IJCRR - 7(20), October, 2015
Pages: 22-29
Date of Publication: 20-Oct-2015
Print Article
Download XML Download PDF
A GUIDE TO MANAGEMENT OF VARIOUS ENDODONTIC PERIODONTAL LESIONS - A CASE SERIES
Author: Rajendran Maheaswari, A. Selvam, M. Jeeva Rekha, A. Mahalakshmi, Tukaram Kshirsagar Jaishree
Category: Healthcare
Abstract:Aim: To explain the key to identify the primary disease and secondary disease of the endodontic periodontal lesion and its management using a case series. Case description: Four cases belonging to different types of endodontic periodontal lesion such as primary endodontic with secondary periodontic lesion, primary periodontic with secondary endodontic lesion, combined lesion, iatrogenic periodontal lesion were explained. The appropriate management and its outcome for each case was elaborated and justified. Discussion: In all the four cases, patient presented with established chronic secondary disease. Hence all the cases were planned to complete the endodontic therapy initially and then proceed with periodontal therapy such as open flap debridement, hemisection and bone graft, platelet rich fibrin and guided tissue regeneration. Conclusion: Treatment outcome will be more predictable if the clinician has more thorough knowledge about the diagnosis, treatment sequence with inter-disciplinary approach .Thereby the immediate and true management of the endodontic- periodontic lesions can impede the loss of the natural tooth and delay the more complex treatment.
Keywords: Endo perio lesion, Platelet rich fibrin, Palato radicular groove, Hemisection, Iatrogenic perforation
Full Text:
INTRODUCTION
Interrelationship of pulp and periodontium begins from the embryonic stage of development of the tooth since they have a common origin (dental papillae). Thus pulp and periodontium has embryonic, functional and anatomic relationship (1). Effect of periodontal disease on the pulp was first described by Turner and Drew in 1919(5). In 1964, Simring and Goldberg described relationship of periodontal and pulpal disease (6). Studies stated that bacterial plaque is the main cause for coexistence of periodontal and pulpal lesion(9-12).The accurate identification of pathway for spread of infection is still a controversy due to presence of various routes such as apical foramen, accessory, lateral, and secondary canals, dentinal tubules and iatrogenic perforation (2,3, 4, 7, 8). According to the primary disease with its secondary manifestation, endodontic periodontal lesions are classified by, Khalid S in 2014 as (13)-
(1) Retrograde periodontal disease: (a) Primary endodontic lesion with drainage through the periodontal ligament, (b) Primary endodontic lesion with secondary periodontal involvement;
(2) Primary periodontal lesion;
(3) Primary periodontal lesion with secondary endodontic involvement;
(4) Combined endodontic-periodontal lesion;
(5) Iatrogenic periodontal lesion. Clinically, a deep narrow probing defect is detected on any aspect of the tooth in cases of primary endodontic lesion with drainage through the periodontal ligament. It represents the sinus tract of the endodontic lesion (13). In cases of primary endodontic lesion with secondary periodontal involvement, long-term existence of the defect, results in advancement of the periodontal disease (13). The primary periodontal lesion with secondary endodontic involvement is due to progression of periodontal infection through lateral canal foramen or apical foramen. Pulp remains vital in most cases of primary periodontal lesion (13). In conditions of combined endodontic-periodontal lesion, the tooth has a nonvital pulp, infected root canal system and a coexisting periodontal defect (13). Iatrogenic periodontal lesions could be due to any adverse condition during dental treatment such as root perforations, coronal leakage along the margin of restoration, dental injuries or trauma, vertical root fractures, use of chemicals such as hydrogen peroxide (17) Identification and elimination of the primary etiopathogenesis of the existing condition is the key route for the success of treatment. Management of the cases in the above conditions mainly depend upon factors such as elimination of the primary cause of the lesion, functional need for the tooth, its restorability after treatment, the prognosis of the tooth, patient cooperation etc(14,15,16,17) Management of these cases often requires combined team approach of an endodontist and a periodontist. In regular practice, endodontic treatment is often followed up by periodontal therapy. In this case report, few cases of periodontitis associated with endodontic lesions and its management has been discussed in the following sections.
CASE REPORTS
Case 1: Primary endodontic with secondary periodontic lesion
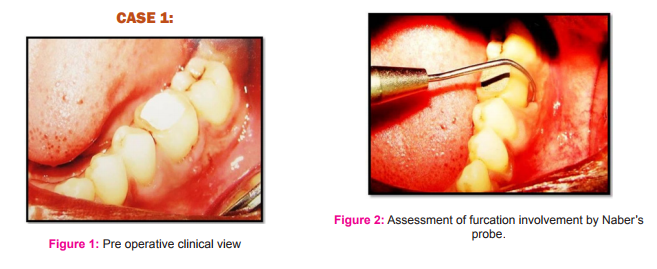
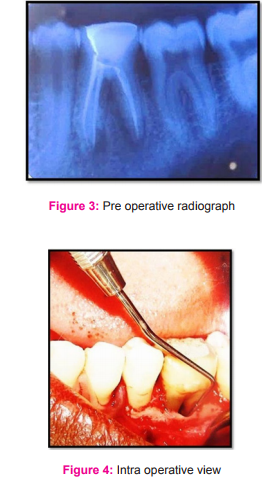
A 33 years old female patient reported to Department of Periodontics with a complaint of recurrent swelling and pus discharge in relation to #36 with the history of endodontic treatment in # 36, 6 months back. On clinical examination, the root canal treated #36 presented with grade II furcation involvement and with the probing depth of 8mm with pus discharge from periodontal pocket (Fig.1 and 2). Intra oral periapical radiograph revealed inter dental bone loss in between 36 and 37 and periradicular radiolucency in relation to both mesial and distal root of #36 (Fig.3). After phase 1 therapy, persistence of periodontal pocket in relation to #36 was noted, hence open flap debridement was planned. Under local anesthesia, on elevation of mucoperiosteal flap, Cul-de-sac furcation involvement was detected in relation to #36 (Fig.4). Degranulation and debridement of the furcation defect was done. On achieving hemostasis, flaps were approximated and sutured with black silk 3-0 (Mersilk (Ethicon) – Johnson and Johnson pvt Ltd, India) and periodontal dressing was given. Evaluation after 6 months revealed no signs of inflammation, reduced probing depth with satisfactory radiographic bone fill (Fig.5 and 6).
Case 2: Primary periodontic with secondary endodontic lesion
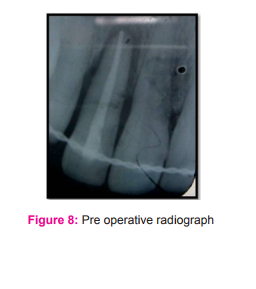
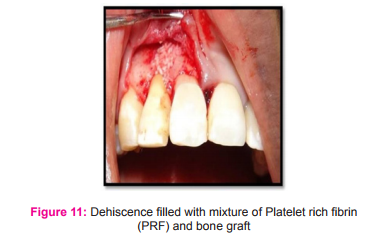
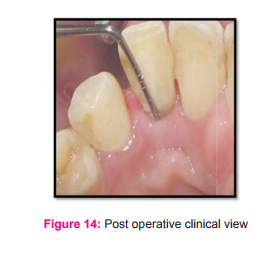
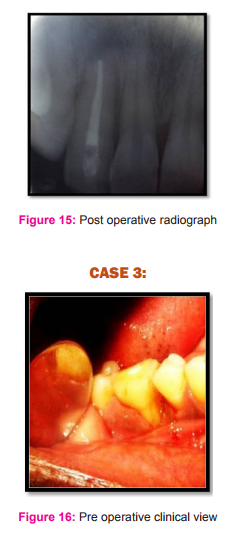
A 32 years old female patient was referred from Department of Endodontics for management of mobility of tooth #12. On clinical examination, it was root canal treated #12 and presented with grade II mobility with probing depth of 8mm on its palatal aspect (Fig.7). On careful examination, a palato radicular groove was detected in relation to #12 extending beyond the cervical margin. IOPA revealed periradicular radiolucency in #12 (Fig.8). Non surgical Phase 1 therapy with temporary splinting was done and the tooth was kept under observation. During re evaluation after 3 months, surgical management was planned. Under local anesthesia, mucoperiosteal flap was elevated in relation to #12. Dehiscence was seen labially (Fig.9) and a palato radicular groove extending till the apical third of the root with a three walled intra osseous defect was detected (Fig.10). After complete debridement, the palato radicular groove was restored with glass ionomer cement (GIC) (GCFuji I, Blackwell supplies, Essex) (Fig.13). The labial and palatal defect of #12 was planned to fill with demineralized bone graft and platelet rich fibrin (PRF). PRF was prepared by centrifuging 10ml of patient venous blood. Part of PRF was mixed with bone graft and the remaining PRF was used to prepare membrane. Mixture of demineralised bone matrix (Osseograft, Encoll,U. S. A) and PRF was packed well into the labial(Fig.11) and palatal defect(Fig.13). Labial defect was covered with PRF membrane (Fig.12). Flaps were approximated and sutured with black silk 3-0 (Mersilk (Ethicon) – Johnson and Johnson pvt Ltd, India) and periodontal dressing was given. Sutures were removed after 2 weeks post operatively and the patient was reviewed at frequent intervals. Post operative review after 8 months revealed obvious reduction in tooth mobility with probing depth of 2mm (Fig.14). Radiograph also revealed satisfactory bone fill around tooth #12 (Fig.15).
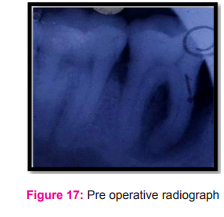
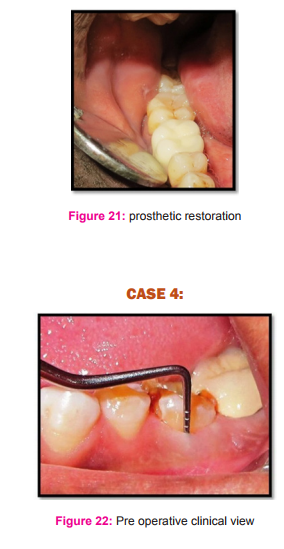
Case 3: Combined lesion
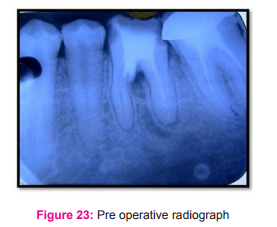
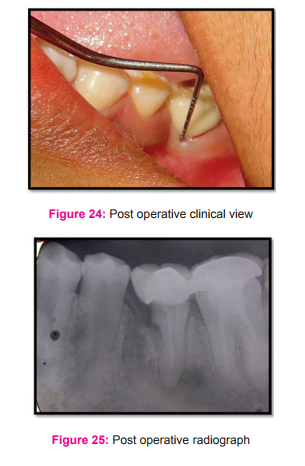
A 45 years old male patient reported to Department of Periodontics with frequent food impaction associated with throbbing pain in relation to #46. On clinical examination, probing depth of 7mm was detected in relation to mesial aspect of #46 along with grade III furcation involvement. Grade III gingival recession in relation to mesial root of #46 was associated with pus discharge and the tooth was found to be non vital on pulp testing (Fig.16). IOPA revealed peri radicular radiolucency in relation to mesial root of #46 (Fig.17). On considering the clinical condition, it was planned for a nonvital hemisection. After phase 1 therapy, patient was referred to Department of Endodontics for endodontic management of 46. On review after three months, surgical management was planned. Under local anesthesia, buccal and lingual full thickness flap was elevated in relation to #46 and thorough degranulation and debridement was done. Tooth was bisected with diamond coated round disc and mesial half of the tooth along with mesial root was completely removed (Fig.18). Socket was curetted well and irrigated with normal saline. Hemostasis was achieved. Flaps were approximated and sutured with 3.0 black silk (Mersilk (Ethicon) – Johnson and Johnson pvt Ltd, India). Post operative wound healing was uneventful (Fig.19 and 20). Prosthetic rehabilitation was done with fixed partial denture prosthesis (Fig.21). Case 4: Iatrogenic Periodontal lesion A 35 years old male patient, referred from Department of Endodontics for periodontal opinion regarding frequent discomfort of a root canal treated tooth. History of root canal treatment in relation to 36 about a year ago and reported with a complaint of frequent discomfort and pain of the same tooth. On clinical examination, a probing depth of 8mm was detected in relation to #36 (Fig.22). IOPA revealed an root canal treated #36 with perforation extending to furcation area along with inter-radicular radiolucency (Fig.23). This case was planned for hemisection of #36 followed by prosthetic rehabilitation (Fig.24 and 25). The treatment of #36 was similar to case 3.
DISCUSSION
In day to day practice, assessment and treatment planning of an endo perio lesion is challenging as it often ends up in dilemma whether to initiate the treatment with endodontic therapy followed by periodontal treatment or only with periodontal therapy or both in most of cases. As a general rule it is often practiced to complete the treatment of the primary disease alone, if the secondary disease has just begin to progress and in cases of combined presentation of primary and secondary disease it is advised to treat both the disease (18-21) . In all the four cases, patient presented with established chronic secondary disease. Hence all the cases were planned to complete the endodontic therapy initially and then proceed with periodontal therapy. In case 1, patient presented with periodontal disease as secondary disease since she had undergone endodontic treatment 6 months ago. The secondary periodontal disease would have not been considered during the endodontic management and hence it has been mistreated leading to gross destruction of the periodontal apparatus (grade 2 furcation involvement) of the affected tooth #36. As there was grade 2 furcation involvement with 8mm periodontal pocket, closed curettage would not have been sufficient and so open flap debridement was done. Bone regeneration at the end of 6 months indicates the success of proper debridement of infection. In case 2, The main etiological factor being Palato radicular groove (PRG), as these grooves acts as pathway of entry of infection into periodontal apparatus and periapical region. Hence it is considered as primary periodontal lesion with secondary endodontic involvement. The primary aim of treatment was to obliterate the groove and end the communication of infection from oral cavity to periodontal structures. Hence open flap debridement was done and groove was restored with glass ionomer cement. Glass ionomer cement was opted due to its biocompatibility, resistance to water degradation at tooth cement interface, better sealing and bonding ability (22,23). Since the defect was a three walled defect with dehiscence of upto 8 mm, the defect was filled with xenografts along with platelet rich fibrin due to its osteoconductive property and better healing. As the etiological factor was removed, a satisfactory periodontal regeneration with bone fill at the end of 8 months was observed. In Case 3 and 4, bone defect involving the mesial root of mandibular first molar with furcation involvement was present. Due to severity of the defect and intention to save the periodontal support of the remaining roots, hemisection with open flap debridement was done for both the cases. Post operative review depicted good soft tissue healing with sound periodontal support which was necessary for prosthetic rehabilitation.
CONCLUSION
Treatment outcome will be more predictable if the clinician has more thorough knowledge about the diagnosis, treatment sequence with inter-disciplinary approach .Thereby the immediate and true management of the endodontic- periodontic lesions can impede the loss of the natural tooth and delay the more complex treatment.
ACKNOWLEDGEMENT
Authors acknowledge the immense help received from the scholar whose articles are cited and included in reference of this manuscript. The authors are also grateful to authors/ editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.



References:
1. Mandel E, Machtou P, Torabinejad M. Clinical diagnosis and treatment of endodontic and periodontal lesions. Quintessence Int. 1993;24:135-9.
2. Jansson L, Ehnevid H, Lindskog S, Blomlöf L. The influence of endodontic infection on progression of marginal bone loss in periodontitis. J ClinPeriodontol 1995;22:729-73.
3. Jansson L, Ehnevid H, Blomlöf L, Weintraub A, Lindskog S. Endodontic pathogens in periodontal disease augmentation. J ClinPeriodontol 1995;22:598-602.
4. Jansson L, Ehnevid H, Lindskog S, Blomlöf L. Relationship between periapical and periodontal status. A clinical retrospective study. J ClinPeriodontol 1993;20:117-23.
5. Turner JH, Drew AH. Experimental injury into bacteriology of pyorrhea, Proc R Soc.Med (Odontol) 1919;12:104.
6. Simring M., Goldberg M.The pulpal pocket approach: retrograde periodontitis, J Periodontol 1964; 35:22.
7. Adriaens PA, de Boever JA, Loesche WJ. Bacterial invasion in root cementum and radicular dentin of periodontally diseased teeth in humans: a reservoir of periodontopathic bacteria. J Periodontol 1988; 59(4):222-230.
8. Adriaens PA, Edwards CA, de Boever JA,Loesche WJ. Ultrastructural observations on bacterial invasion in cementum and radicular dentin of periodontally diseased human teeth. J Periodontol 1988.;59(8): 493-503.
9. Haapasalo M, Ranta H, Ranta K,Shah H. BlackpigmentedBacteroides spp. in human apical Periodontitis.Infect Immun. 1986;53(1):149-153.
10. Trope M, Tronstad L, Rosenberg ES, Listgarten M. Darkfield microscopy as a diagnostic aid in differentiating exudates from endodontic and periodontal abscesses. J Endod. 1988; 14(1); 35-38.
11. Jansson L, Ehnevid H, Bloml¨of L, Weintraub A,Lindskog S. “Endodonticpathogens in periodontal disease augmentation. J Clin Periodontol 1995: 22(8); 598-602.
12. DahleUR, Tronstad L, Olsen I. “Characterization of new periodontal and endodontic isolates of spirachet´es,” Eur J Oral Sci.1996 :104(1); 41-47.
13. .Khalid S. Al-Fouzan. A New Classification of Endodontic-Periodontal Lesions Hindawi Publishing Corporation International Journal of Dentistry Volume 2014, Article ID 919173, 5 pages http://dx.doi.org/10.1155/2014/919173
14. Cohen S, Burns RC. Pathways of the pulp, 4thEdition, 1990;840- 844.
15. Newman, Takei, Carranza, et al. Carranza’sClinical Periodontology, 10th edition, 2007.
16. Lindhe J, Karring T and Lang NP.ClinicalPeriodontology and Implantology, 4th edition, 2003.
17. Walton RE, Torbinejad M. Principles and practice of endodontic, 1st Edition, 1986; 665-667.
18. Richard E Walton and Mahmoud Torabinejad. Principles and Practice of Endodontics. 3rd Edition Philadelphia W B Saunders Company; 2002 pp. 467-84.
19. Rotstein I, Simon JH. Diagnosis, prognosis and decision-making in the treatment of combined periodontal-endodontic lesions. Periodontol 2000 2004;34:165-203.
20. Harrington GW, Steiner DR, Ammons WF. The periodontalendodontic controversy. -Periodontol 2000 2002;30:123-30.
21. Meng HX. Periodontic-endodontic lesions. Ann Periodontol 1999;4:84-9.
22. Maldonado A, Swartz ML, Phillips RW. An in vitro study of certain properties of a glass ionomer cement. J Am DentAssoc 1978; 96: 785-791.
23. Vermeersch G, Leloup G, Delmee M, Vreven J Antibacterial activity of glass-Ionomer cements, compomers and resin composites: relationship between acidity and material setting phase. J Oral Rehabil 2005; 32: 368-374.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License