IJCRR - 14(4), February, 2022
Pages: 40-44
Date of Publication: 15-Feb-2022
Print Article
Download XML Download PDF
An Update on Silver Diamine Fluoride and Its Use in Special Needs Individuals
Author: Kiran K, Bhargavi R Vojjala, Arshiya Shakir
Category: Healthcare
Abstract:Dental care was determined to be one of the most common unmet health care in Special needs patients. As special needs patients have certain limitations, routine dental treatment cannot be performed. Radical treatment modalities such as sedation or general anaesthesia are often required. However, these treatment modalities have their own risks. During recent times, there has been a revival in interest in using silver diamine fluoride to arrest dental caries. This review makes a case for using the silver fluoride bulletin special needs individuals to simplify the treatment procedure and make radical treatment modalities unnecessary.
Keywords: Cariostatic agents, Dental caries, Silver compounds, Silver diamine fluoride, Topical fluorides
Full Text:
INTRODUCTION
In the field of dentistry, special needs patients are individuals who present with physical, sensory, mental, growth medical limitations, whether they are transitory or permanent.Due to their limitations, these individuals need differentiated dental treatment.1 The US Maternal and Child Health Bureau stated that Children with Special Health Care Needs (CSHCN) are “those who have or are at increased risk for a chronic physical, developmental, behavioural, or emotional condition and who also require health and related services of a type or amount beyond that required by children generally”.2 Special Care Dentistry (SCD) is concerned with providing and enabling the delivery of oral care for people with an impairment or disability.3
According to the World Health Organization (WHO), nearly 600 million persons around the world or 1 in every 10 persons have some form of disability.4 In the United States, nearly 15 million children or 1 in 5 children have special health care needs.5 In India, a total of 2.21% of the population or 2.68 Crore persons are disabled. The prevalence of disability is highest in the age group 10-19 years. It consists of 46.2 lakhs persons and makes up 17% of the total disabled population.6
Informally collected evidence suggested that CSHCN are at increased risk for poor oral health.7 Dental care was determined to be the most common unmet health care need for these children.8,9 Several factors are associated with the unmet dental care needs. These factors encompass the difficulties associated with the treatment. CSHCN often require advanced pharmacologic behaviour guidance modalities such as sedation or general anaesthesia. These modalities are not always available and have risks inclusive of effects on brain development in young children and mortality.10
Due to the hurdles expected during the treatment of CSHCN, an agent which is capable of preventing and limiting the damage and discomfort caused by dental caries is required. In turn, this agent will constrain the difficulties associated with more radical treatment modalities. One such agent is silver diamine fluoride (SDF). Though not new, the solution has recently been in the limelight. Clinicians throughout the world have been showing interest in SDF due to its effectiveness in arresting the progression of carious lesions.11,12
However, even with global acceptance, very few articles have explained the use of SDF in individuals with special needs. This update attempts to encourage the use of SDF in these individuals to provide for their unmet dental needs and improve their health and quality of life.
SILVER DIAMINE FLUORIDE
SDF is a clear, colourless, odourless solution of silver, fluoride and ammonium ions. It is also known as Ammoniated Silver Fluoride, Ammoniacal Silver Fluoride, Silver Ammonium Fluoride, Silver Fluoride Diamine, Diamine Silver Fluoride, Silver Diamine Fluoride, Diamine Silver Fluoride, Silver Fluoride.13-17 Additionally, due to its hypothesized ability to halt the caries process and simultaneously prevent the formation of new caries, it is referred to as “silver fluoride bullet”. 18
In 1917, Percy Howe was the first to add ammonia to silver nitrate and prepare a solution that became known as “Howe’s solution” (ammoniacal silver nitrate).18 This solution was used to arrest caries for the next 50 yrs. This initial combination acted as the backbone for the formation of silver diamine fluoride solution.
In 1969, Nishino was the first to study Silver diamine fluoride at Osaka University in Japan. Later, The Central Pharmaceutical Council of the Ministry of Health and Welfare of Japan approved “Diamine silver fluoride” for caries prevention.19 The solution was marketed as Saforide solution (Toyo Seiyaku Kasei Co. Ltd, Osaka, Japan).20,21,22 Since then, more than four decades have witnessed the effective use of SDF as a preventive material.
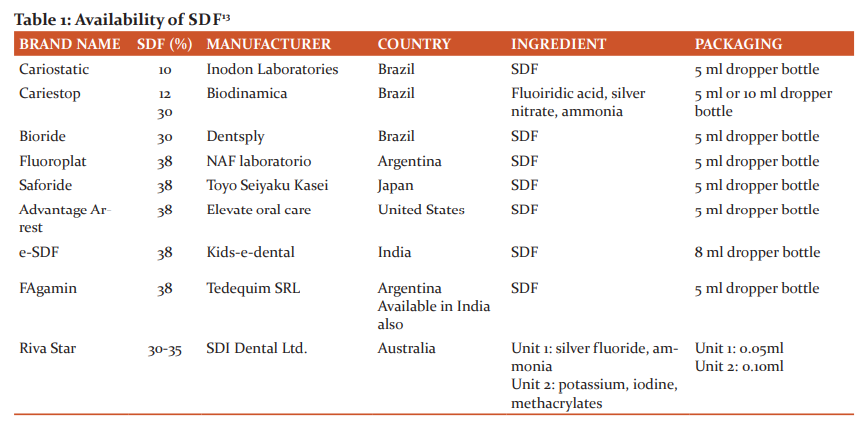
In August 2014, The U.S. Food and Drug Administration (FDA) gave clearance to SDF for dental use in the United States.23 The solution is available as a 38% concentration comprising of 24.4–28.8% (w/v) silver and 5.0–5.9% fluoride, at pH 10, and marketed as Advantage Arrest by Elevate Oral Care, LLC, West Palm Beach, Florida. Currently, SDF is marketed in different concentrations across the globe. Table 1 summarizes its availability.13,14
Mechanism of Action:
The mechanisms by which SDF arrests and/or prevents dental caries are:
Obturation of dentinal tubules:
When applied topically, a squamous layer of silver protein conjugate is formed on the exposed dentinal area. The dentinal tubules are partially plugged and there is increased resistance to acid dissolution and enzymatic digestion. Hydroxyapatite, fluorapatite, silver chloride, and metallic silver form a protective layer on the exposed organic matrix.25,26
Anti-microbial action of silver:
Silver ions act directly against bacteria by breaking membranes, denaturing proteins, and inhibiting DNA replication.24
Additionally, silver present in the SDF solution is reactivated when the dead bacteria (bacteria killed by silver ions) are added to the living bacteria. This reactivated silver again effectively kills the living bacteria. The dead bacteria act as a reservoir and show biocidal activity towards the viable bacterial population. This reservoir effect helps explain why silver deposited on bacteria and dentin proteins within a cavity has sustained antimicrobial effects. This concept of the dead bacteria killing the living bacteria is called as the “zombie effect”.27
Cariostatic action mediated by fluorapatite
Remineralisation of the demineralised inorganic tooth mineral is supported by the fluoride ions in SDF. Fluorapatite, silver phosphate and calcium fluoride are formed. They produce a surface more resistant to acid dissolution.28
Anti-enzymatic action on organic component
Silver diamine fluoride specifically inhibits the proteins that break down the exposed dentine organic matrix.29 These include matrix metalloproteinases, cathepsins, and bacterial collagenases.30
DISCUSSION:
SDF can be used in a variety of clinical conditions. It can be used in cases of active cavitated dental carious lesions, carious lesions which may not be treated in one visit, and extensive lesions which need to be temporarily controlled due to the presence of external factors (such as financial restraints) which do not allow for completion of treatment.26 Later, the arrested lesions can be restored via Silver Modified Atraumatic Restorative Technique (SMART).
All these indications, suggest the SDF can be a great alternative for the treatment of untreated decay in young children. In case of CHSCN, caregivers reported higher unmet dental care needs when compared with their medically unremarkable peers. 31-33 A National Survey conducted in 2007 on CSHCN stated that 22.8% of caregivers reported presence of cavities in the previous 6 months in children younger than 18 years.34 In addition, about 15% to 18.7% of caregivers reported that their child had toothache in the previous 6 months.35
SDF can also be used in conditions where traditional restorations fail to stop disease progression and caries risk is extremely high. The “zombie effect” mentioned earlier may help to restrict the carious process in such circumstances. These conditions include severe early childhood caries, recurrent caries, and xerostomia.
Xerostomia can be a frequent oral health concern for special needs individuals. Potential causes of xerostomia include mouth breathing, dehydration, medications such as anticholinergics, antidepressants, antipsychotic agents, diuretics, antihypertensive drugs, sedatives, anxiolytics, muscle relaxants, analgesics (opioids and nonsteroidal anti-inflammatories), bronchodilators, and antihistamines. Other causes include salivary gland disorders, malignancies or other medical conditions affecting salivation. 36,37 These potential risk factors are more common in paediatric patients with special needs. Thus, application of diamine silver fluoride can be considered as a treatment modality for these patients.
Another important indication is in treatment of behaviourally or medically challenged individuals. These include uncooperative children, pre-cooperative children, those with severe cognitive or physical disabilities, and patients with dental phobias. CSHCN patients may fall into one or more of these categories, thereby justifying the application of SDF.
In addition to all these scenarios, SDF can also be used as a desensitizer and improve hypersensitivity symptoms within 24 hours. Studies have reported a significant number of children and adults with special needs experience tooth sensitivity.38,39 These individuals can be treated with SDF.
However, the versatile nature of SDF which allows for it to be used in numerous clinical situations should not be the only reason for clinicians to consider its use. Several other advantages also make it an exceptional treatment modality. These advantages include affordability (cost per pennies), simplicity of application, and non-invasive nature.19
Research has stated the reasons for increased unmet dental needs in CSHCN include living in low-income households or rural area, failure to receive medical care, increased special needs severity and lower degree of functioning, poor psychological adjustment, caregiver burden, not having a personal dentist, lack of preventive medical care, and the absence of coordination among community-based organizations.7,40-43 All of these reasons can be countered by the above-mentioned benefits of diamine silver fluoride.
Furthermore, no serious adverse events, inclusive of allergic reactions, toxicity or pulpal irritations have been reported by any randomised control trial till date. Gingival reactions and chemical burns to skin were rare too. SDF is also safe even when applied to several carious lesions at the same visit, in terms of the pharmacokinetics of the solution.24 Thus, while using SDF, the clinician can be rest assured.
Unfortunately, this “silver fluoride bullet” is not without disadvantages. It does not restore form and function to teeth as do other restorative procedures. Therefore, it can only be used as an adjunct to restorative therapy.44 In addition, it has a transient metallic or bitter taste, and causes dark discoloration. The staining is more of a concern when SDF is applied in the aesthetic zones.45,46,47 Studies have shown that parents have concerns in relation to the staining of the teeth but prefer SDF over other more radical options such as general anaesthesia for treatment.48,49 Thus, it can be stated that the undesirable effects caused by the solution are outweighed by its desirable properties.10
CONCLUSION:
Silver diamine fluoride is a simple, safe, cost-effective, and efficient topical solution that can be used for treating dental caries. The solution is readily available throughout the world. Its easy application makes the solution a go-to therapeutic, especially in case of behaviourally or medically challenged patients.50
These inherent properties of SDF suggest that it possesses significant potential in treatment of CSHCN. SDF will allow for the dental needs of special needs individuals to be met and improve their quality of life. However, limited research has been conducted on CSHCN and the suggestions made by this article are based on it. Hence, we recommend that further high-quality, systematic, condition-specific epidemiologic studies be performed with regard to CSHCN.
CONFLICTS OF INTEREST: No conflicts of interest.
SOURCE OF FUNDING: Nil
ACKNOWLEDGEMENTS: Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
AUTHORS’ CONTRIBUTION:
Author 1: Concept and Design off Article, Manuscript Editing, Manuscript Review
Author 2: Literature Search, Manuscript Preparation, Manuscript Editing
Author 3: Definition of Intellectual Content, Manuscript Review
References:
-
Gavina VP, Alves NS, Alves FR, Cortellazzi KL, Silveira FM, Assaf AV. Oral Health for Patients with Special Needs: Evaluative Research of the Dental Specialties Centers. Port J Public Health. 2018;36(2):81-94.
-
McPherson M, Arango P, Fox H, Lauver C, McManus M, Newacheck PW et al. A new definition of children with special health care needs. Pediatrics. 1998; 102:137–40.
-
Dougall A, Fiske J. Access to special care dentistry, part 1. Access. Br Dent J. 2008; 204, 605-16.
-
Petersen PE. The World Oral Health Report 2003: continuous improvement of oral health in the 21st century-the approach of the WHO Global Oral Health Program. Community Dent. Oral Epidemiol. 2003; 31: 3-24.
-
Child and Adolescent Health Measurement Initiative (CAHMI). Who are children with special health care needs (CSHCN). Data Resource Center for Child and Adolescent Health. Available at: http://childhealthdata.org/. Accessed February 22, 2020.
-
Social Statistics Division. Ministry of Statistics Programme Implementation. Government of India. Disabled persons in India-a statistical profile 2016. http://mospi.nic.in/sites/default/files/publication_reports/Disabled_persons_in_India_2016.pdf. Accessed February 22, 2020.
-
Chi DL. Oral health for US children with special health care needs.Pediatr Clin North Am. 2018; 65(5):981-93.
-
Newacheck PW, Hughes DC, Hung YY. The unmet health needs of America’s children. Pediatrics. 2000; 105:989–97.
-
Lewis CW. Dental care and children with special health care needs: a population based perspective. Acad Pediatr. 2009; 9(6):420–26
-
Crystal YO, Marghalani AA, Ureles SD, Wright JT, Sulyanto R, Divaris K et al. Use of silver diamine fluoride for dental caries management in children and adolescents, including those with special health care needs. Pediatr Dent. 2017; 39(5):135E-45E.
-
Gao SS, Zhang S, Mei ML, Lo Chin-Man E, Chu C-H. Caries remineralisation and arresting effect in children by professionally applied fluoride treatment—a systematic review. BMC Oral Health. 2016; 16:12.
-
Oliveira BH, Rajendra A, Veitz-Keenan A, Neiderman R. The effect of silver diamine fluoride in preventing caries in the primary dentition: a systematic review and meta-analysis. Caries Res. 2019;53(1):24–32.
-
Nuvvula S, Mallineni SK. Silver Diamine Fluoride in Pediatric Dentistry. J South Asian Assoc Pediatr Dent. 2019;2(2):73–80.
-
Mei ML, Lo EC, Chu CH. Clinical use of silver diamine fluoride in dental treatment. CompendContin Educ Dent. 2016 Feb 1;37(2):93-8.
-
Horst JA, Tanzer JM, Milgrom PM. Fluorides and Other Preventive Strategies for Tooth Decay. Dent Clin North Am. 2018;62(2):207-34.
-
Craig GG, McIntyre JM. Clinical evaluation of diamine silver fluoride/potassium iodide as a dentine desensitizing agent. A pilot study. Aust Dent J. 2012;57(3):308-11.
-
Yamaga R, Nishino M, Yoshida S, Yokomizo I. Diammine silver fluoride and its clinical application. J Osaka Univ Dent Sch. 1972; 12:1-20.
-
Knight GM, McIntyre JM, Craig GG, Mulyani, Zilm PS, Gully NJ. Differences between normal and demineralized dentineepretreated with silver fluoride and potassium iodide after an in vitro challenge by Streptococcus mutans. Aust Dent J. 2007;52(1):16-21.
-
Rosenblatt A, Stamford TCM, and Niederman R. Silver diamine Fluoride: A Caries “Silver-Fluoride Bullet. J Dent Res. 2009; 88(2):116-25.
-
Nishino M, Yoshida S, Sobue S, Kato J, Nishida M. Effect of topically applied ammoniacal silver fluoride on dental caries in children. J Osaka Univ Dent Sch. 1969; 9:149–55.
-
Yamaga R, Nishino M, Yoshida S, Yokomizo I. Diamine silver fluoride and its clinical application. J Osaka Univ Dent Sch. 1972; 12:1–20.
-
Shah S, Bhaskar V, Venkatraghavan K, Choudhary P, Trivedi K. Silver diamine fluoride: a review and current applications. J. Adv. Oral Res. 2014; 5(1):25-35.
-
Crystal YO, Niederman R. Evidence-based dentistry update on silver diamine fluoride. Dent. Clin. N. Am. 2019; 63(1):45-68.
-
Seifo N, Robertson M, MacLean J, Blain K, Grosse S, Milne R et al. The use of silver diamine fluoride (SDF) in dental practice. Br. Dent. J. 2020; 228(2):75-81.
-
Mei ML, Ito L, Cao Y, Li QL, Lo EC, Chu CH. Inhibitory effect of silver diamine fluoride on dentine demineralisation and collagen degradation. J Dent. 2013; 41(9):809-17
-
Horst JA, Ellenikiotis H, Milgrom PL. UCSF Protocol for Caries Arrest Using Silver Diamine Fluoride: Rationale, Indications and Consent. J Calif Dent Assoc. 2016; 44(1):16-28.
-
Wakshlak R B-K, Pedahzur R, Avnir D. Antibacterial activity of silver-killed bacteria: The” zombies” effect. Sci Rep. 2015; 5: 9555.
-
Zhao I S, Gao S S, Hiraishi N, Burrow MF, Duangthip D, Mei ML et al. Mechanisms of silver diamine fluoride on arresting caries: A literature review. Int Dent J. 2018; 68: 67–76.
-
Chaussain-Miller C, Fioretti F, Goldberg M, Menashi S. The role of matrix metalloproteinases (MMPs) in human caries. J Dent Res. 2006; 85: 22–32.
-
Mei M L, Li Q L, Chu C H, Yiu C K, Lo EC. The inhibitory effects of silver diamine fluoride at different concentrations on matrix metalloproteinases. Dent Mater. 2012; 28: 903–08.
-
Nelson LP, Getzin A, Graham D, Zhou J, Wagle EM, McQuiston J et al. Unmet dental needs and barriers to care for children with significant special health care needs. Pediatr Dent. 2011; 33(1): 29–36.
-
Paschal AM, Wilroy JD, Hawley SR. Unmet needs for dental care in children with special health care needs. Prev Med Rep. 2015; 3:62–7.
-
McManus BM, Chi D, Carle A. State Medicaid eligibility criteria and unmet preventive dental care need for CSHCN. Matern Child Health J. 2016; 20(2):456–65.
-
Wiener RC. Children with special health care need’s association of passive tobacco smoke exposure and dental caries: 2007 National Survey of Children’s Health. J PsycholAbnorm Child. 2013; 2: 1
-
Lewis C, Stout J. Toothache in US children. Arch Pediatr Adolesc Med. 2010; 164(11):1059–63.
-
Walsh LJ. Dry mouth: a clinical problem for children and young adults. Int Dent SA. 2007; 9:48–58.
-
Guggenheimer J, Moore PA. Xerostomia: etiology, recognition and treatment. J Am Dent Assoc. 2003; 134:61–9.
-
John JR, Daniel B, Paneerselvam D, Rajendran G. Prevalence of dental caries, oral hygiene knowledge, status, and practices among visually impaired individuals in Chennai, Tamil Nadu. Int J Dent. 2017
-
Mohd-Dom TN, Omar R, Malik NA, Saiman K, Rahmat NA. Self-reported oral hygiene practices and periodontal status of visually impaired adults. Glob J Health Sci. 2010; 2(2):184-91.
-
Skinner AC, Slifkin RT, Mayer ML. The effect of rural residence on dental unmet need for children with special health care needs. J Rural Health 2006; 22(1): 36–42.
-
Kane D, Mosca N, Zotti M, Schwalberg R. Factors associated with access to dental care for children with special health care needs. J Am Dent Assoc 2008; 139(3):326–33.
-
Iida H, Lewis C, Zhou C, Novak L, Grembowski D. Dental care needs, use and expenditures among U.S. children with and without special health care needs. J Am Dent Assoc 2010; 141(1):79–88.
-
Gaskin DJ, Mitchell JM. Health status and access to care for children with special health care needs. J Ment Health Policy Econ 2005; 8(1):29–35.
-
Davis MR, Johnson EL, Meyer BD. Comparing dental treatment between children receiving and not receiving silver diamine fluoride. Int. J. Clin. Pediatr. Dent. 2020;44(6):400-6.
-
Alshammari AF, Almuqrin AA, Aldakhil AM, Alshammari BH, Lopez JNJ. Parental perceptions and acceptance of silver diamine fluoride treatment in Kingdom of Saudi Arabia. Int J Health Sci. 2019;13(2):25-29.
-
Bagher SM, Sabbagh HJ, AlJohani SM, Alharbi G, Aldajani M, Elkhodary H. Parental acceptance of the utilization of silver diamine fluoride on their child's primary and permanent teeth. Patient Prefer Adherence. 2019; 13:829-35.
-
Magno MB, Silva LP, Ferreira DM, Barja?Fidalgo F, Fonseca?Gonçalves A. Aesthetic perception, acceptability and satisfaction in the treatment of caries lesions with silver diamine fluoride: a scoping review. Int. J. Clin. Pediatr. Dent.. 2019 May;29(3):257-66.
-
Crystal YO, Janal MN, Hamilton DS, Niederman R. Parental perceptions and acceptance of silver diamine fluoride staining. J Am Dent Assoc. 2017; 148(7):510-18.
-
Hu S, Meyer B, Lai BW, Chay PL, Tong HJ. Parental acceptance of silver diammine fluoride in children with an autism spectrum disorder. Int. J. Paediatr. Dent. 2020; 30(4):514-22.
-
Wright JT, White A. Silver diamine fluoride: changing the caries management paradigm and potential societal impact. North Carolina medical journal. 2017 Nov 1;78(6):394-7.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License