IJCRR - 14(3), February, 2022
Pages: 63-66
Date of Publication: 01-Feb-2022
Print Article
Download XML Download PDF
Ovarian Pregnancy in Kindu City, D.R. Congo - A Case Report
Author: Mbungu Mulaila AP, Mbungu Mwimba R., Mbanzulu Pita NZ, Ambambula Yalala O., Okamba Alangi T., Kahindo P. Muyayalo
Category: Healthcare
Abstract:Introduction: Ovarian pregnancy (OP) is an uncommon form of ectopic pregnancy that is often misdiagnosed. However, the rupture of the expanding OP can lead to internal bleeding and threaten women life. The purpose of this case report is to discuss the challenge to diagnosing and managing OP, specifically in low-income countries, accurately. Case Report: We report the case of an ectopic pregnancy suspected as being an abdominal pregnancy with a dead fetus in utero on ultrasound and which turned out to be ovarian, discovered intraoperatively in a 22-year-old third parous without known morbid history. Discussion: Due to its rarity, OP remains an isolated and exceptional phenomenon in a woman's life. OP is difficult to diagnose and sometimes lately diagnosed, especially in countries with limited resources as the Democratic Republic of Congo (DRC). Indeed, the lack of adequate imaging and histopathologic equipment, and qualified practitioners in most medical centers do not facilitate the early diagnosis and treatment of OP in those settings. Conclusion: This first reported case of OP in the D.R. Congo confirms the difficulty in making the diagnosis. In case of diagnosis doubts, medical care practitioners should consider directing patients to specialized health care cente
Keywords: Ectopic pregnancy, Ovarian pregnancy, Case report, Mapon Clinic, Kindu City, D.R. Congo
Full Text:
INTRODUCTION
The most commonly occurring gynecologic emergency leading to maternal death in the first trimester of pregnancy,1 ectopic pregnancy (EP), is a complication of pregnancy in which an embryo attaches itself anywhere outside of the uterus.2The large majority of EP (95 %) are located at the fallopian tubes; the remain 5 % are located in the abdomen, ovary, and cervix.1
Ovarian pregnancy (OP) is an uncommon form of ectopic pregnancy with an incidence of 0.5-3% of all ectopic gestations3, which occurs when a fertilized ovum implants on the surface of the ovary.4OP are often misdiagnosed as corpus luteum hemorrhage, and around 75% terminate in first trimester5. Indeed, the rupture of the expanding OP is expected at the early stage of pregnancy1, which can lead to internal bleeding and hypovolemic shock.4
Despite the availability of sophisticated diagnostic technology, the diagnosis of OP remains a challenge. Patients most often undergo surgery for suspected tubal ectopic pregnancy or hemorrhagic corpus luteum.6 Here we report the case of an ectopic pregnancy suspected as being an abdominal presenting as missed abortion on ultrasound, which turned out to be an OP during surgery, diagnosed at the Lumbulumbu Hospital Center (LLHC) / Mapon Clinic of Kindu in Maniema in the Democratic Republic of the Congo (DRC).
CASE REPORT
A 22-year-old gravida 3, para 3 was admitted at the LLHC / Mapon Clinic for lower abdominal pain, vaginal bleeding, and absence of active fetal movements (AFM). She did not have any history of pelvic inflammatory disease or insertion of an intrauterine device (IUD). She saw her last period on December 2th 2019, and 6 weeks later, she did the first ultrasound that confirmed the pregnancy without mentioning its location. The occurrence of vaginal bleeding (or spotting) at around 15 weeks of amenorrhea motivated her consultation in another medical center of the Kindu City. She received treatment for a threatened miscarriage that stopped the bleeding.
The recurrency of vaginal bleeding at around 19 weeks of amenorrhea and the absence of AFM let the patients to consult in another medical center of Kindu City different from the previous one, where ultrasound realized by unqualified practitioners reported an aseptic necrobiosis of a uterine fibroid without mentioning pregnancy. Then, the patient was referred for better management by specialists at the LLHC / Mapon Clinic.
At the time of her presentation at LLHC / Mapon Clinic, the gestational age was estimated at 28 weeks of amenorrhea. She complained of vaginal bleeding(spotting), intermittent lower abdominal pain, and the absence of AFM. She was in good general condition on examination, with moderately colored eyelid conjunctiva and good vital signs. The breasts were symmetrical, flabby, secreting breast milk. On abdominal examination, we observed a hypogastric arch eccentric to the left, going up to a finger gap below the umbilicus. Two distinct, poorly over conscribed, non-sensitive masses of more or less firm consistency, with irregular surfaces, were palpated in the right para-uterine side. One small and mobile mass to the two planes of the abdominal wall, and the other more significant still. In the left para-uterine side, we notice a tenderness on the deep palpation. The vulva was eutrophic and clean. The speculum examination revealed a healthy cervix pauciparous without ex-utero hemorrhage. On digital vaginal examination, the cervix was posterior, soft, long, closed. The uterus was enlarged about the size of an orange; the pelvis was considered clinically good. In addition, she did not present edema of the lower limbs.
Given the patient's history and the clinical examination, we suspected an aborted pregnancy; and uterine myomatosis was excluded.
Laboratory Investigations revealed Blood-Rhesus Group: B +; Hemoglobin (Hb): 12.4g / dl; Hematocrit (Ht): 38%; Red blood cells (RBCs) count: 4,460,000 / mm3; White Blood Cell (WBCs) Count: 5300 / mm3 (Neutrophils 44%, Lymphocytes 52%, Eosinophils 2%, Basophils 1%, and monocytes 1%); Platelets: 288000 / mm3; HIV serology negative.
Abdominopelvic ultrasound showed a left para-uterine abdominal pregnancy with a dead fetus in utero whose gestational age was 20 weeks ultrasound (femoral length: 33mm). The empty uterus having measured 98x46x67 mm, the left ovary not visualized, the right ovary with normal echo anatomy measuring 32x25x17 mm.
Based on all the above examinations (clinical, laboratory, and ultrasound), we decided to perform an exploratory laparotomy for arrested abdominal pregnancy.
The surgery was performed under general anesthesia. After median sub-umbilical coeliotomy, we made the following observations: a peritoneal fluid tinted with old blood estimated at 150ml after aspiration. An old sizeable septate blood clot in the omentum weighed 170g. A pelvic mass of firm consistency, irregular surface, poorly mobilized, at the expense of the left ovary and firmly adhering to the ipsilateral tube, filling the Douglas sac and pushing back the uterus to the right (Figure 1). The mass had no contact with the intestinal loops or omentum (Figure 1). There was a clear cleavage line between the mass and the posterolateral part of the uterus that served as a surgical approach to removing the pelvic mass. The right tube and ovary were normal in appearance and volume.
We performed the right total adnexectomy, removing the mass that was fixed by the left utero-ovarian and lumbo-ovarian ligaments (Figure 1). The mass contained a female fetus with overlapping skull bones (Figure 2), first-degree macerated, weighing 457g (Figure 2). We then performed hemostasis, cleaned the peritoneal cavity with 3 liters of warm 0.9% Nacl, and placed a sentinel drain in the Douglas pouch. Finally, we closed the abdominal wall plan by plan and ended with a clean and dry bandage. There weren't any incidents during the surgery, and the postoperative follow-up was simple. The patient was discharged from the hospital on postoperative day five.
DISCUSSION
OP is a rare entity among ectopic pregnancies. Its diagnosis and management are not always easy. Its frequency is estimated at 2-3% of GEUs, representing an incidence of approximately 1/2500 to 1/5000 births.7 Sergeant et al. 8 found an incidence of 1 per 1400 births. It should be noted that the lowest Incidence was reported in Tunis with 1/21439 births.9 In the D.R. Congo, no incidence is available as this is the first reported case of OP.
In their series, Reithmeller et al.10 reported two cases of OP in older infertile women without an IUD. Similar to the findings of Beugre N. et al.11 in Ivory coast, our patient was younger and fertile. This difference might be related to the fact that the sample is unrepresentative, making it impossible to draw any possible conclusions to be extrapolated.
Clinically, abdominal pain, delayed menstruation, and bleeding are often presented.12,13 The pain corresponds to the rupture of the ovarian capsule by the OG and the formation of the hemoperitoneum.8,14 Patients are most often seen in an emergency setting, with significant hemoperitoneum or even in a state of hypovolemic shock.14 However, in our case, the patient was hemodynamically stable with no worsening of other symptoms. This would be justified by the possible existence of a polymorphism of the clinical pictures, resulting in a possible delay in the management when the symptoms are not acute.
According to Spiegelberg15, OP is characterized by its usual occurrence in the right side since 1) the average size of the right ovary (16mmx19mm) is much smaller than that of the left ovary (35mmx18mm); 2) part of the parenchyma of the right ovary often turns into a cystic cavity; 3) the wall of this cavity and the ovary have the same histological structure, in this cavity, we usually find fetal remains and placental remains.15,16
Many authors report that OP is diagnosed before 12 gestational weeks8, and some may progress until the 2nd trimester12 or even more. Danish et al. reported a case of a 32 gestational weeks OP that was diagnosed as an abdominal pregnancy before surgery, but during laparotomy, the diagnosis of GO was made.17 Because of the qualified medical practitioners and adequate equipment, our patient's diagnosis and management were delays (around 33 weeks of amenorrhea). Indeed, the patient visited several medical centers in the city without getting an accurate diagnosis. This case highlights the importance for medical care providers of recognizing their limits (in terms of skills and equipment) and better orient patients by transferring them to specialized structures when they are available in the environment.
CONCLUSION
Ovarian pregnancy is rare and can be associated with high morbidity and mortality rates. Sometimes the clinical presentation is confusing with threatened abortion or simply premature delivery. Despite the progress of medical treatment, its management remains surgical by laparoscopic route when the diagnosis is made early. The lack of adequate equipment and qualified personnel in many health care’s structures in countries with limited resources causes late consultations of pregnant women, often in severe conditions and sometimes fatal states. This first reported case of OP in the D.R. Congo confirms that the diagnosis of OP is still a dilemma. Therefore, when faced with diagnostic difficulties and doubts, the medical care practitioner should consider directing patients to specialized health care centers to improve their prognosis.
ACKNOWLEDGEMENTS
Authors acknowledge the immense help received from the scholars whose articles are cited and included in the references of this manuscript. The authors are also grateful to the authors /editors/publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
Ethical approval
Ethical committee of the Faculty of Medicine in the University of Kindu approved this case study. Informed consent was taken from the patient.
Source of Funding: None
Conflict of interest: None
AUTHORS’CONTRIBUTION:
Mbungu Mulaila AP.: diagnostic, therapeutic management and follow-up of the patient, writing - original draft and literature review. Ambambula Yalala O. and Okamba Al a ngi T.: diagnostic and therapeutic management of the patient. Mbungu Mwimba R., Mbanzulu Pita NZ, and Kahindo P. Muyayalo: supervision, validation, writing - original draft, writing - review editing. All authors also declare that they have read and approved the final version of the manuscript.
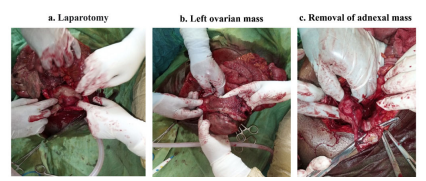
Figure 1: Left adnexal mass found during abdominal surgery. By surgical incision into the abdominal cavity (laparotomy), we came directly across a large clot made from old blood. This clot was covered with omentum and did not adhere to any intra-abdominal organs (fig 1a). The pelvic exploration revealed a large ovarian mass intimately adhered to the left fallopian tube and well-buried towards Douglas' cul-de-sac (fig 1b). After careful manual and instrumental adhesiolysis, we had exteriorized the mass and proceeded to the left total adnexectomy (fig 1c).
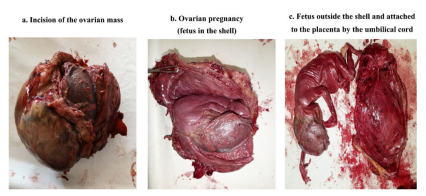
Figure 2: Female fetus with overlapping skull bones discovered after incision of the ovarian mass. The incision of the ovarian mass (fig 2a) let us observe the entire ovarian pregnancy made of a shell in which we saw a part of the fetal head (fig. 2b). The shell dissection allowed the externalization of a female fetus attached to the placenta by its umbilical cord (fig 2 C).
References:
1. Kadau JV. Sonographic Detection of Ovarian Ectopic Pregnanc
: A Case Study. J Diagn Med Sonogr. 2016;32(5):299-303.
2. Sotelo C. Ovarian Ectopic Pregnancy: A Clinical Analysis. J Nurse Pract. 2019;15(3):224-227.
3. Raziel A, Golan A, Pansky M, Ron-El R, Bukovsky I, Caspi E. Ovarian pregnancy: a report of twenty cases in one institution. Am J Obstet Gynecol.1990;163(4 Pt 1):1182-1185.
4. Birge O, Erkan MM, Ozbey EG, Arslan D. Medical management of an ovarian ectopic pregnancy: a case report. J Med Case Rep. 2015;9:290.
5. Goyal LD, Tondon R, Goel P, Sehgal A. Ovarian ectopic pregnancy: A 10 years' experience and review of literature. Iran J Reprod Med. 2014;12(12):825-830.
6. Gupta N, Gupta A, Onyema G, Pantofel Y, Ying SC, Garon JE, et al. Accurate Preoperative Diagnosis of Ovarian Pregnancy with Transvaginal Scan. Case Reports in Obstetrics and Gynecology.2012;2012:934571.
7. Job-Spira N, Coste J, Aublet-Cuvelier B, Germain E, Fernandez H, Bouyer J, et al. [Incidence of extra-uterine pregnancy and characteristics of treated patients. First results of the Auvergne registry]. Presse Med. 1995;24(7):351-355.
8. Sergent F, Mauger-Tinlot F, Gravier A, Verspyck E, Marpeau L. Grossesses ovariennes : réévaluation des critères diagnostiques J Gynecol Obstet Biol Reprod 2002;31(8):741-746.
9. Picaud A, Ella Edogha R, Ozouaki F, Nlome-Nze AR, Faye A, Ogowet-Igumu N, et al. Grossesse abdominale: à propos de 11 cas. Méd d'Afrique Noire. 1990;37(8/9):483-487.
10. Riethmuller D, Sautiere JL, Benoit S, Roth P, Schaal JP, Maillet R. [Ultrasonic diagnosis and laparoscopic treatment of an ovarian pregnancy. A case report and review of the literature]. J Gynecol Obstet Biol Reprod (Paris).1996;25(4):378-383.
11. Beugre NJ, Kouakou F. Etude épidémiologique et anatomo-pathologique des grossesses extra-utérines : à propos de 59 cas.Abidjan, Ivory Coast: Faculty of Medicine, FELIX HOUPHOUET-BOIGNY 1993.
12. Grimes HG, Nosal RA, Gallagher JC. Ovarian pregnancy: a series of 24 cases. Obstet Gynecol. 1983;61(2):174-180.
13. Cabero A, Laso E, Lain JM, Manas C, Escribano I, Calaf J. Increasing incidence of ovarian pregnancy. Eur J Obstet Gynecol Reprod Biol. 1989;31(3):227-232.
14. Ercal T, Cinar O, Mumcu A, Lacin S, Ozer E. Ovarian pregnancy; relationship to an intrauterine device. Aust N Z J Obstet Gynaecol. 1997;37(3):362-364.
15. O. S. Zur Kasuistik der Ovarialschwangerchaft. Arch Gynaekol1878(13):73–19.
16. Ranaivoson HV, Ranaivomanana VF, Nomenjanahary L, Andriamampionona TF, Randrianjafisamindrakotroka NS. [Ovarian pregnancy: about 3 cases and review of the literature]. Pan Afr Med J.2016;25:128.
17. Dane B, Dane C, Yayla M, Çetin A, Dural S, Tarlac A. An Ovarian Pregnancy with Delivery of a Live Infant. Perinatal Journal 2005;3:125-127.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License