IJCRR - 14(2), January, 2022
Pages: 54-59
Date of Publication: 16-Jan-2022
Print Article
Download XML Download PDF
A Prospective Study of Risk Malignancy Index in Adnexal Masses
Author: Neha Kumari, Mamta Singh
Category: Healthcare
Abstract:This scoring system is based on serum CA-125, menopausal status, ultrasonographicfinding. This scoring method yield much better results than individual parameters. Methods: Present study conducted between July 2017 to June 2019.Parameter like menopausal status, ultrasoundfeatures, and serum level of tumor marker like CA-125 for calculating RMI 3. Then RMI was compared with the histopathological report which was taken as gold standard. Results: RMI 3 had a sensitivity of 100%, a specificity of 91.67%, a positive predictive value of 97.50% and negative predictive value of 100%. Conclusions: This scoring system due to its simplicity and applicability can be used by the general gynaecologists at the periphery to refer suspected ovarian cancer to oncologicalcenters and thereby improving the survival and prognosis of women undergoing surgery for ovarian tumors.
Keywords: Adnexalmass, Benign ovarian tumor, CA-125, Malignantovarian tumor, Menopausalstatus, Risk Malignancy Index
Full Text:
INTRODUCTION
Ovarian cancer is one of the leading causes of mortality in females.1 The annual percentage of increase in age-standardized incidence rates ranged from 0.7% to 2.4%.2 Gynecological cancer constitutes about 30% of the total cancers among women in India and ovarian cancer contributes about 19.8% of the total cases.3
Risk malignancy index (RMI) is a simple scoring system based on serum CA 125, USG score & menopausal status. It is useful in predicting a malignant ovarian mass and in differentiating malignant from benign ovarian mass. Most of the ovarian tumors are diagnosed at a later stage since the onset and progression of this tumor makes early diagnosis difficult.
There is a significant difference in the management of malignant and benign tumors. Pre-operative knowledge is necessary to determine the nature of adnexal mass for optimal and appropriate primary treatment.
RMI-1 was developed by Jacobs et al. in 1990 and RMI-2 was developed by Tingulstad et al. with slight modification in the score value of menopausal status and ultrasound score. It was modified to RMI-3 in 1994.4 Cut-off value of Risk of malignancy index is taken 250 to increase the detection rate of true negativecases.5
Preoperative determination of the nature of adnexal mass is necessary for optimal and appropriate primary treatment. RMI is a simple scoring system which can be applied in less specialized centers.
MATERIAL AND METHODS
The present study was conducted in the Department of Obstetrics & Gynaecology in collaboration with Department of Pathology and Department of Radiodiagnosis, Institute of Medical Sciences, Banaras Hindu University from July 2017 to June 2019.
This is a prospective study on 100 patients with clinically diagnosed ovarian masses attending either outdoor or admitted in the gynecology ward of SSH, BHU, Varanasi. Written informed consent was obtained from all the participants prior to the enrolment for the study. Confirmed adnexal masses cases were selected purposively from outdoor and those hospitalized in the Gynaecology ward, SSH, BHU.
Inclusion criteria
Women with clinically detected ovarian mass of any age group. In premenopausal women, the criteria for ovarian masses sizeare more than 8 cm. Postmenopausal status defined as more than 1 year of amenorrhea or, who underwent hysterectomy and criteria for ovarian mass size is more than 5 cm.
Exclusion criteria-
Women having an ovarian tumor with other conditions like endometriosis, fibroid, pregnancy, PID, women in menstruating phase and associated with concurrent malignancy. Patients who were unfit for major surgery, inoperable cases, or previous major pelvic surgery.
Intraoperatively, any other mass other than ovary was also excluded from study. Women with already diagnosed cases of ovarian malignancy receiving chemotherapy, masses arises from GI tract or urinary bladder, pregnancy and its complications like ectopic, molar and post-abortive were excluded.
Clinical history was taken including Age, Parity, menstrual history, socioeconomic status and symptoms. Personal, family and history of any medical illness were also obtained. Premenopausal and Postmenopausal status was certain in each subject.
Serum CA125 level was estimated in all subjects.
Risk of malignancy index (RMI)
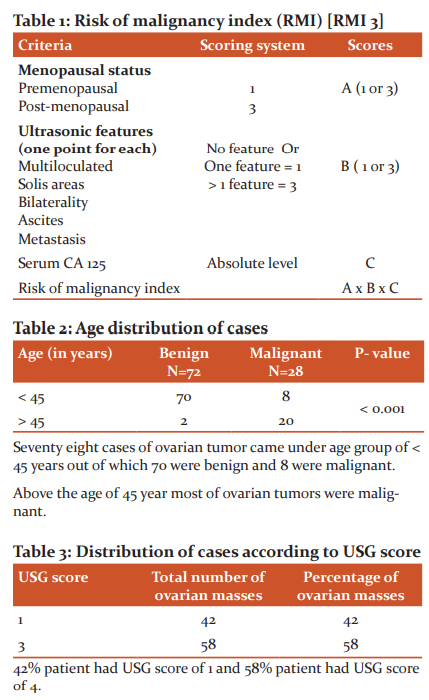
RMI – U x M x value of CA-125 (Table 1)
USG scoring
Transabdominal scans were done using a 3.5MHz and transvaginal scan were done with a 7.5Mz transducer. The lesions were evaluated according to size, shape and multiplicity, the thickness of wall and septa and ascites. Scoring system based on sonographic findings. Morphological evaluation was done using ultrasonography.USG score was done within 2 week prior to laparotomy.
SerumCA-125 levelestimation
A peripheral venous sample was taken from each patient, prior to surgery for the estimation of serum CA-125 levels by radioimmunoassay. Abnormal CA-125 level is defined as serum levels > 35 U/ml, (considered a high risk for ovarian malignancy).
Menopausal scoring (M)-
Menopausal status was defined as one or more years of amenorrhoea or women who had undergone a hysterectomy. All other women were considered premenopausal. For premenopausal women score 1 was given and for postmenopausal women score 3 was given.
Risk of malignancy index was calculated for each subject by multiplying USG score, absolute values of CA-125 serum levels and menopausal score.
Operative finding during laparotomy of all cases were noted. An operative specimen or tissue was sent for histopathological examination. Ascitic fluid or peritoneal washing was sent for cytological examination. Histopathological diagnosis was considered as gold standard for defining outcome.
Therefore RMI is a simple, valuable, highly reliable and clinically applicable scoring system, in the preoperative evaluation of ovarian mass for differentiating malignant from benign lesion.
Interpretation of risk malignancy index (RMI)
If the score was < 25, considered as low risk.
If the score was 25-250, considered a moderate risk.
If the score was >250,considered a high risk.
STATISTICAL ANALYSIS
Chi-square, Fisher's exact tests are used to compare proportion of benign and malignant cases with different ultrasonographic parameters. A p-value <0.05 was considered to be significant. Results of RMI were validated against histopathological confirmed lesions. For patient age and sonographic parameters univariate statistical analysis was performed.
RESULTS:
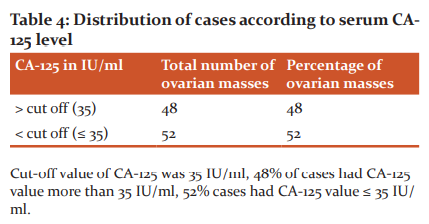
-Maximum patients of benign and malignant ovarian tumor were clustered in age group of less than 45 year and more than 45 year respectively.
-The association between ultrasound score and disease status was not that statistically significant at a P-value of 0.009.
-The association between value of CA-125 and disease status was statistically significant at a p-value of <0.001.
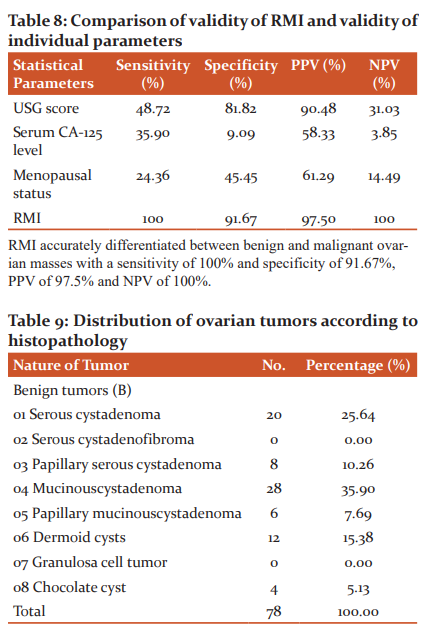
-RMI had a sensitivity of 100%, a specificity of 91.67%, a positive predictive value of 97.50%, and negative predictive value of 100%.
-Menopausal status had sensitivity of 24.36%, specificity of 45.45%, positive predictive value of 61.29%, negative predictive value of 14.49%.
-Serum CA-125 level had a sensitivity 35.90%, a specificity of 9.09%, a positive predictive value of 58.33%, and a negative predictive value of 3.85%.
-Ultrasound score had a sensitivity of 48.72%, a specificity of 81.82%, a positive predictive value of 90.48%, and a negative predictive value of 31.03%.
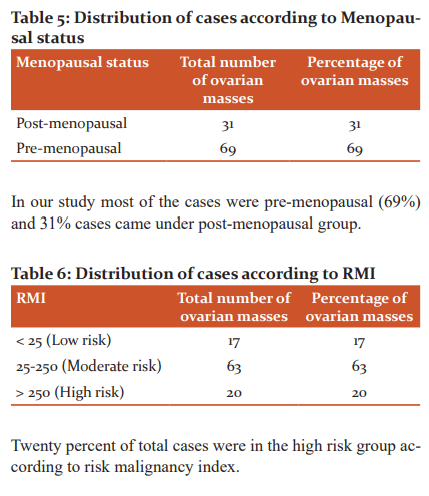
-20 out of 100 subjects had RMI > 250 of which 20 subjects had malignant tumor. Eighty subjects had RMI < 250 of which 78 had benign tumor, and 2 had malignant tumor.
-Analysing the diagnostic performance of RMI, we found that RMI performed better than individual parameters in differentiating benign and malignant ovarian tumors at the cut-off score of 250.
DISCUSSION
-Risk of malignancy index is the multiplication of serum CA-125, menopausal status and USG findings. In this study, the cut-off level of RMI is taken as 250.[RMI 3 is calculated]
-If ovarian cancers are diagnosed at early stage (stage I or II), the cure rate could be as high as 80-90% and the mortality rate could decrease up to 50%. Hence, this method of diagnosis is of great importance for the prediction of the prognosis. Selective referral of patients with high risk of malignancy to specialized oncology centers is of great importance.
-Comprehensive index overcomes the false-positive result obtained when using a single parameter like menopausal status or serum CA-125 or USG alone. RMI also increases the sensitivity and specificity in the pre-operative diagnosis of ovarian mass.
-In this study, the cut-off level of RMI is taken as 250. This scoring was more closer to ZinatossadatBouzari et al., who used 265 as cut-off.6
-In this study out of 100 cases 28 cases (28%) were malignant (Table-2), out of which 20 cases were more than 45 year age group, which is statistically significant (p-value of <0.001). Rujuta J and Nandita M have made similar observations (malignant cases 15%, 17.2% more than 45 years age) (2015).7
-In our study we assigned USG scores of 1 (absence of specific findings or presence of one finding) or 3 (two or more findings) to the subjects (Table-3, 7), depending on the ultrasound findings, 42% of cases had an ultrasound score of 1, while 58% patients scored 3 (p-value 0.009). Dora SK. et al (2017) have observed 45.23% have USG score 1 and 54.76% having score of 3.8
-Premenopausal patients predominate in our study (69%) (Table-5), while 31% of the affected patients were in the postmenopausal group. Among the postmenopausal patients, 19 had benign diseases, while 12 had the malignant diseases (table-7).In this study, menopausal status had a sensitivity of 24.36% and specificity of 45.45%
-Hence menopausal status could be a weak constituent of RMI. In the study of TaherahAshrafgangooei et al., had shown higher specificity of 93.18%.9 This discrepancy was due to the proportion of sample size which included a large number of premenopausal women as compared to postmenopausal (86.3%) in their study. In premenopausal age group most of the ovarian masses were benign compared to postmenopausal patients with a P-value of 0.008.
-In present study, out of 100 clinically diagnosed cases 52 cases were noted with lower CA-125 value ( <35IU/ml) and 48 cases with CA-125 value >35IU/ml (Table-4 ). Out of 48 patients of CA-125 value >35IU/ml, 28 cases were benign and 20 were malignant. Out of 52 cases with lower CA-125 value (<35 IU/ml), 50 cases were benign and 2 were malignant (Table-7).
-Ultrasonography is widely appreciated as the best imaging method for evaluation of ovarian pathology. Several groups have reported higher values for this method. In our study, an ultrasound score of 3 had a sensitivity (48.72%), specificity 81.82%, positive predictive value 90.48% and negative predictive value (31.03%) among the parameters evaluated. [Yelikar KA et al. 2016]10
-Serum CA-125 level is widely appreciated as a useful biomarker for estimating the risk of ovarian cancer, though other gynecological pathology can also increase its levels. Mayer AR et al. have earlier reported sensitivity and specificity of less than 80%, for this marker, in the prediction of ovarian cancers.11Simsek et al. (2014) has reported a sensitivity of 78.6% and specificity of 63.5% for a CA-125 cut-off of 35 IU/ml.12 In our study, CA-125 levels >35IU/ml had a sensitivity of 35.90%, specificity of only 9.09%, positive predictive value of 58.33%, and negative predictive value of 3.85% respectively. (Statistically significant p-value <0.001). This discrepancy in the present study was due to small sample size.
-Rao (2014) had reported higher sensitivity, specificity and positive and negative predictive values for a postmenopausal score of 3.13 In our study, this parameter had sensitivity (24.36%), specificity (45.54%), positive predictive value (61.29%) and negative predictive values (61.29%) in assessing malignancy risk. This discrepancy in the present study was due to the proportion of sample size which included a large number of premenopausal women as compared to postmenopausal
-The RMI cut-offs in many studies ranged from 25 to 250 (reviewed in Geomini et al. 2009).14,15 Most studies reported an increased diagnostic accuracy and performance with an RMI cut-off of 200.16 Yamamoto et al. (2009) reported a sensitivity and specificity of 75% and 91%, respectively.17
-A systematic review study by Geomini et al. in 2009,116 diagnostic studies for adnexal malignancy was reviewed.18 The reported results showed that RMI at cut-off point of 200 had a sensitivity of 78% and a specificity 87% for malignant mass diagnosis.
-According to the results of Ulusoys et al. in 2007, the RMI in a cut-off level of 153 showed a sensitivity of 76.4%, a specificity of 77.9%, a PPV of 65.9% and an NPV of 85.5% for prediction of malignancy.19 In our present study, RMI, at a cut-off level of 250 had a high sensitivity (100%) and high specificity (91.67%), PPV of 97.50% and NPV of 100% respectively.
-From our results RMI is suggested to be better than other single parameter.
-False-negative rate should ideally be zero or close to zero to exclude malignancies. Higher cut-off value of RMI is taken so that specificity increases and false-negative cases decrease, so that problem of limitation of referral to distant centers can overcome.
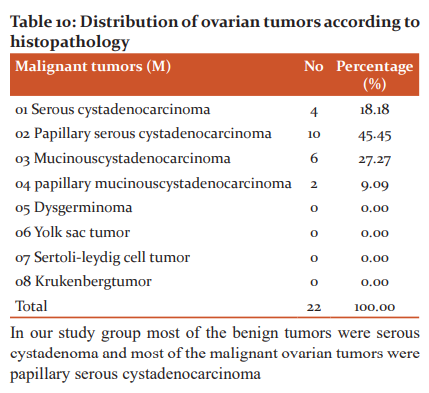
-Table-9, 10, when the distribution of ovarian tumors was studied according to histopathology report, 78% cases were benign and 22% were malignant. Out of benign cases 35.90% were Mucinouscystadenoma, 25.64% were serous cystadenoma and 15.38 % were dermoid cyst. Out of Malignant tumor 45.45% were papillary serous cystadenocarcinoma, 27.27% were Mucinouscystadenocarcinoma and 18.18% were serous cystadenocarcinoma. Nearly similar figures have been observed by Dora et al. in 2017.
CONCLUSION
The present study demonstrates that the validity of RMI is higher as compared to validity of individual parameters. In a low-resource setting where sophisticated radiological and biochemical tests may not be available at all places, where RMI can be used as an investigation for the triage of patients and referral to a higher center.
ACKNOWLEDGEMENTS
We would like to thanks all the support member of department of Obstetrics and Gynaecology, department of Radiodiagnosis and Imaging and Department of Pathology, Banaras Hindu University, and Varanasi India. We also acknowledge the immense help received from the scholar article are cited and included in references of this manuscript.
Source of Funding: Done by hospital.
Conflict of interest: No competing interests.
Ethical approval: The study was approved by the ethical committee of the hospital. The ethical committee approval number is Dean/2018/EC/482. The aim of the study was explained appropriately and informed written consent was obtained from all the patients.
Authors’ Contribution:
All the work including study conception and design, data collection, patient selection, consent, histopathology report collection, analysis and interpretation of results and manuscript preparation done by Dr Neha Kumari under guidance of Dr Mamta Singh.

References:
1. Spencer JA. A multidisciplinary approach to ovarian cancer at diagnosis. The British J Radiol. 2005;78(2005): S95-102.rmi 17.
2. Murthy NS, Shalini S, Suman G, Pruthvish S, Mathew A. Changing trends in incidence of ovarian cancer - the Indian scenario. Asian Pac J Cancer Prev. 2009;10(6):1025-30.
3. Kanan AYSonali SD, Sandip SN, Sanjaykumar BP. Evaluation of the validity of risk malignancy index in clinically diagnosed ovarian masses and to compare it with the validity of individual constituent parameters of risk malignancy index. Int J Reprod Contracept Obstet Gynecol. 2016 Feb;5(2):460-464
4. Tingulstad S, Hagen B, Shjerdestad FE, Onsrud M, Kiserud T, Halorsen T, et al. Evaluation of a risk of malignancy index based on serum CA 125, USG findings and menopausal status in the preoperative diagnosis of pelvic masses. Br J Obstet Gynaecol. 1996:103:826-31
5. RCOG Guideline No. 34 October 2003, Reviewed 2010.
6. Bouzari Z, Yazdani S, Ahmadi MH, Barat S, Kelagar ZS, Kutenaie MJ et al. Comparison of three malignancy risk indices and CA-125 in the preoperative evaluation of patients with pelvic masses. BMC Res Notes. 2011;4:206.
7. Javdekar R, Maitra N. Risk of Malignancy Index (RMI) in Evaluation of Adnexal Mass. The Journal of Obstetrics and Gynecology of India (March–April 2015) 65(2):117–121.
8. Santosh KD, Atal BD, Benudhar P and Jatindra PH. A prospective study to evaluate the risk malignancy index and its diagnostic implication in patients with a suspected ovarian mass. Dora et al. Journal of Ovarian Research (2017)10:55. DOI 10.1186/s13048-017-0351-2
9. Tahereh A, Mahdieh R. Risk of malignancy index in preoperative evaluation of pelvic masses. Asian Pac J Cancer Prev. 2011;12:1727-30.
10.Kanan AY, Sonali SD, Sandip SN, Sanjaykumar BP. Evaluation of the validity of risk malignancy index in clinically diagnosed ovarian masses and to compare it with the validity of individual constituent parameter of risk malignancy index. Int J Reprod Contracept Obstet Gynecol. 2016 Feb;5(2):460-464
11. Mayer AR, Chambers SK, Graves E, Home C, Tseng PC, Nelson GE, et al. Ovarian cancer staging: does it require a gynecologic oncologist? Gynecol Oncol. 1992; 47:223–7.
12. Simsek HS, Tokmak A, Ozgu E. Ole of a risk of malignancy index in clinical approaches to adnexal masses. Asian Pac J Cancer Prev. 2014;15(18): 7793–7.
13. Rao JH. Risk of malignancy index in assessment of pelvic mass. Int J Biomed Res. 2014;5(3):184-6.
14. Geomini P, Kruitwagen R, Bremer GL, Cnossen J, Mol BWJ. The accuracy of risk scores in predicting ovarian malignancy: a systematic review. Obstet Gynecol. 2009;113(2):384–94.
15. Tahereh A, Mahdieh R. Risk of malignancy index in preoperative evaluation of pelvic masses. Asian Pac J Cancer Prev. 2011;12:1727-30.
16. Jacobs I, Oram D, Fairbanks J, Turner J, Frost C, Grudzinskas JG. A risk of malignancy index incorporating CA125, ultrasound and menopausal status for the accurate preoperative diagnosis of ovarian cancer. Br J Obstet Gynaecol. 1990;97(10):922-9.
17. Yamamoto Y, Yamada R, Oguri H, Maeda N, Fukaya T. Comparison of four malignancy risk indices in the preoperative evaluation of patients with pelvic masses. Eur J Obstet Gynecol Reprod Biol. 2009;144(2):163–7.
18.Geomini P, Kruitwagen R, Bremer GL, Cnossen J, Mol BWJ. The accuracy of risk scores in predicting ovarian malignancy: a systematic review. Obstet Gynecol. 2009;113(2):384–94.
19. Ulusoy S, Akbayir O, Numanoglu C, Ulusoy N, Odabas E, Gulkijik A. The risk of malignancy index in discrimination of adnexal masses. Int J Gynaecol Obstet. 2007;96(3):186–91.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License