IJCRR - 14(2), January, 2022
Pages: 17-22
Date of Publication: 16-Jan-2022
Print Article
Download XML Download PDF
Impact of COVID-19 on RPE & Functional Status of Patients Using PCFS Scale: A Cross-Sectional Survey
Author: Reema Joshi, Shilpa Khandare, Madhuri Rai, Mrunal Rasane, Roopali Banerjee, Sajitha Harilal, Ruturaj Salvi
Category: Healthcare
Abstract:Introduction: \"Post-COVID-19 Functional Status (PCFS) scale\" been recommended to evaluate functional status of post COV�ID-19 patients. It is proposed that it could be used to get the information of functional squeal of COVID-19. Aim: To evaluate the Impact of COVID-19 on Functional Status in relation to age, gender, BMI, RPE level and Co-morbidities. Method: During the period of October 2020 till March 2021 study was conducted. Patients who had COVID-19 four weeks before and got discharged were included in study. Patients who were admitted in the COVID ward during last six month were contacted on telephone and those who were willing to be part of the study were included. They were called on appointment basis to OPD of Dr D Y Patil College of Physiotherapy, Pune and assessed with RPE and PCFS scale. Results: 80% of COVID-19 recovered cases have varied degrees of functional limitation while performing different type of activities ranging from negligible (67.1%), slight (19.4%), moderate (12%) to severe (3.5%) based on PCFS. Furthermore, there was a substantial variance between the score of PCFS with age (P= 0.003), gender (P= 0.014), the duration since the onset of the symptoms of COVID-19 (P < 0.001) and lastly the presence of any co-morbid disorder (P< 0.001). Conclusions: Most of the COVID-19 recovered cases have diverse degrees of functional restrictions ranging from negligible to severe based on PCFS. These restrictions were affected by age, gender, periodic influenza vaccination, smoking, duration since symptoms onset, need for oxygen or ICU admittance, and lastly the presence of coexisting co-morbidity.
Keywords: Post COVID-19 Patients, PCFS, Functional Status, SARS-CoV-2, RPE, Dyspnoea
Full Text:
INTRODUCTION
The Novel Corona virus disease (COVID-19) is an emerging respiratory infectious disease caused by severe acute respiratory syndrome-Coronavirus-2. The SARS COV-2 is known to be the causative agent of a potentially fatal disease that is of enormous global public health concern. In December 2019, there as a cluster of pneumonia cases of unknown etiology in Wuhan, Hubei Province, China. The virus has spread globally to infect over 180 countries. SARS-CoV-2 has infected humans in all age groups, of all races, both males and females while spreading across communities at an alarming rate. The symptoms range from asymptomatic, to most common symptoms like fever, dry cough, fatigue, headache, sore throat, diarrhea, anosmia, ageusia to severe symptoms like pneumonia and acute respiratory distress syndrome.6
SARS infections have revealed a considerable impact on the respiratory system, and musculoskeletal system which includes skeletal muscle, neurological, bone, and joint disorders. Extensive ventilator use also causes elevation of cytokines and C-reactive protein (CRP) causing pro-inflammatory sequelae inducing muscle de-conditioning in the recovery period. There was a subsequent reduction in the health indices hampering the quality of life due to depletion in the functional capacity of these patients.13
The Borg Rating of Perceived Exertion (RPE) is a method of measuring physical activity intensity level. RPE is a personalized exertion grading since it gives a good estimate of heart rate during physical activity. The RPE scale runs from1-10. Physical activity and exercise is imperative in maintaining the muscle mass and to stay healthy. Impaired physical function caused by SARS-COV2 infection is multidirectional due to an extended period of immobilization leading to muscle de-conditioning and infection resulting in disturbance in mitochondrial homeostasis. Physical inactivity is correlated with deleterious effects comprising of decreased levels of aerobic performance and reduction in VO2 peak and depletion in musculoskeletal and cognitive function. It is also linked to several metabolic disturbances involving changes in Insulin signaling. This causes rise in peripheral insulin resistance and growth of inflammatory mediators along with adipose tissue lipolysis and changes in the function of mitochondria. Physical inactivity produces increased insulin sensitivity in the skeletal muscle which causes the dissemination of energy substrates to surround tissues leading to central fat accumulation.16, 17The Post COVID-19 functional status scale (PCFS) is an ordinal tool to measure the full spectrum of functional status in a recovered post-COVID-19 individual. F.A. Klok, G.J.A.M. Boon and B. Siegerink drafted the first version of the manuscript. This scale is a tool to keep a track on function independence of post-COVID patients and also can be used as a full range of functional outcomes. It focuses on constraints in day to day activities and changes in lifestyle. It comprises of 6 grades according to the functional capabilities of the individual post-recovery. The proposed “Post- COVID-19 Functional Status (PCFS) scale” could be assessed upon discharge from the hospital, at 4 and 8 weeks post-discharge to monitor direct recovery, and at 6 months to assess functional sequelae.18 Hence it is necessary to identify the magnitude of the impact of COVID- 19 infection on functional status and rate of perceived exertion in recovered post-COVID-19 patients.
METHODS:
A Cross-Sectional Study was conducted in Pune City. During the period of October 2020 till March 2021 around 500 patients, contacts were received from the COVID ward of the hospital those who were recovered 4 weeks back from COVID-19 were interviewed on the telephone and the study intention was explained about Post COVID functional status of COVID patients. Out of those who were interested were called with appointment to OPD of Dr D. Y. Patil College of Physiotherapy, Pune. Both male and female above the age of 25 years were included whereas any patient with any acute symptoms, fever, excessive fatigue, recent injury, severe cardiovascular complications were excluded from survey. The Borg Rating of Perceived Exertion (RPE) was used to measure the physical activity intensity level.14 RPE is a personalized exertion grading since it gives a good estimate of heart rate during physical activity. 6-minute walk test was performed and after that patient's RPE level was graded based on the Modified Borg scale grading 1-10 with 1 as “nothing”, 2 as “very easy” 3 as “Easy “,4 as “comfortable”,5 as “somewhat difficult”,6 as “difficult”,7 as “hard", 8 as "very hard",9 as “extremely hard”,10 as “maximal exhaustion” 15. All the subjects were also assessed with Hindi & English versions of Post COVID-19 Functional Status Scale (PCFS) to evaluate the magnitude of functional limitations in the recovered post-COVID-19 patients. The PCFS is an ordinal scale with kappa’s of 0.75 and 1.0 developed by Klok and his colleagues incorporating six components based on basic activities of daily living, instrumental activities of daily living, participation in social roles and symptom checklist. The functional limitations were graded according to Grade-0 (with no functional limitations), Grade 1 (with negligible functional limitations), Grade 2 (with significant functional limitations), Grade 3 (with moderate functional limitations) and Grade 4 (with severe functional limitations).
Statistical Analysis:
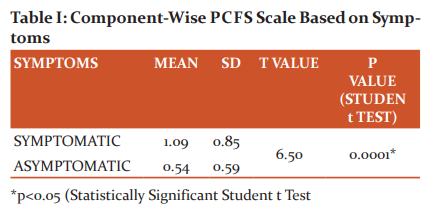
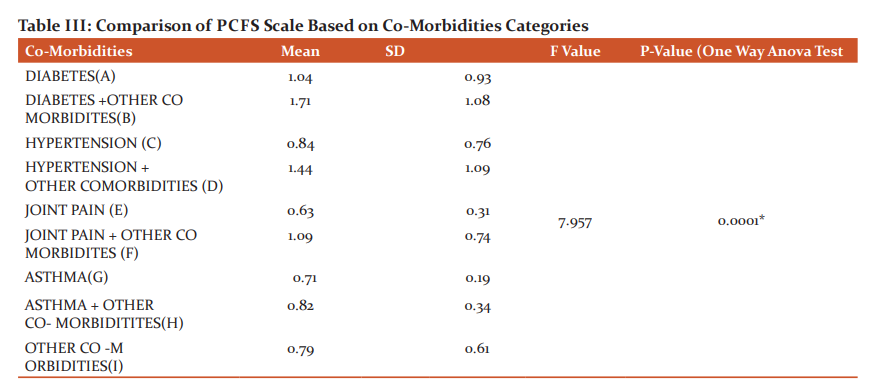
Data was analyzed using the statistical package SPSS 22.0 (SPSS Inc., Chicago, IL) and level of significance was set at P<0.05. Descriptive statistics was performed to assess the mean and standard deviation of the respective groups. Normality of the data was assessed using Shapiro Wilkinson test. Inferential statistics to find out the difference between the groups was done using ANOVA TEST AND TUKEY HSD POSTHOC TEST and STUDENT t TEST. The component-wise comparison of PCFS scale with co-morbidities like diabetes mellitus, hypertension, and joint pain was analyzed using the ONE WAY ANOVA test with a significant p-value of 0.0001. The comparison between basic and instrumental components of PCFS scale with body mass index categories was analysed using ONE WAY ANOVA test.
The student t-test shows that there is a significant difference present between the two age categories with respect to PCFS scale (P>0.05).
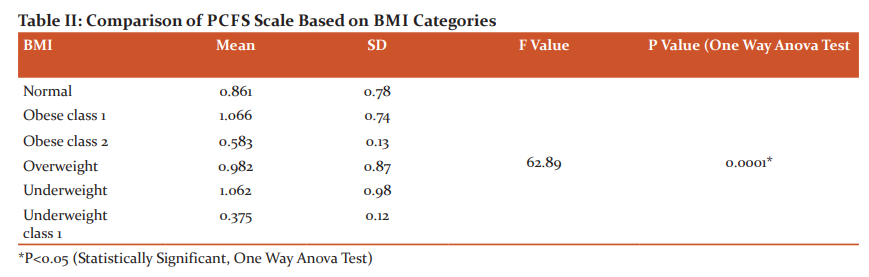
Statistically, significant difference was observed between the BMI categories with respect to PCFS scale where the highest mean was reported in OBESES CLASS 1(1.066) and Underweight ( 1.062) and the least mean was observed in Underweight class 1(0.375).
P<0.05 IS STATISTICALLY SIGNIFICANT ONE WAY ANOVA TEST shows that there is a
Significant difference exist between the co-morbidities regarding the PCFS scale (P<0.05).
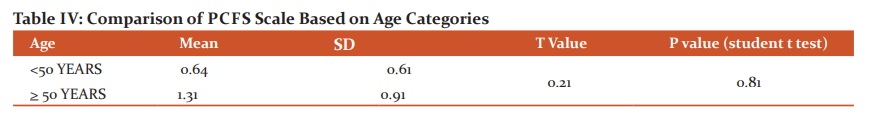
*P<0.05 STATISTICALLY SIGNIFICANT STUDENT t TEST shows that there is no significant difference present between the two age categories with respect to PCFS scale(P>0.05).
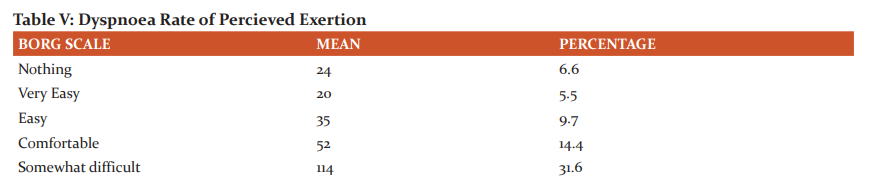
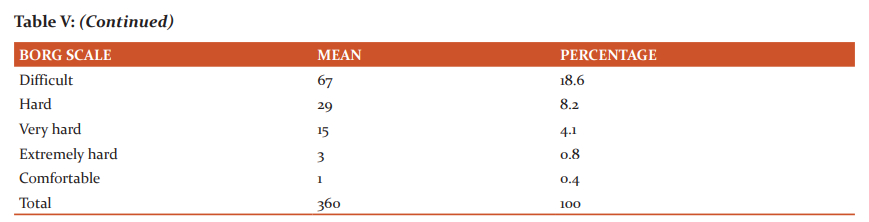
Table explains the rate of perceived exertion using a modified BORG scale. The result shows 31.6% reported “somewhat difficulty” and 18.6% “expressed difficultly “and just 0.4 % and 0.8% expressed “comfortable “and” very hard” respectively.
RESULTS
A total of 565 patients who had COVID 19 was contacted over the telephone out of which 340 completely recovered post-COVID -19 patients were included for the study. 225 individuals were excluded due to acute symptoms from the study. The Data Analysis and interpretation was performed to estimate the Impact of COVID-19 on their functional performance of them using PCFS scale and RPE on Modified Borg Scale. The Comparison of PCFS scale based on symptoms was found functional limitation is more in symptomatic individuals compared to asymptomatic and statistically significant with a p-value of 0.0001(see table 1). The Comparison of PCFS scale based on BMI categories was found to be statistically significant with a p-value of 0.0001 with the highest mean reported in OBESE CLASS 1(1.066) and the least observed in underweight(0.375)(see table2). The comparison between the PCFS scale and Comorbidities revealed the functional limitation was high in hypertensive and diabetic patients on statistical analysis using One-way Anova & Post hoc test p-value of 0.0001(see table 3). Rate of perceived exertion analyzed using Modified Borg scale revealed the highest incidence in the category “somewhat difficult” accounting for 31.6%.
DISCUSSION:
COVID-19 is declared as the deadliest pandemic in most parts of the world with its remarkable consequences on the physical, cognitive, mental and social well-being of our body ultimately provoking deterioration in the overall functional status of the individual. Due to the sudden spike of COVID- 19 cases nationwide lockdown was imposed. Mandatory quarantine protocol had to be followed by patients.18 The study is intended to evaluate the impact of COVID-19 according to their regions and their lifestyle with existing comorbidities on functional status and rate of perceived exertion in recovered post-COVID-19 patients. This study highlights the prolonged health-related squeal in COVID-19 survivors. A Post COVID-19 Functional Status Scale (PCFS) was used to evaluate the magnitude of functional limitations in the recovered post COVID-19 patients. The PCFS is an ordinal scale with kappa’s of 0.75 and 1.0 developed by Klok and his colleagues incorporating six components based on basic activities of daily living, instrumental activities of daily living, participation in social roles and symptom checklist. The functional limitations were graded according to Grade-0 (with no functional limitations), Grade 1 (with negligible functional limitations), Grade 2 (with significant functional limitations), Grade 3 (with moderate functional limitations) and Grade 4 (with severe functional limitations).19 The study was commenced with the screening of 500 recovered post COVID-19 patients. A total of 360 recovered post COVID-19 individuals (215 males and 145 females) with a positive COVID-19 report were included in the study. 140 individuals were enlisted in the exclusion criteria of the study. Out of 360 individuals, 17.1% patients required constant care. Basic activities of daily living component comprised of 9.1% of individuals required assistance in eating, 16.3% of individuals reported the need of assistance in toilet activities, 18.5% of individuals required assistance in routine daily hygiene activities and 25.4% individuals reported the need of assistance in walking. Instrumental activities of daily living incorporated 40.3% of individuals requiring assistance in basic household chores. The data was analyzed using the statistical package SPSS22.0. The normality of the data was assessed using the Shapiro Wilkinson test. Inferential statistics to find of the difference between the groups was done using ONE WAY ANOVA test and TUKEY HSD POST-HOC test and Student t-test. The comparison between PCFS scale with symptomatic and asymptomatic patients was analyzed using student t-test between two age categories ranging from individuals between 25 to 50 years and the second category ranging from 50 years and above. 44.4% population reported of fever as the most predominant symptom followed by 39.1% population who reported of breathlessness and 26.6% population had a cough. There was a significant difference between the two categories with a p-value as 0.0001 which suggests equal chances of functional deterioration in both categories respectively. The comparison between basic and instrumental components of PCFS scale with body mass index categories was analyzed using the ONE WAY ANOVA test. Positive correlation using spearman rank correlation coefficient was observed between normal BMI with upper and lower limit of BMI according to WHO classification suggested a significant difference in the study with a p-value of 0.0001. It suggests that obesity and increased ectopic fat provokes impaired insulin resistance and decreased beta-cell activation leading to loss of effective host defenses and promoting functional immunological deficit. Obesity is associated with compromised immune response and reveal worsened antibody and T-cell response. Considerable hike has been observed in adipocyte count of obese individuals thereby triggering over-expression of ACE-2 receptors. Extensive use of mechanical ventilation causes elevation of cytokines and C- reactive protein (CRP) causing sequelae inducing muscle de-conditioning in the recovery period. There was a subsequent reduction in health indices deteriorating the quality of life. It thereby leads to a decline in the functional status of the individual. A similar study conducted by Manuel Taboada et al. stated that the term ''long COVID” is being used to describe illness in people who are recovered COVID-19 patients but are still reporting long-term effects of the infection.20,21,22
The component-wise comparison of PCFS scale with co-morbidities like diabetes mellitus, hypertension, joint pain was analyzed using ONE WAY ANOVA test with a significant p-value 0.0001. Out of 360 individuals 112 reported of joint pain, 91 reported hypertension and 84 individuals reported of diabetes mellitus. Individuals with diabetes mellitus express high levels of furin enzyme, a type 1 membrane-bound protease that aids the virus to enter the host cell. Obstinate inflammation in diabetic patients amplify their vulnerability to hyper-inflammation thereby initiating cytokine storm.23 Similarly, hypertensive patients exhibit increased levels of ACE-2 receptors attributed to intake of anti-hypertensive drugs. Joint pain and myalgia are frequently observed in post recovered COVID-19 patients due to immunological cascade. Hence, individuals with co-morbidities are more susceptible to higher risk of functional limitation in the recovery phase.24,25 Similar study conducted by Dr. Aarti Gupta et al. stated the majority of COVID-19 cases have different degrees of functional limitations ranging from negligible to severe based on PCFS scale.26 On the assessment of Dyspnea using Rate of perceived exertion (RPE) was taken using the Modified Borg scale. 31.6% of individuals were reported in the “somewhat difficult” category, 17.7 % individuals were reported in the “difficult” category, 8.3% of individuals were reported in the “hard” category and 14.4% individuals were reported in the “comfortable” category post 6 min walk. A comparison of rate of perceived exertion using the Modified Borg Scale with co-morbidities was analyzed. 93.10% of individuals were reported in the “Hard category”, 70.3% individuals were reported in the „difficult category? and 57.2% individuals were reported in the “somewhat difficult category”. Hence it leads to a decline in the functional status of the individual causing a reduction in VO2 max and total lung capacity.
Conclusion: The study strongly recommends a detailed assessment of both symptomatic and asymptomatic individuals to outline effective post-COVID-19 rehabilitation. The subsequent reduction in health indices deteriorating the quality of life has been observed. Early identification of functional decline with the subsequent layout of rehabilitation measures plays a crucial role in post-acute care management of COVID-19. The Post-COVID-19 Functional Status Scale is an effective tool in determining the functional limitations in the acute phase of post-COVID-19 recovery.
Acknowledgment:
The authors would like to thank the participant for co-operating during the entire process. We would also like to acknowledge the support of our colleagues for their assistance. We are thankful to Dr D Y College of Physiotherapy, Pune for giving us permission
Conflict Of Interest: All the authors declare no conflict of interest in any discipline.
Source of Funding: “SELF”
Ethical Statement: Institutional sub-ethical committee of Dr. D.Y. Patil College of Physiotherapy, Pune with ref. DYPCPT/790/2020.
Authors’ Contribution:
Conceptualization: Dr. Reema Joshi, Dr Madhuri Rai,Dr Mrunal Rasane
Methodology: Dr. Reema Joshi, Dr Mrunal Rasane,Dr Ruturaj Salvi.
Software: Dr Ruturaj Salvi
Validation: Dr. Reema Joshi, Dr. Sajitha Harilal
Formal analysis: Dr. Reema Joshi, Dr Madhuri Rai
Investigation: Dr. Mrunal Rasane, Dr. Sajitha Harilal,Dr Roopali Banerjee
Data curation: Dr. Reema Joshi, Dr Ruturaj Salvi
Writing – Original Draft: Dr Reema Joshi
Writing – Review & Editing: Dr. Shilpa Khandare.
Visualization: Dr. Reema Joshi
Supervision: Dr.Shilpa Khandare
Project administration: Dr. Reema Joshi
References:
-
Lai CC, Chih-Cheng L, Tzu-Ping S, Wen-Chien K, Hung-Jen T, Po-Ren H et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges Int. J. Antimicrob. Agents 17:105924.
-
HuipengGe, Xiufen Wang, Xiangning Yuan, Gong Xiao, Chengzhi Wang, Tianci Deng et al.The epidemiology and clinical information about COVID-19. 2020 Apr 14:1.
-
Ghosh A. Srijita N, Tapas KM How India is dealing with COVID-19 pandemic. Sensors International. 2020 Jan 1; 1:100021.
-
Adeknule S, Chuku O, Aleksandra M, Risha P, Kokab Y, Priyank D et al. Comorbidity and its Impact on Patients with COVID-19. SN comprehensive clinical medicine. 2020 Jun 25:1-8.
-
Husain R, Siddappa B. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. Journal of autoimmunity. 2020 Feb 26:102433
-
https://www.who.int/emergencies/diseases/novel-coronavirus-2019
-
Bandyopadhyay D, Tauseef A, Adrija H, Manasvi G, Avash D, Sandipan C et al. COVID-19 pandemic: cardiovascular complications and future implications. Am. J. Cardiovasc.2020 Jun 23:1-4.
-
Shereen MA, Suliman K, Abeer K, Nadia B, Rabeea S. COVID-19 infection: Origin, transmission and characteristics of human coronaviruses. J. Adv. Res. 2020 Mar 16.
-
Bohn M, Hall A, Sepiashvili L, Jung B, Shannon S, Khosrow A. Pathophysiology of COVID-19: mechanisms underlying disease severity and progression. Physiology. 2020 Sep 1;35(5):288-301.
-
https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/what- coronavirus-does-to-the-lungs?amp=true
-
Varkey B, Bhattacharjee S. Neurological complications with COVID-19: A contemporaneous review. Annals of Indian Academy of Neurology. 2020 Jul 1;23(4):468.
-
Qing Ye, Wang B, Zhang T, Xu J, Shang S. The mechanism and treatment of gastrointestinal symptoms in patients with COVID-19. An J Physiol Gastrointest Liver Physiol Aug 1;319(2): G245-52.
-
Disser N, Micheli A, Schenk M, Konnaris M, Piacentini A, Daniel LE et al. Musculoskeletal consequences of COVID-19. JBJS. 2020 Jul 15;102(14):1197-204.
-
https://www.cdc.gov/physicalctivity/basics/measuring/exertion.htm
15. .https://www.nursing center.com/journalarticle?Article_ID=2695880&Issue_ID=4388241
-
Rooney S, Webster A, Paul L. Systematic Review of Changes and Recovery in Physical Function and Fitness after Severe Acute Respiratory Syndrome–Related Coronavirus Infection: Implications for COVID-19 Rehabilitation. Physical Therapy. 2020 Sep 28;100(10):1717-29.
-
Woods J, Hutchinson NT, Powers SK, Roberts WO, Gomez-Cabrera, Radak Z et al. The COVID-19 pandemic and physical activity. 2020 June 2(2)
-
Pant P, Joshi A, Basnet B, Shrestha B, Bista N, Bam Net al. Prevalence of Functional Limitation in COVID-19 Recovered Patients Using the Post COVID-19 Functional Status Scale. JNMA 2021 Jan;59(233):7.
-
Klok FA, Boon G, Barco S, Endres M, Geelhoed J, Knauss S et.al. The Post-COVID-19 Functional Status scale: a tool to measure functional status over time after COVID-19. Eur. Respir. J.2020 Jul 1;56(1).
-
Sattar N, Mclnnes I, McMurray J. Obesity is a risk factor for severe COVID-19 infection: multiple potential mechanisms. Circulation. 2020 Jul 7;142(1):4-6.
-
Mohammad S, Aziz R, Mahri S, Malik S, Haji E, Khan A et al. Obesity and COVID-19: what makes obese host so vulnerable? Immunity & Ageing. 2021 Dec; 18 (1):1-0.
-
Taboada M, Morano E, Carinena A, Rey T, Romero R, Leal S et al. Quality of life, functional status, and persistent symptoms after intensive care of COVID-19 patients. British journal of anaesthesia. 2021 Mar 1;126(3):e110-3.
-
Callender LA, Curran M, Bates S, Mairess M, Weigandt J, Bettes C et al. The impact of pre-existing co-morbidities and therapeutic interventions on COVID-19. Frontiers in Immunology. 2020;11.
-
Ejaz H, Alsrhani A, Zafar A, Javed H, Junaid S, Abdalla A et al. COVID-19 and co-morbidities: Deleterious impact on infected patients. Journal of Infection and Public Health. 2020 Aug 4.
-
Thaweerat W. Current evidence on pancreatic involvement in SARS-CoV-2 infection. Pancreatology. 2020 May 27.
-
Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? The Lancet. Respiratory Medicine. 2020 Apr;8 (4):e21.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License