IJCRR - 13(19), October, 2021
Pages: 23-26
Date of Publication: 11-Oct-2021
Print Article
Download XML Download PDF
Clinical Study of Scleral Fixated Posterior Chamber Intraocular Lens Implantation and its Morbidity
Author: Neha Maheshwari, B.S. Joshi, V H Karambelkar
Category: Healthcare
Abstract:Introduction: Secondary implantation of the intraocular lens in the posterior chamber is a safe and effective option for visual rehabilitation for cases with inadequate capsular support following cataract surgery, subluxation or anterior dislocation of lens following trauma, collagen vascular diseases or pseudoexfoliation. Aim: This study was done to analyze the visual outcomes and complications associated with scleral fixated intraocular lenses. MATERIAL AND METHOD- This prospective study was conducted in Krishna institute of medical sciences Karad from OCTO�BER 2018- MAY 2020 for a period of 18 months.67 patients were included who were diagnosed with surgical aphakia, traumatic aphakia, subluxation of the lens and traumatic dislocation of the lens. All the patients underwent the Ab-external fixation technique of Scleral-fixated intraocular lenses (SFIOL) after informed consent. All the surgeries were performed by the same surgeon. The patients were followed up on the first day, one week, one month and three months after the surgical procedure and Best Corrected visual acuity and postoperative complications were noted. Results: Visual acuity at end of 3 months of follow up showed 74.62% cases had 6/9- 6/12 visual acuity and the remaining had visual acuity between 6/18-6/36 in 20.89% of cases and ≤ 6/60 in 4.48% cases. The immediate postoperative complications were: corneal oedema in 62.69%, followed by striate keratopathy in 11.94% cases, anterior uveitis among 2.99% cases, CME and raised IOP among 1.49% cases each. The late postoperative complication rate was reduced as compared to the early post-operative period. 68.66% had no postoperative complication after 12 weeks. The incidence of CME at the end of 12 weeks was 13.43%. 8.96% cases had raised IOP. Transient anterior uveitis was noted in 2 cases (2.99%). Retinal detachment (RD) was developed in 2.99% of cases. Conclusion: SFIOL is a safe and effective option in cases of inadequate posterior capsular support due to surgery or trauma, providing better visual rehabilitation with decreasing long term complication rates.
Keywords: Glaucoma, Intraocular lens, Posterior chamber, Cataract surgery, Retinal detachment, Ab-externo fixation technique
Full Text:
INTRODUCTION
Implantation of intraocular lenses is the standard procedure done in cataract surgery. Ideally, the lens is placed in the capsular bag (Posterior chamber intraocular lenses), which is close to the nodal point of the eye. However, there are instances where it is not possible to achieve in conditions like congenital (e.g., familial or idiopathic ectopia lentis, Marfan syndrome, etc) and secondary weakness of the lens zonules, type of cataract (e.g., traumatic cataracts with lens subluxation, cataracts in pseudoexfoliative syndrome with zonular/capsular dehiscence) or to intraoperative surgical complications (e.g., large breaks in the posterior capsule or posterior capsular rupture during cataract extraction, accidental aspiration of the capsular bag etc), trauma, lens dislocation, surgeons need to employ a technique to fixate an IOL without the support of capsule. Three principal alternatives for fixation are-
1. Scleral suture-fixated posterior chamber intraocular lenses. (SFIOL).
2. Peripheral iris suture-fixated posterior chamber IOLs.
3. Anterior chamber intraocular lenses. (ACIOL).
Anterior chamber angle supported lenses are close to the cornea and anterior chamber angle, increasing the risk for bullous keratopathy, glaucoma, and peripheral anterior synechiae.1 In absence of capsular support, SFIOLs have become increasingly popular over the past decade. 2 Also SFIOL is an alternative to patients with complications of implanted ACIOL and those with contraindications to ACIOL and iris or angle-related abnormality. In 1986, Malbran and co-authors first reported trans-scleral sulcus fixation of posterior chamber lenses in aphakic patients. 3
Intraocular lens placement in the posterior chamber reduces the risk of various complications like bullous keratopathy, damage to anterior chamber angle, pupillary block glaucoma, iris chafing, hyphema, uveitis, and pseudo phacodonesis. 4
The surgical techniques which are explained for trans scleral sutures to fixate a posterior chamber intraocular lens are Ab interno (inside out) and ab externo (outside-in). 5,6 Ab- interno (inside out) technique involves the passage of sutures from the inside of the eye to the outside whereas the Ab-externo (outside-in) technique involves the passage of a suture from the outside of the eye to the inside. In the Ab-externo method, the intraocular lens placement occurs in the ciliary sulcus and the view of the surgical field is never obscured. The risk of vitreous haemorrhage decreases as all the manipulations occur in the iris plane. 7
MATERIALS AND METHODS
This prospective study was conducted in Krishna institute of medical sciences Karad from OCTOBER 2018- MAY 2020 for 18 months
INCLUSION CRITERIA-
•Patients who underwent scleral fixation of posterior chamber intraocular lens (SFIOL) implantation in the Ophthalmology Department in Krishna hospital, Karad during the study period.
EXCLUSION CRITERIA-
•All anterior segment pathology like central corneal opacity, glaucoma, uveitis etc. affecting the visual outcome.
•All Posterior segment pathologies affecting visual function like macular degeneration, chorioretinal atrophy etc., and complicating the surgery.
•All patients with manifestations of systemic diseases affecting the outcome of surgery.
•Patients who did not come for complete 3 month follow up period.
METHODOLOGY
Patients having a history of eye trauma with capsular bag rupture or complicated cataract surgery causing aphakia and those who completed 3 months follow-up were included in the study.
A standard case proforma was maintained and a detailed clinical history was taken. PREOPERATIVE EVALUATION
1. Uncorrected and best-corrected visual acuity using Snellen’s distance and near visual acuity chart.
2. Slit-lamp biomicroscopic examination-
3. Measurement of IOP in all patients preoperatively.
4. FUNDUS EXAMINATION
5. IOL POWER CALCULATION - using SRK-T formula.
6. B scan and OCT done whenever required.
SURGICAL TECHNIQUE
All the surgeries were performed by the same surgeon. Anaesthesia and akinesia of globe obtained by peribulbar block with a mixture of 2% xylocaine with adrenaline with 2ml of 0.75 % bupivacaine with the addition of hyaluronidase were used. The skin around the eye is painted with 5% povidone-iodine and the same drops instilled topically.
1. After preparing the patient, a superior conjunctival peritomy from 4 o'clock to 10 o'clock position was created.
2. Partial-thickness triangular scleral flap of 3×2 mm at 4 and 10 o'clock positions created.
3. A 7 mm corneal scleral wound was made and a complete anterior vitrectomy was performed.
4. Anterior chamber and retro pupillary space were filled with viscoelastic substance.
5. Using a straight needle with 10-0 polypropylene suture was passed through one end of the sclera bed, 1 mm posterior to the surgical limbus and parallel to the iris until it was visualized through the pupil.
6. A 28 gauge hollow needle was passed through a 4 o'clock sclera bed was used to retrieve the straight needle, via its barrel.
7. Using a sinskey hook the loop of suture was retrieved through the corneoscleral wound.
8. After cutting the loop of the suture, it was tied to superior and inferior eyelets of the haptic of the IOL.
9. The IOL was placed in the sulcus and sutures were gently pulled to secure the position of the lens.
10. A second 10-0 polypropylene suture is used to take a bite just anterior to the original suture exit point in the scleral bed. The long end of the second polypropylene suture is tied to both its short end and the lens-fixing suture.
11. This was repeated at the other end of the scleral bed.
12. The scleral flap and conjunctival peritomy was closed.
Postoperatively patients were treated with topical Moxifloxacin 0.5 % + Dexamethasone 0.1 % eye drops 2 hourly which was gradually tapered.
POSTOPERATIVE EVALUATION-All patients were examined on the next day and were followed up after one week, one month and three months of the surgical procedure.
RESULTS
In the present study, we observed that the majority of the study subjects belonged to the age group of 56 to 65 years (47.76%), followed by 66 to 75 years (20.90%) then 46 to 50 years (14.93%). . Majority of the study subjects were males (58.21%), while 40.30% subjects were females Right eye was affected among 52.24% study subjects, while the left eye was affected among 47.76% subjects.
The majority of the study subjects had preoperative BCVA as indicated in table 1 which was less than 6/60 (41.79%), followed by 6/24 among 38.81% subjects, 6/36 among 14.93% subjects and 6/18 among 4.48% subjects.
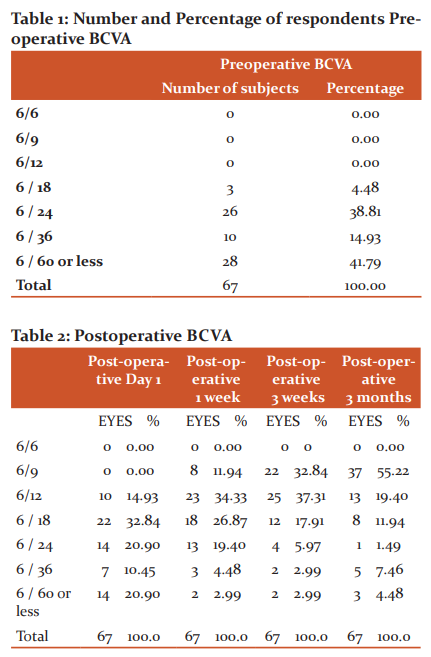
In table 2, Postoperative BCVA has been indicated which was less than 6/18 (32.84%), followed by 6/24 and 6/60among 20.90% subjects, 6/12 among 14.93% subjects and 6/36 among 10.45% subjects.
DISCUSSION
In the present study, all the patients (67) were selected for scleral fixation of posterior chamber intraocular lens (SFIOL) implantation. The mean age of the study subjects was57.39 ± 12.67 years. In the kwong et al. study the mean age of the patients was 76.7 years.8
Our study had 39 males and 27 females. The male to female ratio was 1:0.69. Regarding laterality, both eyes were almost equally affected (35 right eyes and 32 left eyes).
The most common diagnosis at presentation was post-surgical aphakia (65.67%) followed by the subluxated lens (19.41 %), traumatic subluxated lens (10.45%) and traumatic aphakia (5.98%). No studies have been found that included all the above inclusion criteria for SFIOL implantation.
In our study, all the post-surgical aphakia patients had undergone secondary procedures and all the traumatic patients had undergone primary procedures. In Lee et al study there were 30(54.5%) in the primary group and 25(45.5%) in the secondary SFIOL group8.In 39 patients the pre-operative visual acuity was between 6/36 to 6/18 and 28 patients had visual acuity of 6/60 and less. The mean duration of SFIOL implantation was 60 minutes. In Kwong et al. study the mean duration was 65min (SD±24.12 min).7,8,9
The Kh value pre-operative and post-operative was analyzed using the paired t-test and the p-value was significant (P = 0.0008). The analysis of Kv value pre-operatively and post-operative showed significant change and the p-value was significant (P= 0.00001). The mean pre-operative astigmatism was 1.29 ± 1.47, while the mean postoperative astigmatism was 1.76 ± 1.50. The analysis of mean corneal astigmatism pre and post-operative was found to be significant (p=0.00107).
Preoperatively, the majority of the cases had WTR astigmatism (43.28%), followed by ATR astigmatism (34.33%), OBL astigmatism (16.42%). Postoperatively we observed that 44.78% cases had WTR astigmatism, 32.84% cases had ATR astigmatism, and 13.43% had OBL astigmatism. The conversion of one type of astigmatism into another type was noted but the average percentage of the various types of corneal astigmatism has not altered much.
Postoperatively BCVA after 1 week was improved to6/9 – 6/ 12 among 46.27% cases followed by 6/18- 6/ 36 among 50.75 cases and≤ 6/60 observed among 20.99 % cases. At 12 weeks 74.62 cases had 6/9- 6/12 visual acuity and the remaining had visual acuity between 6/18-6/36 in 20.89% of cases and ≤ 6/60 in 4.48% cases. The improvement in visual acuity after 12 weeks of follow up is due to treatment of associated complications.
The immediate post-operative period was uneventful in 17.91% of cases. The immediate postoperative complications were: corneal oedema among 62.69%, followed by striate keratopathy among 11.94%, anterior uveitis among 2.99%, CME and raised IOP among 1.49% cases each.
68.66% had no postoperative complication after 12 weeks. The incidence of CME and ERM at the end of 12 weeks was 13.43% and 1.49% respectively which were treated medically. These cases were associated with vitreous loss either at the initial event with the loss of capsular support or during scleral fixation. Another contributing factor for the development of CME is light-induced retinal injury due to the increased operating time.10
Increased IOP was noted in 6 cases (8.96%) for 1 week and was controlled with antiglaucoma drugs.11 While doing scleral fixation of IOL, transient anterior uveitis was noted in 2 cases (2.99%) which was treated with steroids and topical cycloplegics. 2 cases (2.99%) had developed Retinal detachment 3 months postoperatively due to too posterior placement of suture fixation and underwent RD surgery. None of the patients had major complications like endothelial decompensation, suprachoroidal or vitreous haemorrhage, dislocation of IOL/ IOL tilt or endophthalmitis.
CONCLUSION
In our study, we have noted that the rate of complications in the late postoperative period (>3 months after surgery) and found that the complication rate was reduced as compared to the early postoperative period. SFIOL to conclude is a safe and effective option in cases of inadequate posterior capsular support due to surgery or trauma, providing better visual rehabilitation with decreasing long term complication rates.
Acknowledgement: We acknowledge the contribution of our university and department for the unending support.
Conflict of Interest: There is no conflict of Interest
Source of Funding: No Source of Funding
Authors Contribution: This is a collaborative work among all authors. Neha Maheshwari B.S Joshi, V H Karambelkar, performed the statistical analysis, wrote the protocol, and wrote the first draft of the manuscript. Neha Maheshwari managed the literature searches. All the authors read and approved the final manuscript.
References:
1. Lorente R, de Rojas V, de Parga PV, Moreno C, Landaluce ML, Domínguez R, Lorente B. Management of late spontaneous in-the-bag intraocular lens dislocation: retrospective analysis of 45 cases. J Cataract Refract Surg. 2010 Aug 1;36(8):1270-82.
2. Peyman GA. Vitreoretinal surgical techniques. Routledge; 2019 Jul 12.
3. Malbran ES, Malbran E, Negri I. Lens guide suture for transport and fixation in secondary IOL implantation after intracapsular extraction. Int Ophthalmol. 1986 May 1;9(2-3):151-60.
4. Brunin G, Sajjad A, Kim EJ, de Oca IM, Weikert MP, Wang L, Koch DD, Al-Mohtaseb Z. Secondary intraocular lens implantation: complication rates, visual acuity, and refractive outcomes. J Cataract Refract Surg. 2017 Mar 1;43(3):369-76.
5. Can E, Ba?aran MR, Gül A. Scleral fixation of a single-piece multifocal intraocular lens. Eur J Ophthalmol. 2013 Mar;23(2):249-51.
6. Rau R, Santana CR, Martinez AA, Silva AL, Allemann N. Positioning of intraocular lens haptics intentionally implanted in the ciliary sulcus by ultrasound biomicroscopy. Arquivos brasileiros de oftalmologia. 2013 Jun;76(3):147-51.
7. Seki M, Yamamoto S, Abe H, Fukuchi T. Modified ab externo method for introducing 2 polypropylene loops for scleral suture fixation of intraocular lenses. J Cataract Refract Surg. 2013 Sep 1;39(9):1291-6.
8. Kwong YY, Yuen HK, Lam RF, Lee VY, Rao SK, Lam DS. Comparison of outcomes of primary scleral-fixated versus primary anterior chamber intraocular lens implantation in complicated cataract surgeries. Ophth. 2007 Jan 1; 114(1):80-5.
9. Chan TC, Lam JK, Jhanji V, Li EY. Comparison of outcomes of primary anterior chamber versus secondary scleral-fixated intraocular lens implantation in complicated cataract surgeries. Am. J. Ophthalmol. 2015 Feb 1; 159(2):221-6.
10. Ceballos EM, Parrish II RK, Schiffman JC. The outcome of Baerveldt glaucoma drainage implants for the treatment of uveitic glaucoma. Ophthalm. 2002 Dec 1; 109(12):2256-60.
11. Collins JF, Gaster RN, Krol WF, Colling CL, Kirk GF, Smith TJ, VA Cooperative Cataract Study Group. A comparison of the anterior chamber and posterior chamber intraocular lenses after the vitreous presentation during cataract surgery: the Department of Veterans Affairs Cooperative Cataract Study. Am. J. Ophthalmol.. 2003 Jul 1;136(1):1-9.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License