IJCRR - 7(15), August, 2015
Pages: 21-25
Date of Publication: 11-Aug-2015
Print Article
Download XML Download PDF
FUNGAL INFECTIONS - A CLINICOMORPHOLOGICAL SPECTRUM
Author: Thamil Selvi Ramachandran, K. Sivakami, Prakash H. Muddegowda, P. Venukeerthan
Category: Healthcare
Abstract:Introduction: Fungal infections at different sites are showing increasing incidence in both healthy and Immunocompromised individuals. Among the fungal infections, Aspergillus and Mucormycosis are the common infections, involving maxillary sinus, oral cavity, lung followed by each case of maduramycosis of foot and mucormycosis of forearm in this study. Aims: To study the clinical and pathological profile of fungal infections at various sites. Settings and Design: A Retrospective observational study conducted in Department of Pathology from Jan 2011- Dec 2012, VMKV medical college, Salem. Material and Methods: Seventeen cases were analyzed in this study with respect to clinical history, physical examination and neuroimaging [computed tomography (CT) or magnetic resonance imaging (MRI)] wherever necessary. Operated specimens were received in 10% formalin for histopathological examination. Results: Male:female ratio was 11:6. Mean age of 49 years. The common clinical presentations were nasal discharge followed by oral ulcer and foot ulcer. Commonest site of lesion was nasal cavity (59%). Mucormycosis was the commonest fungus. Conclusions: Early diagnosis and prompt treatment can reduce the mortality and morbidity of this lethal fungal infection.
Keywords: Fungal infections, Mucormycosis, Aspergillus, Oral ulcer
Full Text:
INTRODUCTION
Fungal infections at different sites are now-a-days showing increasing incidence in both normal and Immunocompromised individuals. Mucormycosis, a fulminant fungal infection, invades the arteries, forms thrombi within the blood vessels that reduces blood supply and causes necrosis of hard and soft tissues (1,2). Once within the arteries, the fungus may spread to orbital and intracranial structures. Aspergillus species are the most common cause of fungal sinusitis. (3,4)
AIMS
To study the clinical and pathological profile of fungal infections at various sites.
MATERIAL AND METHODS
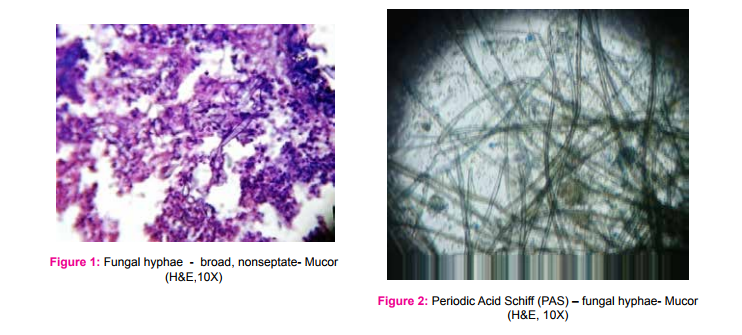
A Retrospective observational study from Jan 2011- Dec 2012 was conducted in the Department of Pathology, VMKV medical college, Salem. Seventeen cases were analyzed in this study with regards to clinical history, physical examination, and radiological examination( like X-Ray paranasal sinus view, neuroimaging [computed tomography or magnetic resonance imaging (MRI)] studies). Operated specimens were received in 10% formalin for histopathological examination. Routine Haematoxylin and Eosin stain and, when necessary, special stains like Periodic Acid Schiff stain(PAS) and Silver stains were done.
RESULTS
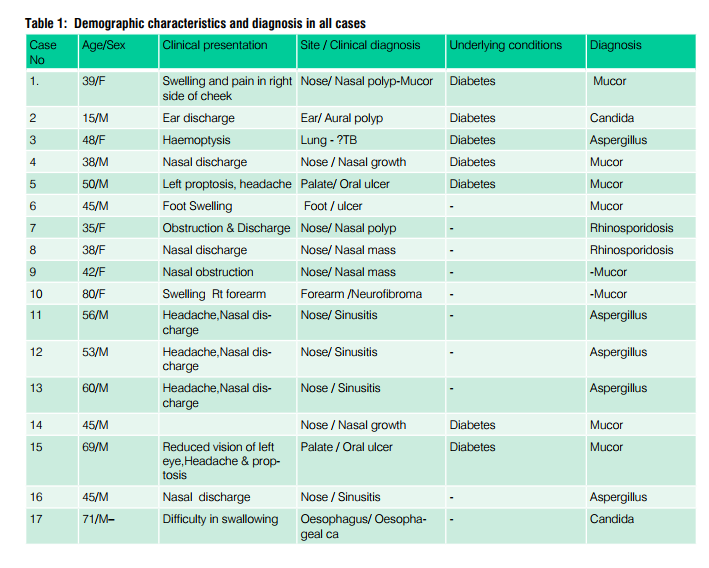
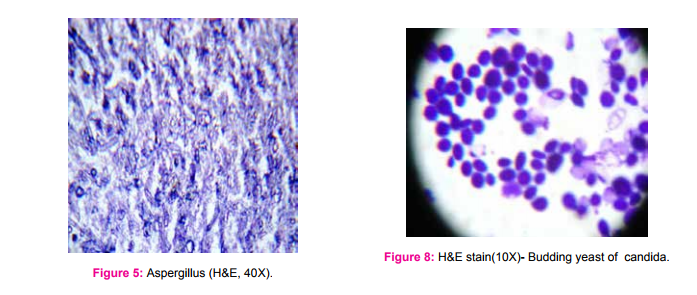
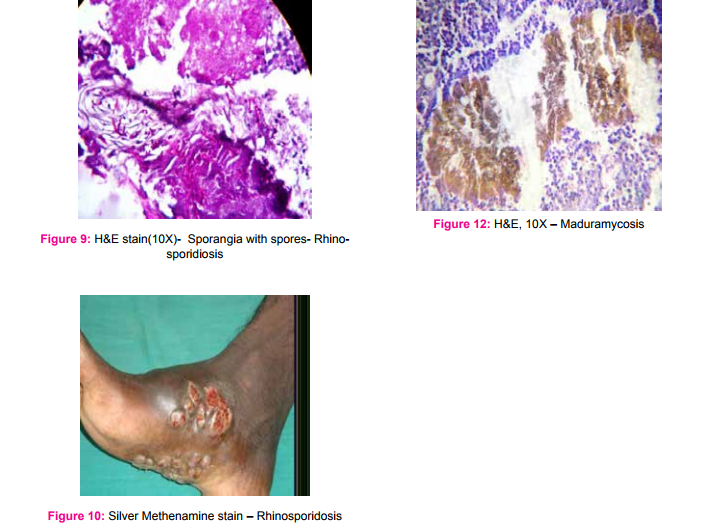
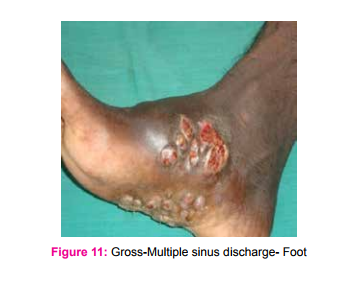
A total of seventeen cases were studied, with age range of 15 to 80 years. Mean age was 49 years and Male:Female ratio was 11:6. Most common presenting symptom was nasal discharge and clinical diagnosis was nasal polyp/growth. In six cases, the underlying disease was diabetes mellitus. (Table 1). X-ray paranasal sinus showed haziness of maxillarysinus in all cases. MRI revealed Orbital pseudo tumor in 3 cases and one case showed air filled cavity in the lung. In this study, Mucormycosis (Fig 1-4) was the commonest fungi (seven cases), followed by five cases of Aspergillosis (Fig 5 and 6) , two cases each of candida (Fig 7 and 8) and Rhinosporidosis (Fig 9 and 10). Only one case of maduramycosis was present in this study (Fig 11 and12). Periodic Acid Schiff (PAS) and Silver methenamine special staining technique demonstrated the fungus. Microbiology culture was positive in 7 cases.
DISCUSSION
In this study, histopathological examination with hematoxylin and eosin (H and E) stained sections showed various types of fungal infection with their characteristic feature, like abscess , necrotic material, inflammatory cells or granuloma composed of epithelioid cells, giant cells, surrounding the thin ribbon like fungal hyphae. The most common fungal infection in the present study was Mucor, an aggressive, opportunistic infection in the class of Phycomycetes, first described in 1885 by Paultauf. (5) Rhinocerebral mucormycosis is a rare opportunistic infection. It is mostly seen in association with immunosuppression as in this study, underlying conditions were diabetes mellitus and malignancy. (5,6,7) Ferry et al in 1983 and Yohai et al (8) in 1994, reported sinus involvement in 69% - 79% of mucormycosis respectively. In our study, it was 59%. Aspergillus species is the most common fungal infection of the paranasal sinuses. (6) Allergic Aspergillus sinusitis was first described as a form of fungal sinusitis by Katzenstein et al in 1983. (7) The typical presentation is nasal polyp associated with thick mucin and scanty fungal hyphae. However, culture is usually negative in most of the cases.(7,8) In our study, out of five cases of aspergillosis, only two cases showed positive culture. The next common fungal infection was candidiasis. Candida species, most often C. albicans, are the most frequent cause of human fungal infections. Diabetics patients are particularly susceptible to superficial candidiasis. Candidiasis takes the form of a superficial infection on mucosal surfaces of the oral cavity (thrush), oesophagitis, vaginitis, mucocutaneous and Invasive candidiasis. 9 We reported two cases of Rhinosporidiosis. It is characterised by hyperplastic polypoidal lesion of the nasal cavity. The organism of Rhinosporidiosis are huge, thick walled sporangia containing several thousands of spores. They elicit inflammatory response composed of neutrophils, lymphocytes and plasma cells. 10 In our study, we had only one case of maduramycosis. 13 species of fungi have been identified as causes of mycetoma. These include madurella mycetomi and Allescheria boydii . The condition occurs mainly in Tropical countries like India. The foot is most commonly involved, as in this study. 11
CONCLUSION
The early diagnosis and recognition of invasive fungal infection is very important, to prevent progression of the disease and avoid the high morbidity and mortality with this destructive disease.

References:
1. Leitner C, Hoffmann J, Zerfowski M, Reinert S. Mucormycosis: necrotizing soft tissue lesion of the face. J Oral Maxillofac Surg 2003;61:1354-8.
2. Pogrel MA, Miller CE. A case of maxillary necrosis. J Oral Maxillofac Surg 2003;61:489-93.
3. Zapico ADV, Suarez AR, Encinas PM, Angulo CM, Pozuelo EC. Mucormycosis of the sphenoidal sinus in an otherwise healthy patient. Case report and literature review. J Laryngol Otol 1996;110:471-3.
4. Jones AC, Bentsen TY, Fredman PD. Mucormycosis of the oral cavity. Oral Surg Oral Med Oral Pathol 1993;75: 455-60.
5. Paulltauf A. Mycosis mucorina. Virchows Arch [A]. 1885, 102- 543.
6. Stammberger M,Jakes R, Beaufort, Austria G. Aspergillosis of the paranasal sinuses: X-ray diagnosis, histopathology and clinical aspects. Ann Otol Rhino Laryngol 1984; 93:251-6.
7. Katzenstein AA, Sale SR, Greenberger PA. Allergic Aspergillus sinusitis. A newly recognized form of sinusitis. The Laryngoscope 1983;72:89-93.
8. Yohai RA, Bullock JD, Aziz AA et al, Survival factors in Rhinoorbito-cerebral mucormycosis. Surv opthalmol:1994; 39:3-22
9. Achkar JM, Fries BC. Candida infections of the genitourinary tract. Clin Microbiol Rev. 2010;23(2):253-73.
10. Sinha A, Phukan JP, Bandopadhyay G, Sengupta S, Bose K, Mondal RK, et al. Clinicopathological study of rhinosporidiosis with special reference to cytodiagnosis. J Cytol 2012;29(4):246- 9.
11. Bonifaz A, Tirado-Sánchez A, Calderón L, Saúl A, Araiza J, Hernández M, et al. (2014) Mycetoma: Experience of 482 Cases in a Single Center in Mexico. PLoS Negl Trop Dis 8(8): e3102. doi:10.1371/journal.pntd.0003102
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License