IJCRR - 7(18), September, 2015
Pages: 38-40
Date of Publication: 20-Sep-2015
Print Article
Download XML Download PDF
MODIFIED SCHIRMER TEST SCREENING FOR DRY EYE DISEASE IN RURAL POPULATION
Author: Virendra Singh Lodha
Category: Healthcare
Abstract:Objective: The present study was undertaken to screen rural patients for dry eye disease by a modified Schirmer 1 test without anaesthesia with a cut off of 10 mm wetting of Schirmer test strip. Methods: Schirmer 1 test without anaesthesia was performed on 140 patients (65 males and 75 females) over 40 years of age from rural background after obtaining informed consent and after applying some exclusion criteria. The test was aborted as soon wetting of 10 mm of Schirmer test strip occurred and time noted. The patients who did not achieve 10 mm of wetting on Schirmer test over 5 minute's time were labelled Schirmer test positive. Results: The incidence of positive Schirmer1 test (without anaesthesia) was 16.4% in the studied group of 140 patients with a higher incidence in females over 50 years of age. Out of 140 patients screened, 63% patients achieved a wetting of 10 mm of Schirmer test strip in 2 or less than 2 minutes. Conclusion: Modified Schirmer 1 test (without anaesthesia) with a cut off limit of 10 mm can be a better option for dry eye disease screening in large volume based ophthalmic practice and eye camps as it reduces test time and causes less discomfort to the patient, and the procedure does not require any equipment other than readily available Schirmer test strips.
Keywords: Schirmer test, Dry eye disease
Full Text:
INTRODUCTION
Dry eye disease is a common ocular disorder affecting a significant percentage of population, estimated to be 5 - >30.1, 2 International Dry Eye Workshop (2007) defined dry eye as a multifactorial disease of tears and ocular surface that results in discomfort, visual disturbance and tear film instability with potential damage to the ocular surface and is accompanied by increased osmolarity of tear film and inflammation of ocular surface.3 The prevalence of dry eye disease is likely to increase in future due to increase in life expectancy, environmental pollution, increased use of medications, increased incidence of diabetes mellitus and life style changes. Dry eye disease results from either decreased tear production or increased evaporation of tears. Various methods used to diagnose dry eye disease include Schirmer test, Phenol Red Thread test, tear film break up time (TBUT),tear meniscus height, epithelial staining with rose Bengal and lissamine green, tear osmolarity, impression cytology and symptom questionnaires like ocular surface disease index (OSDI), dry eye questionnaire (DEQ) etc. Different tests have been shown to have different specificity and sensitivity. Tear osmolarity determination is the most reliable test to diagnose dry eye but is expensive to perform and time consuming. Only Schirmer test is one such test which is simple to perform and does not require slit lamp or other equipment and can be performed easily by a trained ophthalmic technician. Schirmer introduced the test in 1903(4) and since then it has been modified by many investigators of which Schirmer 1 test is the most popular of the variants and is carried out without anaesthesia, it measures both reflex and basal tear secretions.(5) In India rural people seek eye check up mostly in eye camps where they turn out in large numbers. The eye care professional has to examine large number of patients hence it becomes difficult to perform tests for dry eye disease which require more time, equipment and expensive. Hence the present study was undertaken to find out the prevalence of positive Schirmer 1 test in rural population, attending free outpatient services of the eye department of Pacific Medical College and Hospital, Udaipur.
MATERIALS AND METHODS
This study was conducted after obtaining approval from institutional ethics committee. After obtaining informed consent, a total of 140 patients from nearby villages, aged 40 years and above visiting eye department of Pacific Medical College and Hospital, Udaipur from September 2014 to December 2014 were included in the study. Exclusion criteria: Patients with history of any systemic disease, who were on any systemic medications (Allopathic, Ayurvedic, Homeopathic or Unani), history of eye surgery, on topical ocular medications, eye lid deformities, trichiasis, trachoma or other active ocular infection or inflammation, glaucoma, corneal opacities or degenerations and who were unwilling to undergo Schirmer test were excluded from this study. After performing routine ophthalmic examination which included visual acuity measurement, refraction, slit lamp examination and undilated fundus examination, Schirmer 1 test without anaesthesia was performed after explaining the procedure to the patient. Intra ocular pressure was recorded after performing Schirmer test and the patients with high intraocular pressure (>21) were not included in the study. Commercially available Schirmer test strips were used for the test. The test strip was inserted at the junction of medial two third and lateral one third of the lower conjunctival fornix of both eyes and the patient was instructed to keep eyes open, look straight and blink normally. The test strip was removed from the eye as soon as a wetting of 10 mm occurred and time noted. The patients whose wetting did not cross 10 mm mark at completion of 5 minutes were labelled as Schirmer 1 test positive.
RESULTS
Schirmer 1 test without anaesthesia was performed in 140 patients, 65 male and 75 female, table 1 shows age group wise distribution with maximum patients (67.85%) belonging to age group 40 – 50 years of age of which 11% males and 14% females were Schirmer 1 test positive. The incidence of positive Schirmer 1 test was 20% in the groups over 50 years of age in males. In female patients the incidence was 26.6% in the age group of 51 – 60 years and 30% in the age group of over 60 years with an incidence of 28% in the all females over 50 years of age.
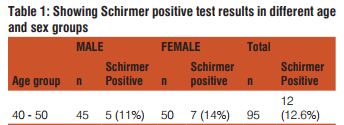
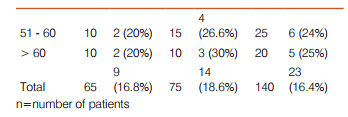
Table 2 shows that out of 117 Schirmer test negative patients, 88 (75%) required less than 2 or 2 minutes to achieve 10 mm wetting of the test strip (63% of total patients screened) and 29 patients (25%) required more than 2 minutes for 10 mm wetting to occur. It shows that only 37% patients including Schirmer test positive patients require the test to be continued for more than 2 minutes. None of the patients in this study complained of any ocular discomfort due to test procedure
DISCUSSION
Since its introduction in1903 by Schirmer6 , many variations of this test have been used clinically; especially test with closed or open eyes, with or without anaesthesia and type of paper and its strip size. Presently Schirmer 1 test without anaesthesia is the most popular test for measuring aqueous tear production with commercially available Schirmer test strips. To minimise ocular discomfort and increasing the co nvenience in performing the test in less time Nelson proposed to do it for 1- minute time with a cut off value of 6mm.7 Bawazeer and Hodge demonstrated that 1-minute test with anaesthesia correlated highly with the 5-minute test with anaesthesia.8 In the present study Schirmer 1 test without anaesthesia was performed to find out the incidence of positive Schirmer test with a 10 mm cut off (wetting of less than 10 mm in five minutes) and the incidence of negative Schirmer test to study the incidence of dry eye disease in rural population. The test was aborted as soon as 10 mm wetting of test strip occurred and time noted as 2 minutes or more. It was found that in the age group of 40-50 years the test was positive in 11% of males and 14% females with combined incidence of 12.6% in this group. In the age group of 51-60 years 20% males and 26.6% females were found to have positive Schirmer test (dry eye) with a combined incidence of 24% in this age group. In the age group of over 60 years 20% males and 30% females were found to be positive on Schirmer Test.
The overall incidence of dry eye in the present study was found to be 16.4%, with 13.8% in males and 18.6% in females wherein only Schirmer 1 test without anaesthesia and with a cut off value of 10 mm was used for the diagnosis in rural population. In studies done in northern and eastern India prevalence of dry eye disease in hospital based population is reported to be between 18.4% and 40.8% with different diagnostic criteria being used.9,10,11 The lower incidence in the present study may be due to the fact that only Schirmer test was used as a screening tool. In the present study Schirmer test was aborted before 5 minutes if a wetting of 10 mm occurred earlier. Out of 117 patients who were negative on Schirmer test (wetting of 10 mm) 88 patients (75%) required less than 2 minutes or less and 29 patients (25%) required more than 2 minutes and from a total of 140 patients tested 63% required less than or 2 minutes of the test time if it was aborted as soon as 10 mm wetting of the test strip occurred. Similar observation has been made in an earlier study and authors concluded that 2- Minute Schirmer 1 test with anaesthesia could be used instead of the standard 5-minute rest.12 However in Schirmer 1 test with anaesthesia reflex tear production cannot be ruled out hence the present study was done with Schirmer 1 test without anaesthesia.
CONCLUSION
From the results of this study it can be concluded that a modified Schirmer 1 test (without anaesthesia) with a cut off limit of 10 mm wetting of the test strip, reduces the test time significantly which is more convenient for both, the eye care professional and the patient, and hence can be a good tool for dry eye disease screening in large volume based ophthalmic practice or eye camps.
ACKNOWLEDGEMENTS
1. The author is thankful to the management of Pacific Medical College and Hospital, Udaipur, India for allowing me to conduct this study.
2. Author acknowledges the immense help received from the scholars whose articles are cited and included in references of this manuscript. The author is also grateful to authors / editors /publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
1. Smith JA, Albenz J, Beglet C et al. The epidemiology of dry eye disease: Report of the epidemiology subcommittee of the International Dry Eye Disease Workshop (2007), Ocul Surf. 2007, 5: 93–107.
2. Lemp MA, Advances in understanding and managing dry eye disease, Am J Ophthalmol. 2008 Sept; 146(3): 350–356.
3. International Dry eye Disease Workshop (DEWS). The definition and Classification and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye Workshop Ocul Surf. 2007, 5: 75–92.
4. Savini G, Prabhawasat P, Kozima T, Grueterich M, Espana E, Goto e. The challange of dry eye diagnosis. Clin Ophthalmol. 2008; 2(1):31–35.
5. Smith J, Nichols KK, Baldwin EK. Current patterns in the use of diagnostic tests in dry eye evaluation. Cornea. 2008; 27(6):656– 662.
6. Schirmer O. Studien zur physiologie und pathologie der tranenabsonderung Und tranenabfuhr. Graefes Arch Clin Exp Ophthalmol. 1903; 56:197–291.
7. Nelson PS. A shorter Schirmer tear test. Optom Mon. 1982; 73:568–9.
8. Bawazeer AM, Hodge WG. One-minute Shirmer test with anaeasthesia. Cornea. 2003; 22 (4): 285–287.
9. Sahai A, Malik P. Dry Eye:Prevalence and attributable risk factors in a Hospital based population. Ind J ophthal 2005; 53: 87– 91.
10. Gupta N, Prasad I, Jain R, D’Souza P. Estimating the prevalence of dry eye Indian patients attending tertiary ophthalmology clinic. Ann Trop Med Parasitol 2010; 104: 247–255.
11. Basak SK, Pal PP, Basak S, Bandhyopadhyay A, Choudhary S, Sar S. Prevalence of Dry Eye Diseases in hospital-based population in West Bengal, Eastern India. J Indian Med Assoc. 2012; 110: 789–794.
12. Suphakasem S, Lekskul M, Rangsin R. Assessment of different wetting time and paper strip size of Schirmer test in dry eye patients. J Med Assoc Thai 2012, 95 Suppl 5: S107–110.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License