (5): e5561.
14. Vejbaesya S, Chierakul N, Luangtrakool P, Sermduangprateep C. 2007. NRAMPI and TNF-Alpha polymorphisms and susceptibility to tuberculosis in Thais. Respiratory.12:202-206.
15. W. Liu, W.C. Cao and et al. 2004. VDR and NRAMP1 gene polymorphisms in susceptibility to pulmonary tuberculosis among the Chinese Han population: a case-control study. The international journal of tuberculosis and lung disease: the official journal of the International Union against Tuberculosis and Lung Disease. Vol: 8:428.
16. Ryu S et al., 2000. 3’UTR Polymorphisms in the NRAMP1 gene are associated with susceptibility to tuberculosis in Koreans. Int J Tuberc Lung Dis.4:577-580.
17. Govoni G, Gros P. Macrophage NRAMP1 and its role in resistance to microbial infections. Inflamm Res 1998.47:277–84.
18. Kuhn DE, et al., Iron transport into Mycobacterium aviumcontaining phagosomes from an Nramp1 (Gly169)- transfected RAW264.7 macrophage cell line. J Leukocyte Biol 2001.69:43– 9.
19. Hackam DJ et al., Host resistance to intracellular infection: mutation of natural resistance-associated macrophage protein 1(Nramp1) impairs phagosomal acidification. J Exp Med 1998.188:351–64.
20. Barton CH, Whitehead SH, Blackwell JM. Nramp transfection transfers Ity/Lsh/Bcg-related pleiotropic effects on macrophage activation: influence on oxidative burst and nitric oxide pathways. Mol Med 1995.1:267–79.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License