IJCRR - 7(15), August, 2015
Pages: 12-16
Date of Publication: 11-Aug-2015
Print Article
Download XML Download PDF
A RARE COMBINATION OF SYNCHRONOUS DOUBLE PRIMARY MALIGNANCIES - A CASE REPORT WITH LITERATURE REVIEW
Author: Balasubramanian A., N. S. Kannan , C. P. Ganesh Babu, M. Palaniappan, A. S. Mughilan
Category: Healthcare
Abstract:Aim: Aim of this study is to report a rare combination of synchronous double primary malignancies and to review the literature with reference to so far reported cases. Case Report: A 48 years old male patient presented to us with lower abdominal pain and burning micturition of one month duration. Based on clinical presentation and investigation reports he was diagnosed as a case of synchronous double primary malignancies of ascending colon and urinary bladder. After complete workup for both the malignancies, he underwent Trans Urethral Resection of Bladder Tumour (TURBT) and radical right hemicolectomy. Discussion: The term Multiple Primary Malignant Neoplasms (MPMNs), was first used by Billroth in 1889. They can be synchronous or metachronous. Extensive literature search shows only four cases of synchronous double primaries involving urinary bladder and colon. We are reporting a rare combination of synchronous double primary malignancies of urinary bladder and ascending colon. This is the fifth case report of synchronous double primaries involving bladder and colon and third case report involving bladder and ascending colon to the best of our knowledge. Conclusion: MPMNs are still elusive for want of proper guidelines regarding correct terminology and classification encompassing varying presentations of chronological, aetiological, clinical and histopathological combinations. Our case adds up to literature for further research. The possibility of occurrence of synchronous multiple primary malignancies should be considered during workup for any malignant condition to institute early intervention to achieve good outcome.
Keywords: Colonic adenocarcinoma, Synchronous primaries, Urothelial carcinoma
Full Text:
INTRODUCTION
The term Multiple Primary Malignant Neoplasms (MPMNs), was first used by Billroth1 in 1889. MPMNs are referred by some authors as multiple primary cancers (MPCs), or as Multiple primary malignacies (MPMs). Though the occurrence of multiple primary cancers has risen due to improvements in diagnostic techniques and treatment, the diagnostic criteria for multiple primary cancers remain the same as advocated by Warren and Gates2 in 1932. i.e. 1) Each cancer must be definitively malignant by histopathology, 2) they must be histologically different and 3) the possibility of metastasis among the cancers must be excluded. Differentiation between multiple primary and multicentric cancers was addressed in the classification by Moertel CG3 : I MPMNs of multicentric origin: a) The same tissue and organ. b) A common, contiguous tissue shared by different organs. c) The same tissue in bilaterally paired organs. II MPMNs of different tissues or organs. III MPMNs of multicentric origin plus a lesion (s) of a different tissue or organ.
In 2002, Howe in ‘A review of the definition for multiple primary cancers in the United States’ classified the association of different cancers in two categories depending on the timing of their discovery; a) synchronous in which the cancers occur at the same time or within two months and b) metachronous in which the cancers follow in sequence of more than two months apart4 . Vaamonde et al. reckoned the time factor as six months5 . In 2005, International Agency for Research on Cancer working Group has come out with International Rules for Multiple Primary Cancers6 .
CASE DETAILS
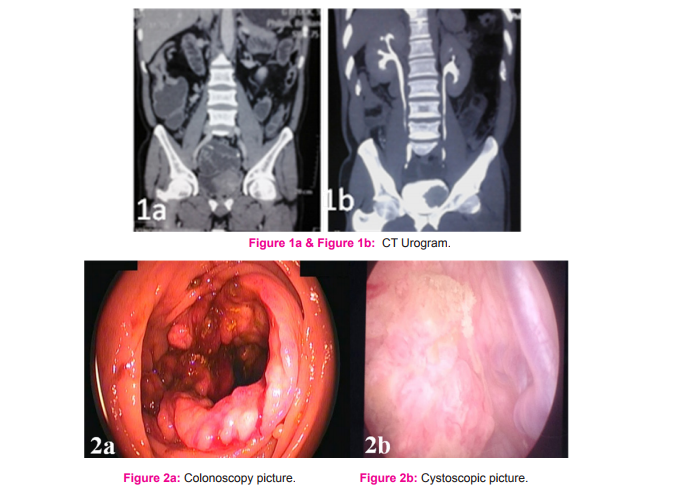
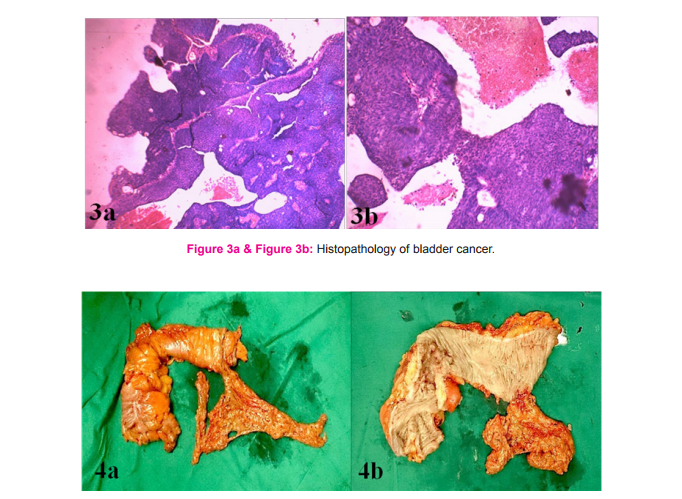
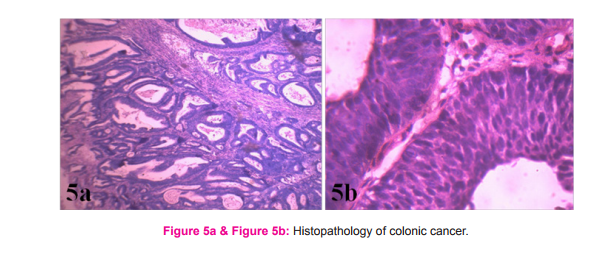
A 48 years old male patient presented to us with lower abdominal pain and burning micturition of one month duration and was evaluated for the same with ultrasonography abdomen, which revealed well defined isoechoic lesion in the left lateral wall of urinary bladder. Further evaluation with CT Urogram showed well defined heterogeneous enhancing lesion with speculations in the urinary bladder suggestive of carcinoma of bladder and incidentally discovered circumferential wall thickening involving the distal part of ascending colon causing partial obstruction with presence of multiple enlarged lymph nodes seen adjacent to the lesion. (Figure 1a and 1b). His serum CEA level was 38 ng/ml. Evaluation with colonoscopy showed circumferential proliferative growth in the distal ascending colon (Figure 2a). Biopsy taken from the growth at colonoscopy reported as adenocarcinoma. He was planned for cystoscopy, which showed a large (6x5cm) papillary growth in the left lateral wall of bladder and rest of the bladder normal (Figure 2b). Transurethral resection of bladder tumour (TURBT) was done and sent for Histopathological examination, which was reported as papillary urothelial carcinoma, low grade with focal invasion and bladder muscle free of tumour (T1G1) (Figure 3a and 3b). Patient was taken up for radical right hemicolectomy. At laparotomy found to have circumferential growth involving distal ascending colon with few enlarged lymph nodes at the adjacent mesocolon. Radical right hemicolectomy with ileotransverse anastomosis was carried out. Right hemicolectomy specimen is shown in (Figure 4a and 4b). Histopathological examination of the postoperative specimen was reported as well differentiated adenocarcinoma involving muscularis, pT2pN0 (Figure 5a and 5b). Postoperative period went uneventful and patient was advised regular follow up including periodic cystoscopy.
DISCUSSION
MPMNs/MPCs/MPMs, whether synchronous or metachronous are rare as such. Of late, the occurrence of multiple primary cancers has risen due to improvements in diagnostic techniques and treatment. According to study by Suzuki et al., most diagnosed synchronous double primary malignancies (SDPM) were lung cancer and head-neck cancers; metachronous double primary malignancies (MDPM) were lung cancer and breast cancer7 . They labelled the first of the MDPMs as MDPM-F and second one as MDPM-S. Double primary malignancies occurring at the same time or at the interval of 2-6 months apart are labelled as SDPMs4,5. Our case presented as synchronous double primary malignancies presenting at the same time. MPMNs prevalence ranged from 0.7 to 11.7% in various publications8-13. According to SEER (Surveillance, Epidemiology and End Results) data, the risk of developing subsequent MPMN varies from 1% for an initial liver primary diagnosis to 16% for bladder cancer primaries14. Ishimaro et al. published that at least 1.2% of patients referred to PET/CT with cancer diagnosis have a second cancer15. Although the mechanism involved in the development of multiple primary cancer has not been clarified, some factors such as heredity, constitution, environmental and immunological factors, oncogenic viruses, radiological and chemical treatments have been implicated16. Hereditary susceptibility explains only a small proportion of all second cancers though many hereditary cancer syndromes have been described17. MPMNs can occur at any age. However, from the reviewed series, patients with MPMNs tend to be older than those with a single primary malignant neoplasm. In many autopsy series and clinical reports, the median age of 50-94% of MPMN patients was over 50 years1,2,3,18,19 . Our case is a 48 years old male. The ratio of male/female patients with MPMNs in several publications varies between 0.9 and 3.5 with male predominance3,4,19-21. There are no established therapeutic rules for multiple primary cancers, but the type, progression, response to therapy and patient’s general health status should be considered. If each of the cancers has the possibility for cure, radical therapy is indicated. If radical therapy of the one primary cancer is impossible, conservative therapy is indicated for the other cancers22,23. Multiplicity of primary malignancies itself does not necessarily indicate a poor prognosis as long as adequate diagnosis and treatment are performed24. A review of 837 cases of colorectal carcinoma showed 32 cases (3.8%) of colorectal multiple primary malignant tumors and 11 cases (1.3%) of colorectal primary malignant tumour associated with extra colonic primary malignant tumour25. There are many reports in literature about double synchronous malignancies. In addition, there are many reports relating to MPMNs of more than two, up to eight MPMNs in the same patient26-30, but almost all of them are metachronous. Colonic primary with extra colonic primary along with other multiple primaries have reported earlier in the literature31,32. They are all metachronous in nature. In 2001 Sari R et al., has reported a case of synchronous double primary malignant neoplasms of colon and bladder33. In 2014, Liu Z et al. reported five patients diagnosed with synchronous bladder cancer and ColoRectal Cancers (CRCs) between May 1997 and September 2010. In this series, the primary colorectal tumors included three sigmoid cancers, one ascending colon cancer and one rectal cancer34. All the patients in this report underwent simultaneous radical cystectomy and CRC resection. Out of three sigmoid cancers, one was associated with recurrent bladder cancer. Hence, up to date literature search reveals only four cases of synchronous double primaries involving bladder and colon. Our case is unique due to its rare combination of synchronous primaries of urinary bladder (T1 N0 M0 ) and ascending colon (T2 N0 M0 ) presenting at the same time in 48 year old male, treated with transurethral resection of bladder tumour and radical right hemicolectomy in immediate consecutive sittings.
CONCLUSION
We have reported a rare combination of synchronous double primary malignancies of urinary bladder and ascending colon. This is the fifth case report of synchronous double primaries involving bladder and colon and third case report involving bladder and ascending colon to the best of our knowledge. MPMNs are still elusive for want of proper guidelines regarding correct terminology and classification encompassing varying presentations of chronological, aetiological, clinical and histopathological combinations. Influence of one primary over other and suggestions for best possible management are also yet to be defined properly. Our case adds up to the previously available ones for further research. The possibility of occurrence of synchronous multiple primary malignancies should be considered during workup for any malignant condition. As long as appropriate early interventions are performed in the synchronous multiple malignancies, good outcome is expected.
ACKNOWLEDGMENT
Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors/ editors/publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed. Authors are grateful to IJCRR editorial board members and IJCRR team of reviewers who have helped to bring quality to this manuscript.
Source of funding: Nil
Conflict of interest: Authors declare that they do not have any conflict of interest.
References:
1. Billroth T. General surgical pathology and therapeutics in: A textbook for students and physicians in fifty-one lectures. 14th ed. Berlin, DE: G. Rerimer; 1889.
2. Warren S, Gates O. Multiple primary malignant tumors; Surgery of literature and statistical study. Am J Cancer 1932;16:1358– 1414.
3. Moertel CG Multiple primary malignant neoplasms: historical perspectives. Cancer 1977;40(4 Suppl):1786-92.
4. Howe HL (Ed) A review of the definition for multiple primary cancers in the United States In Workshop Proceedings from December 4-6, 2002, in Princeton North American Association of Central Cancer Registries: New Jersey, Springfield (IL) 2003.
5. Vaamonde P, Martin C, del Rio M, LaBella T. Second primary malignancies in patients with cancer of the head and neck. Otolaryngol Head Neck Surg 2003;129:65-70
6. International Association of Cancer Registries. International rules for multiple primary cancers. Asian Pac J Cancer Prev. 2005;6(1):104-6.
7. Suzuki T, Takahashi H, Yao K Multiple primary malignancies in the head and neck: a clinical review of 121 patients. acta otolaryngol suppl 2002;547:88-92.
8. Demandante CG, Troyer DA, Miles TP Multiple primary malignant neoplasms: case report and a comprehensive review of the literature. Am J Clin Oncol. 2003;26(1):79-83.
9. Spratt JS Jr, Hoag MG. Incidence of multiple primary cancers per man-year of follow up: 20-year review from the Ellis Fischel State Cancer Hospital. Ann Surg 1966;164: 775-84.
10. Hajdu SI, Hajdu EO. Multiple primary malignant tumors. J Am Geriatr Soc 1968;16:16-26.
11. Berge T, Cederqvist L, Schonebeck J. Multiple primary malignant tumours. An autopsy study of a circumscribed population. Acta Pathol Microbiol Scand 1969;76:171-83.
12. Lee TK, Myers RT, Scharyj M, Marshall RB. Multiple primary malignant tumors (MPMT): study of 68 autopsy cases (1963- 1980). J Am Geriatr Soc 1982;30:744-53.
13. Aydiner A, Karadeniz A, Uygun K Tas S, Tas F, Disci R et al. Multiple primary neoplasms at a single institution: differences between synchronous and metachronous neoplasms. Am J Clin Oncol 2000;23:364-70
14. Hayat MJ, Howlader N, Reichman ME, Edwards BK. Cancer statistics, trends, and multiple primary cancer analyses from the Surveillance, Epidemiology, and End Results (SEER) Program. Oncologist 2007;12:20-37.
15. Ishimori T, Patel PV, Wahl RL. Detection of unexpected additional primary malignancies with PET/CT. J Nucl Med 2005;46:752-7.
16. Tamura M, Shinagawa M, Funaki Y: Synchronous triple early cancers occurring in the stomach, colon and gallbladder. Asian J Surg 2003;26(1):46-8.
17. Hawley AT, Pandolfi PP. Cancer susceptibility syndromes (Ch 12). In: De Vita VT, Hellman S, Rosenberg SA (Eds): Cancer: Principles and Practice of Oncology (8th Edn). Lippincott Williams and Wilkins, Philadelphia, Baltimore, New York, London, Buenos Aires, Hong Kong, Sydney, Tokyo, 2008, pp 157- 168.
18. Lee TK, Barringer M, Myers RT, Sterchi JM. Multiple primary carcinomas of the colon and associated extracolonic primary malignant tumors. Ann Surg 1982;195: 501-7.
19. Vyas JJ, Deshpande RK, Sharma S, Desai PB. Multiple primary cancers in Indian population: metachronous and synchronous lesions. J Surg Oncol 1983;23:239-49
20. Gürsel DM, Ozbek N, Ozdemir O, Odabas E. Multiple PrimaryMalignant Neoplasms from the Black Sea Region of Turkey. J Int Med Res 2011;39:667-74.
21. Ueno M, Muto T, Oya M, Ota H, Azekura K, Yamaguchi T. Multiple primary cancer: an experience at the Cancer Institute Hospital with special reference to colorectal cancer. Int J Clin Oncol 2003;8:162-7
22. Noh S K, Yoon J Y, Ryoo U N, Choi C H, Sung C O, Kim T J. A case report of quadruple cancer in a single patient including the breast, rectum, ovary, and endometrium. Journal of gynecologic oncology, 2008;19(4):265-69.
23. Yoshino K, Asanuma F, Hanatani Y, Kumai K, Ishibiki K: Statistical studies on multiple primary cancers including gastric cancers. Gan No Rinsho 1984;30(12 Suppl):1514-23.
24. Kim JW, Han JW, Jung SY, Jung JP, Kim JW. Synchronous double primary malignant tumor of the gallbladder and liver: a case report. World Journal of Surgical Oncology. 2011;9:84.
25. Iar?mov N, Toshev S, Angelov K, Lukanova Ts, Gribnev P, Sokolov M. Multiple primary carcinomas of the colon and associated extracolonic primary malignant tumors. Khirurgiia (Sofiia). 2007;(4):5-9.
26. Cercato M C, Colella E, Ferraresi V, Diodoro M G, Tonachella R. Report of two cases of quintuple primary malignancies and review of the literature. Anticancer research, 2008;28(5B):2953- 8.
27. Sommers, G. M., Logan, S., and Camel, H. M. Six independent neoplasms in one woman. A case report. The Journal of reproductive medicine, 1988;33(1):82-3.
28. Baigrie, R. J. Seven different primary cancers in a single patient. A case report and review of multiple primary malignant neoplasia. European journal of surgical oncology: the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology, 1991;17(1):81-3.
29. Cigna E, Gradilone A, Sorvillo V, Scuderi N. ABCB5 in peripheral blood of a patient affected by multiple primary malignancies. Ann. Ital. Chir, 2011;82(1):49-53.
30. Zhao J, Tan Y, Wu Y, Zhao W, Wu J, Ji M et al. A rare case of eight multiple primary malignant neoplasms in a female patient: A case report and review of the literature. Oncology Letters, 2015;9(2):587-90.
31. Weingartner K, Melekos MD, Gerharz EW, Kohl U, Neumann K, Riedmiller H. Multiple (five) synchronous primarymalignant neoplasms of dissimilar histogenesis including a malignant fibrous histiocytoma of the bladder. Inter Urol Nephrol 1995;27:157-66.
32. Yakushiji H, Mukai S, Matsukura S, Mukai S, Matsukura S Sato S et al: DNA mismatch repair deficiency in curatively resected sextuple primary cancers indifferent organs: a molecular case report. Cancer Lett 1999;142:17-22,
33. Sari R, Buyukberber S, Sevinc A, Mizrak B. Synchronous primary malignant neoplasms of colon and bladder. Indian J Gastroenterol. 2001;20(4):156-7.
34. Liu, Z., Chen, G., Zhu, Y., and Li, D. Simultaneous radical cystectomy and colorectal cancer resection for synchronous muscle invasive bladder cancer and cT3 colorectal cancer: Our initial experience in five patients. Journal of research in medical sciences: the official journal of Isfahan University of Medical Sciences, 2014;19(10):1012-5]
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License