IJCRR - 13(11), June, 2021
Pages: 219-226
Date of Publication: 04-Jun-2021
Print Article
Download XML Download PDF
Iatrogenic Effects of Orthodontic Treatment-A Review
Author: Anusha S, Navaneetha N, Piradhiba R, Veerasankar S
Category: Healthcare
Abstract:Introduction: Orthodontic treatment aids in the improvement of function, esthetics, and the patients' self-confidence. Iatrogenic damage during orthodontic treatment is believed to have deleterious effects on the dentition &periodontium. The complications associated with orthodontic treatment are a result of a multifactorial process including the patient's biology, clinical skills of the orthodontist, orthodontic appliances, orthodontic treatment procedures, and length of treatment. Aim: The purpose of this study is to summarize the scientific-based evidence on the iatrogenic effects that may be associated with orthodontic treatment and thereby discuss methods of prevention by reviewing various articles published under this topic. Methodology: The database collected from PubMed, PubMed Central (PMC), Cochrane library, Google scholar and research gate were studied and thus all available information has been reviewed and briefed in this article. Discussion and Conclusion: If the orthodontic treatment is to be beneficial, the advantages it offers should outweigh any pos�sible damage it may cause. It is important to assess the risks of treatment as well as the potential gain and balance these aspects of treatment before deciding how to treat the malocclusion. Further studies and controlled trials on the aetiology and intensity of each effect concerning every influencing factor are required.
Keywords: Orthodontics, Iatrogenic, Resorption, Hypersensitivity, Allergy, Demineralisation
Full Text:
INTRODUCTION
Orthodontic treatment is being practiced since the 1800s and the benefits gained are voluminous like improvement in dental health, function, appearance, and self?esteem.Although orthodontic treatment has many such recognized benefits, orthodontic appliances can cause unwanted complications if adequate care is not taken during the treatment.1
Iatrogenic is derived from the Greek word “iatros” meaning physician and “gen” meaning ‘producing’. Identifying the risk factors, causes, and ways to prevention is important for a successful orthodontic treatment and the oral health of the patient. Adequate knowledge on these complications has to be imparted to the patient and necessary counselling on his role in avoiding these have to be given. There is less literature on the consolidated review of all the observed iatrogenic effects and ways to prevent them during orthodontic treatment. This review article aims to discuss various iatrogenic effects of orthodontic treatment and ways to avoid the occurrence of these for a successful orthodontic treatment.2
WHITE SPOT LESION
The white spot lesion (WSL) has been defined by Fejerskov et al. as the first sign of caries-like lesion on enamel that can be detected with the naked eye.1 Enamel decalcification in the form of white spot lesions is a consequence of improper oral hygiene while undergoing orthodontic treatment ( Fig 1). They appear as small lines along the bracket periphery or as large decalcifications with or without cavitations.2

Fig. 1: Facial surface of maxillary anterior teeth.
(Photo courtesy: Chapman et al, Risk factors for incidenceand severity of white spot lesions during treatment withfixed orthodontic appliances. , AJODO 2010)
A sudden increase in the number of WSLs occurred during the first 6 months of treatment and continued to increase at a slower rate to 12 months, thus maintaining proper oral hygiene is critical in the initial months of the treatment.3 According to Oggard et al.,1988 the occurrence of WSLs in orthodontically treated patients was maximum in lateral incisors followed by canines, first premolars, 2nd premolars, and central incisors. The incidence rate is 45.8% and the prevalence rate is 50%–96% in patients undergoing orthodontic treatment, which is quite alarming.4, 5
Diagnosis: There are various methods to identify which include visual inspection, photographs, fluorescent methods, and optical modalities such as diagnosed, quantitative light-induced fluorescence, and digital image fibre-optic transillumination. Benson et al., 2003 considers quantitative laser techniques as more sensitive, yielding a higher prevalence rate than the simple visual technique.6, 7
Prevention and management
a) Maintain Oral Hygiene: Mechanical plaque control by proper tooth brushing, interdental brush, disclosing solutions, floss, water irrigation or powered toothbrush can be used8.
b) Fluoride Toothpaste: Fluoride toothpaste contains sodium fluoride, monofluorophosphate or stannous fluoride (1500-5000 ppm) where fluoride ions get incorporated into the surface of enamel forming fluorapatite crystals. Sonesson et al., proves that they reduced the incidence of WSL by 32%.9, 10
c) Fluoride Mouth rinse: Fluoridated mouth rinses containing 0.05% sodium fluoride used daily or every other day reduced WSL by 25%. Antibacterial agents like chlorhexidine, triclosan, or zinc have been incorporated into these mouthwashes to improve their cariostaticeffects.10,11, 12.
d) Fluoride Varnish: Varnishes adhere to the enamel surface longer than other topical fluoride products and do not require patient compliance. 5% NaF forms a reservoir of calcium fluoride on the tooth surface and prevents demineralization by 30- 50% when applied biannually.13, 14,15
e) Fluoride Releasing Banding Cement
Resin Modified Glass Ionomer Cement (RMGIC) pumps fluoride by absorbing from the environment and releasing it in the most susceptible areas.16 Bishara et al. reported a very less initial bond strength of RMGIC with a failure rate of 24.8%.17, 18
Bioactive glass (BAG) is a cross-linked matrix of hydrolyzed alkoxides of SiO2 and CaO that releases ions such as calcium, fluoride into the oral environment and prevents demineralization of enamel. Manfred et al. showed that BAG-Bond adhesives have better microhardness than Transbond-XT.19
f) Elastomeric ligatures: Tin fluoride (SnF) containing elastomeric ligature ties release a low concentration of fluoride for a long period. Wiltshire et al., 1996 reported an initial burst of fluoride-release (35%) during the first 24 hours followed by a continued release of 63%, 83%, and 88% of the total fluoride in the first week, first month, and second month, respectively.20,21
g) Pit and fissure sealants: The application of resin sealants on the enamel surface surrounding the bracket protects the enamel surface from acid attack. Benham et al. reported a decrease in WSL by 3.8 times with sealants.22, 23 Sealant combined with brushing was more effective in protecting enamel than brushing alone.24
h) Xylitol: Xylitol is a polyol (a type of carbohydrate) that is not metabolized by S mutants and can be used as a sugar substitute. It is available as chewing gum or lozenges.25 Xylitol lozenges reduce the acidogenicity of dental plaque by increasing the pH value.26
i) Laser irradiation: Laser irradiation is a new method for inhibiting demineralization around orthodontic appliances which is regularly combined by fluoride therapy. Meurman et al showed that it is possible to convert hydroxyapatite crystals to fluorapatite crystals instantly in the presence of fluoride using a CO2 laser. 27
j) Intraoral fluoride-releasing devices: Copolymer Membrane Device, Glass Device Continuing Fluoride, Slow-Fluoride Release Tablets. These devices can significantly increase the salivary fluoride concentration without substantially affecting the urinary fluoride levels.28
ROOT RESORPTION
External apical root resorption (EARR) is defined as a physiologic or pathological process characterized by the loss of cementum or dentine resulting in the shortening of the root apex29. When heavy orthodontic forces are applied for a long duration (weeks or months), necrosis (hyalinization) of the compressed PDL may occur. The defensive leukocytes that migrate out of PDL capillaries include osteoclast progenitors that promptly coalesce to form multinucleated cells, capable of resorbing mineralized tissues (bone and tooth roots).30
Stages of root resorption, as proposed by Levander and Malmgren, which was further modified by Beck and Harris in 1994 ( Fig 2).31
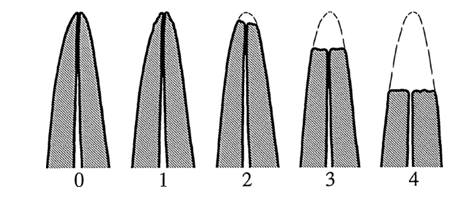
Fig. 2: Root resorption index acc. to Malmgrenet al., 1982
Root resorption after orthodontic treatment of traumatized teeth. AJO. 1982
(Grade 0: Normal root length
Grade 1: Irregular root contour
Grade 2: Root loss apically, <2mm
Grade 3: Root loss apically, 2mm to 1/3rd root length
Grade 4: Root loss exceeding 1/3rd of root length)
Krishnan et al., reported a genetic influence in those individuals homozygous for IL-1β(+3953) allele 1 where the risk of root resorption increased by 5.6-fold.30
Maxillary teeth are more sensitive than mandibular teeth as their extent of movement is greater and their root structure and periodontium tend to transfer the forces mainly to the apex. The use of fixed appliances is more detrimental to the roots than removable appliances.32 The use of elastics that give jiggling forces, rapid maxillary expansion with cervical traction, has been reported to cause severe root resorption of the first maxillary molars.33, 34 Intrusion is the most damaging to the roots involved.35 Agap in treatment with intermittent forces permits the resorbed cementum to restore and avoids further resorption.36
In the view of accelerated orthodontics, which mainly acts by RAP (Regional Acceleratory Phenomenon), the inflammatory markers (cytokines) activate the cementoblasts and it increases the chance of root resorption.37
Diagnosis: Several radiographic techniques used include periapical radiograph, orthopantomogram, cephalogram, and laminogram as it provides the most appropriate information with the least irradiation to the patient.32
Prevention and management: Clinical considerations30, 32
-
Frequent periapical radiographs, at least every year during active treatment
-
The orthodontic force should be for a short duration, intermittent and minimal.
-
Traumatized teeth should be treated with utmost care since they are more prone to root resorption.
-
Eliminate pressure habits
-
Occlusal traumatism and jiggling are detrimental to the roots
-
If any root resorption is found, an inactive phase of 4 to 6 months before resuming orthodontic treatment is advised. In extreme cases, an interdisciplinary approach is adopted35.
DENTIN HYPERSENSITIVITY
Injudicious use of interproximal reduction (IPR) can result in hypersensitivity. IPR is done to manage tooth mass discrepancy, late secondary crowding problems, prevent relapse by stabilizing dental contacts over the long-term, and eliminate black triangles in periodontal patients and reshaping the canines in congenitally missing lateral incisors. Around 0.2mm- 0.6mm can be removed from the mesiodistal surfaces of the teeth based on the tooth. The air-rotor with fine tungsten-carbide or diamond burs/ disks and abrasive metal strips are used38.
Hypersensitivity depends on various factors such as the age of the patient, severity of crowding, pathological tooth wear, hypersensitivity before treatment, and the amount of the enamel removed.39 The sensitivity is mild, transient and the symptoms usually subside over time40.
Prevention and management
Identifying the thickness of enamel by projecting a line from the cervical line vertically to the occlusal plane because dentin is projected in a straight line from the cervical line or using special gauges, aligning the rotated teeth before striping, finishing and polishing with superfine strips, using a fluoride mouth rinse or denitrifies, or professional interventions through the application of fluoride varnish to promote remineralization can be done.41- 43
PERIODONTAL PROBLEMS
Orthodontic appliances interfere with oral hygiene procedures and contribute to plaque accumulation.44 Vanarsdall et al. observed that the gingival changes associated with orthodontic appliances are transient and they resolve themselves or will respond to professional oral prophylaxis measures. Gingival recession is the exposure of root surfaces due to apical migration of the gingival tissue margins.45 Marginal tissue recession or attachment loss is associated with thermal and tactile sensitivity, esthetic complaints, and root caries.46
Morris et al. reported that orthodontic treatment is not a major risk factor for the development of gingival recession. However, larger amounts of maxillary expansion may increase the risk of recession after treatment.47
Prevention and management
When pre-existing gingival recessions are found before orthodontic treatment, the impact of orthodontic treatment should be carefully evaluated. If the tooth is planned to move lingually, tooth movement alone can end up treating or at least not aggravating the recession. If the tooth is to be moved labially, a mucogingival procedure to avoid disease progression must be planned. OTM may be initiated once wound healing is complete (3-4 months). When a gingival recession occurs during tooth movement, soft tissue grafting is indicated and is performed as soon as possible. Orthodontic therapy should be carefully evaluated to determine whether to stop or slow down OTM until wound healing is complete48.
6. BLACK TRIANGLE
Open gingival embrasures, also known as black triangles, refer to space below the interproximal contact when space is not filled with gingiva. They cause esthetic and periodontal problems related to chronic food retention.2 Adult orthodontic patients show a relatively high incidence of 38 to 43.7% of open gingival embrasures despite their high esthetic demands( Fig 3).49

Fig. 3: Black triangle
(Photo courtesy: Pugliese F et al., Black triangles:
Preventing their occurrence, managing them whenprevention is not practical.
Semin.Orthod. 2019)
Ageing, thin periodontal biotype, increased distance from the contact point to the alveolar bone, divergent or triangular shaped crown forms, incisively placed interproximal contact, root angulation a (1° increase in root divergence increased the odds of an open gingival embrasure by 14- 21%) pose a major risk factor for the black triangle.50 Burke reported that a black triangle is a consequence of aligning crowded maxillary central incisors. One-third of orthodontic patients are likely to have crowded central incisors, of which two-fifths of them are likely to have a post-orthodontic black triangle.51
Prevention and management
Periodontal management by papilla preservation or papillae regeneration with soft tissue graft can be advised. Restorative approaches to change the shape of the crown. Orthodontic treatment to converging roots of central incisors (normal gingival embrasures converges at 3.65°) and restorative approaches by reshaping the triangular crown shape results with reduction of interproximal enamel (IPR) using diamond strips or discs (0.5- 0.75 mm of enamel is removed with IPR).52
SOFT TISSUE INJURY
Intraoral appliances:
Patients may have mouth ulcers, due to pricking of wires, bands, brackets or, cleats on the lips and cheeks. Oral tissues rapidly adjust to the new appliance and in the meantime, vegetable wax can be used to give temporary relief. Sometimes, palatal/ lingual bars may cause trauma to the palate or tongue. Some patients damage their appliances frequently, they are counselled about diet and habits and extra precautions such as placing bands rather than bonds are taken.53
Extraoral appliances:
In 1975 the American Association of Orthodontists reported in an editorial that they come across several rare situations in which patients undertaking extraoral traction appliances had sustained facial injuries.54
The extraoral injuries involve the cheeks, chin and, eye. Injury from headgear is the most common and is commonly due to:
-
Accidental disengagement when the child was playing while wearing the headgear
-
Incorrect handling by the child during the fitting or removal of the headgear
-
Deliberate disengagement of the headgear caused by another child
-
Unintentional disengagement or detachment of the headgear during sleep
The current safety devices available to counter injuries are safety release or snap-away head caps/neckstraps, plastic safety neck straps, and several designs of safety face-bows. They should be given both verbal and written safety instructions after fitting headgear.54, 55 Micro implant injuries
Micromplants are commonly used in absolute anchorage cases. Ellis and Benson discussed the most frequent complications and accidents are the contact between adjacent tooth roots, mucositis, contamination, and mini-implant fracture during placement or removal. Inflammation of soft tissues (poor oral hygiene and implants on free gingiva) around the mini-implant is a possible complication for TADs, which may lead to loss of stability ( Fig 4).53
Gingival soft tissue thickness must be considered when choosing the most appropriate type of mini-implant and incomplete engagement into the cortical bone during placement leads to miniscrewslippage.56, 57
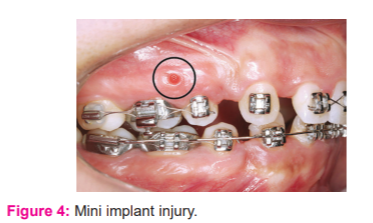
Fig. 4: Mini implant injury
Photo courtesy: Consolaro et al., Reasons for mini-implants failure: choosing installation site should be valued!. Dental Press J Orthod. 2014
Due to accelerated orthodontics
Of all the available techniques for accelerated orthodontics, corticototmy is known to double the rate of tooth movement58. Even though Wilko brothers claim it to be a routine periodontal procedure, surgery-assisted techniques are invasive with bone loss, postoperative pain, swelling, infection, avascular necrosis, and moderate morbidity.59, 60
Ingestion of appliance components
Accidental ingestion or inhalation of foreign bodies in orthodontics range from brackets, bands, buccal tubes, lingual arches and quad-helix, removable appliance fragments, sectional archwire fragments, coil springs, expansion appliance keys, and retainers.61
When a foreign object is lost at the back of the mouth, it is expected to pass through the gastrointestinal tract, rather than the respiratory tract. The British Orthodontic Society advises that any object ingested that is smooth, flexible and, less than 5 cm in length passes through the GIT uneventfully, whilst larger objects are more prone to obstruct or perforate the GIT.62
Prevention61-64
-
Identifying at-risk patients during history taking
-
Ensuring high-speed suction and appropriate barrier techniques such as rubber dam, gauze, or cotton wool rolls.
-
Small orthodontic components can be protected from ingestion by attaching floss or wax.
-
Appliances, both fixed and removable, should be retentive.
-
Every removable appliance should have a radio-opaque component and should be without any sharp edges.
-
An upright position can be used instead of a supine position for some patients and procedures.
-
Unsupportedarchwires should be supported with sleeves or tubing.
Any missing appliance or component is checked for at each visit. Acting immediately to retrieve the foreign body clinically, and using radiological data in deciding to retrieve or observe.
Due to aligners
With the advances in 3D printing and manufacturing, aligners is an emerging technology to treat malocclusions65. Even though they showed a reduced incidence of root resorption, the treatment outcome showed no difference.66, 67 On analysing the MAUDE (Manufacturer and User Facility Device Experience) database, serious adverse clinical events- e.g., difficulty in breathing, swollen throat, anaphylactic reaction, swollen lips, laryngospasm, blisters could be associated with the use of Invisible aligner systems.68
ALLERGY
An allergic response is one in which the immune system of our body reacts extremely to a foreign substance. Two key allergic reactions have been described in the literature. A delayed hypersensitivity reaction (Type IV) is an allergic immune reaction manifesting primarily through T cells (Cellular immunity).69
Allergy in patients undergoing orthodontic treatment can be due to several reasons and these include nickel allergy, allergy to the acrylic resins that are used during treatment, latex products, etc.
Nickel
Nickel alloys are widely used in an orthodontic practice in the form of brackets, wires, bands, and other components. Signs and symptoms of nickel allergy include gingivitis, gingival hyperplasia, lip desquamation, burning sensation in the mouth, metallic taste, angular cheilitis, and periodontitis ( Fig 5).69, 70
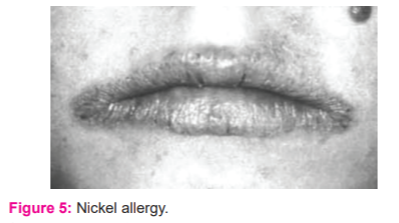
Fig. 5: Nickel allergy
(Photo courtesy: Staerkjaeret al., Nickel allergy and orthodontic treatment. EJO 1990)
Kim et al. suggested in such patients stainless steel, titanium molybdenum alloy, fibre-reinforced composite wires, gold plated wires, ion-implanted nickel-titanium archwires, or plastic/resin-coated nickel-titanium archwires can be used71. Ceramic brackets or even plastic aligners are a good alternative. Extra-oral metal components like headgear studs can be replaced with plastic coated studs72.
Latex
Natural rubber latex is found in gloves, intra and extra-oral elastics, separators, elastomeric modules, elastomeric power chains, polishing rubber cups. Severe systemic reactions, involving the skin, airways, and/ or cardiovascular systems, have been reported after cutaneous and respiratory exposure73.
A definitive diagnosis should be based on the previous medical history and a positive skin reaction to the particular chemicals present in natural rubber latex. In the latex-sensitive patient, stainless steel ligatures, self-ligating brackets and, self-locking separating springs may be preferred. Synthetic non-latex gloves made from nitrile, polychloroprene are available as an alternative.
Acrylic resin
Acrylic re
References:
-
Hunt O, Hepper P, Johnston C, Stevenson M, Burden D. Professional perceptions of the benefits of orthodontic treatment. Eur J Orthod. 2001 Jun;23(3):315-23
-
Meeran NA. Iatrogenic possibilities of orthodontic treatment and modalities of prevention. J Orthod Sci. 2013 Jul;2(3):73-86.
-
Chapman JA, Roberts WE, Eckert GJ, Kula KS, González-Cabezas C. Risk factors for incidence and severity of white spot lesions during treatment with fixed orthodontic appliances. Am J Orthod Dentofacial Orthop. 2010 Aug;138(2):188-94
-
Ogaard B, Rølla G, Arends J. Orthodontic appliances and enamel demineralization. Part 1. Lesion development. Am J Orthod Dentofacial Orthop. 1988 Jul;94(1):68-73
-
Mitchell L. Decalcification during orthodontic treatment with fixed appliances--an overview. Br J Orthod. 1992 Aug;19(3):199-205
-
Julien KC, Buschang PH, Campbell PM. Prevalence of white spot lesion formation during orthodontic treatment. Angle Orthod. 2013 Jul;83(4):641-7
-
Benson PE, Pender N, Higham SM. Quantifying enamel demineralization from teeth with orthodontic brackets--a comparison of two methods. Part 2: validity. Eur J Orthod. 2003 Apr;25(2):159-65
-
Harvey WJ, Powell KR. Care of dental enamel for the orthodontic patient. AustOrthod J. 1981 Dec;7(2):70-6. PMID: 6956324.
-
Zabokova-Bilbilova E, Popovska L, Kapusevska B, Stefanovska E. White spot lesions: prevention and management during the orthodontic treatment. Pril (MakedonAkadNaukUmet Odd Med Nauki). 2014;35(2):161-8
-
Sonesson M, Twetman S, Bondemark L. Effectiveness of high-fluoride toothpaste on enamel demineralization during the orthodontic treatment-a multicenter randomized controlled trial. Eur J Orthod. 2014 Dec;36(6):678-82
-
Geiger AM, Gorelick L, Gwinnett AJ, Benson BJ. Reducing white spot lesions in orthodontic populations with fluoride rinsing. Am J OrthodDentofacialOrthop. 1992 May;101(5):403-7
-
Chadwick BL, Roy J, Knox J, Treasure ET. The effect of topical fluorides on decalcification in patients with fixed orthodontic appliances: a systematic review. Am J OrthodDentofacialOrthop. 2005 Nov;128(5):601-6; quiz 670.
-
Arends J, Lodding A, Petersson LG. Fluoride uptake in enamel. In vitro comparison of topical agents. Caries Res. 1980;14(6):403-13
-
Todd MA, Staley RN, Kanellis MJ, Donly KJ, Wefel JS. Effect of a fluoride varnish on demineralization adjacent to orthodontic brackets. Am J OrthodDentofacialOrthop. 1999 Aug;116(2):159-67
-
Demito CF, Rodrigues GV, Ramos AL, Bowman SJ. Efficacy of a fluoride varnish in preventing white-spot lesions as measured with laser fluorescence. J ClinOrthod. 2011 Jan;45(1):25-9; quiz 40
-
Wilson RM, Donly KJ. Demineralization around orthodontic brackets bonded with resin-modified glass ionomer cement and fluoride-releasing resin composite. Pediatr Dent. 2001 May-Jun;23(3):255-9
-
Bishara SE, VonWald L, Olsen ME, Laffoon JF. Effect of time on the shear bond strength of glass ionomer and composite orthodontic adhesives. Am J OrthodDentofacialOrthop. 1999 Dec;116(6):616-20. doi: 10.1016/s0889-5406(99)70195-2
-
Gaworski M, Weinstein M, Borislow AJ, Braitman LE. Decalcification and bond failure: A comparison of a glass ionomer and a composite resin bonding system in vivo. Am J OrthodDentofacialOrthop. 1999 Nov;116(5):518-21
-
Manfred L, Covell DA, Crowe JJ, Tufekci E, Mitchell JC. A novel biomimetic orthodontic bonding agent helps prevent white spot lesions adjacent to brackets. Angle Orthod. 2013 Jan;83(1):97-103.
-
Viriyakosol, Nuttachai&Dechkunakorn, Surachai&Anuwongnukroh, Niwat&Tua-ngam, Peerapong&Wichai, Wassana. An Investigation of Fluoride Release from Orthodontic Elastomeric Ligatures. Advanced Materials Research. 2014;1025-1026:787-791
-
Wiltshire WA. Determination of fluoride from fluoride-releasing elastomeric ligature ties. Am J OrthodDentofacialOrthop. 1996 Oct;110(4):383-7
-
Silverstone LM. Fissure sealants. Laboratory studies. Caries Res. 1974;8(1):2-26
-
Benham AW, Campbell PM, Buschang PH. Effectiveness of pit and fissure sealants in reducing white spot lesions during orthodontic treatment. A pilot study. Angle Orthod. 2009 Mar;79(2):338-45
-
PithonMatheusMelo, Santos Mariana de Jesus, Souza Camilla Andrade de, LeãoFilho Jorge César Borges, Braz Ana Karla Souza, Araujo Renato Evangelista de et al . Effectiveness of fluoride sealant in the prevention of carious lesions around orthodontic brackets: an OCT evaluation. Dental Press J. Orthod. [Internet]. 2015 Dec; 20( 6 ): 37-42
-
Guzmán-Armstrong S, Chalmers J, Warren JJ. Ask us. White spot lesions: prevention and treatment. Am J OrthodDentofacialOrthop. 2010 Dec;138(6):690-6
-
Sengun A, Sari Z, Ramoglu SI, Malkoç S, Duran I. Evaluation of the dental plaque pH recovery effect of a xylitol lozenge on patients with fixed orthodontic appliances. Angle Orthod. 2004 Apr;74(2):240-4
-
Meurman JH, Hemmerlé J, Voegel JC, Rauhamaa-Mäkinen R, Luomanen M. Transformation of hydroxyapatite to fluorapatite by irradiation with high-energy CO2 laser. Caries Res. 1997;31(5):397-400
-
Gambhir RS, Kapoor D, Singh G. Singh J, Kakar H. Intraoral Fluoride-Releasing Devices: A literature review. World J Dent 2012;3(4):350-354
-
Ne RF, Witherspoon DE, Gutmann JL. Tooth resorption. Quintessence Int. 1999 Jan;30(1):9-25.
-
Krishnan V. Root Resorption with Orthodontic Mechanics: Pertinent Areas Revisited. Aust Dent J. 2017 Mar;62 Suppl 1:71-77
-
Malmgren O, Goldson L, Hill C, Orwin A, Petrini L, Lundberg M. Root resorption after orthodontic treatment of traumatized teeth. Am J Orthod. 1982 Dec;82(6):487-91.
-
Brezniak N, Wasserstein A. Root resorption after orthodontic treatment: Part 2. Literature review. Am J OrthodDentofacialOrthop. 1993 Feb;103(2):138-46
-
Linge BO, Linge L. Apical root resorption in upper anterior teeth. Eur J Orthod. 1983 Aug;5(3):173-83.
-
Hill FJ. Iatrogenic root resorption of upper first permanent molars associated with orthodontic treatment. Report of a case. Br J Orthod. 1987 Apr;14(2):109-13.
-
Stenvik A, Mjör IA. Pulp and dentine reactions to experimental tooth intrusion. A histologic study of the initial changes. Am J Orthod. 1970 Apr;57(4):370-85
-
Oppenheim A. Human tissue response to orthodontic intervention of short and long duration, American Journal of Orthodontics and Oral Surgery. 1942 May;28(5):263-301
-
Frost HM. The regional acceleratory phenomenon: a review. Henry Ford Hosp Med J. 1983;31(1):3-9
-
Koretsi V, Chatzigianni A, Sidiropoulou S. Enamel roughness and incidence of caries after interproximal enamel reduction: a systematic review. OrthodCraniofac Res. 2014 Feb;17(1):1-13.
-
Baysal A, Uysal T, Usumez S. Temperature rise in the pulp chamber during different stripping procedures. Angle Orthod. 2007 May;77(3):478-82.
-
Sikorska-Bochi?ska J, Jamroszczyk K, ?agocka R, Lipski M, Nowicka A. Ocenawrazliwo?cizebinyposzlifowaniupionowymszkliwa [Dentinal hypersensivity after vertical stripping of enamel]. Ann Acad Med Stetin. 2009;55(2):65-7. Polish
-
Jadhav S, Vattipelli S, Pavitra M. Interproximal enamel reduction in comprehensive orthodontic treatment: a review. Indian J Stomatol. 2011;2(4):245- 8.
-
Nanda R. Biomechanics and esthetic strategies in clinical orthodontics. St. Louis, Mo.: Elsevier Saunders; 2005
-
Radlanski RJ, Jäger A, Schwestka R, Bertzbach F. Plaque accumulations caused by interdental stripping. Am J Orthod Dentofacial Orthop. 1988 Nov 1;94(5):416-20.
-
Genco RJ, Borgnakke WS. Risk factors for periodontal disease. Periodon. 2000. 2013 Jun;62(1):59-94.
-
Graber TM, Vanarsdall RL. Orthodontics: current principles and techniques. 4th ed. St. Louis: Elsevier Mosby; 2005;p.1161-62.
-
Robert L. Vanarsdall. Periodontal problems associated with orthodontic treatment. Ame Acad Pedodontics. 1981;3, Special Issue
-
Morris JW, Campbell PM, Tadlock LP, Boley J, Buschang PH. Prevalence of gingival recession after orthodontic tooth movements. Am J Orthod Dentofacial Orthop. 2017 May;151(5):851-859.
-
Gorbunkova A, Pagni G, Brizhak A, Farronato G, Rasperini G. Impact of orthodontic treatment on periodontal tissues: a narrative review of multidisciplinary literature. Int J Dent. 2016 Jan 19;2016.
-
Kurth JR, Kokich VG. Open gingival embrasures after orthodontic treatment in adults: prevalence and aetiology. Am J Orth Dentofacial Orthoped. 2001 Aug 1;120(2):116-23.
-
Pugliese F, Hess R, Palomo L. Black triangles: Preventing their occurrence, managing them when prevention is not practical. In Seminars in Orthodontics 2019 Jun; 25(2, pp. 175-186). WB Saunders.
-
Burke S, Burch JG, Tetz JA. Incidence and size of pretreatment overlap and posttreatment gingival embrasure space between maxillary central incisors. American J Orthod Dentof Orthoped. 1994 May 1;105(5):506-11.
-
Kolte R, Kolte A, Mahajan A. Assessment of gingival thickness with regards to age, gender and arch location. J Ind Society of Periodon. 2014 Jul;18(4):478.
-
Ellis PE, Benson PE. Potential hazards of orthodontic treatment–what your patient should know. Dental update. 2002 Dec 2;29(10):492-6.
-
AAO issues a special bulletin on extraoral appliance care, Editorial. Am J Orthodontics, 1975;68:457.
-
Samuels RH, Orth D, Orth M. A review of orthodontic face-bow injuriesand safety equipment. Am J Ortho Dentofacial Orthop. 1996 Sep 1;110(3):269-72.
-
Consolaro A, Romano FL. Reasons for mini-implants failure: choosing installation site should be valued!. Dental press journal of orthodontics. 2014 Apr;19(2):18-24.
-
Kravitz ND, Kusnoto B. Risks and complications of orthodontic miniscrews. Am J Orthodont Dentofacia lOrthopedics. 2007 Apr 1;131(4):S43-51.
-
Long H, Pyakurel U, Wang Y, Liao L, Zhou Y, Lai W. Interventions for accelerating orthodontic tooth movement: A systematic review. The Angle Orthodontist. 2013 Jan 1;83(1):164-71.
-
Mathews DP, Kokich VG. Accelerating tooth movement: the case against corticotomy-induced orthodontics. Ame J Orthod Dentofacial Orthoped. 2013 Jul 1;144(1):11.
-
Shenava S, Nayak KU, Bhaskar V, Nayak A. Accelerated orthodontics–a review. Int J Sci Study. 2014 Feb;1(5):35-9.
-
Puryer J, McNamara C, Sandy J, Ireland T. An ingested orthodontic wire fragment: a case report. Dentistry J. 2016 Sep;4(3):24.
-
British Orthodontic Society . Advice Sheet—Guidelines for the Management of Inhaled or Ingested Foreign Bodies. British Orthodontic Society; London, UK: 2011.
-
Cameron SM, Whitlock WL, Tabor MS. Foreign body aspiration in dentistry: a review. J Am Dent Assoc. 1996 Aug;127(8):1224-9.
-
Al-Wahadni A, Al Hamad KQ, Al-Tarawneh A. Foreign body ingestion and aspiration in dentistry: a review of the literature and reports of three cases. Dental update. 2006 Nov 2;33(9):561-70.
-
Wheeler TT. Orthodontic clear aligner treatment. InSeminars in Orthodontics 2017 Mar 1;23(1):83-89. WB Saunders.
-
Papageorgiou SN, Koletsi D, Iliadi A, Peltomaki T, Eliades T. Treatment outcome with orthodontic aligners and fixed appliances: a systematic review with meta-analyses. Eur J Orthod. 2020 Jun 23;42(3):331-43.
-
Zheng M, Liu R, Ni Z, Yu Z. Efficiency, effectiveness and treatment stability of clear aligners: A systematic review and meta?analysis. Orthod Craniof Res. 2017 Aug;20(3):127-33.
-
Allareddy V, Nalliah R, Lee MK, Rampa S, Allareddy V. Adverse clinical events reported during Invisalign treatment: Analysis of the MAUDE database. Am J Orthod Dentofacial Orthoped. 2017 Nov 1;152(5):706-10.
-
Bakula A, Lugovi?-Mihi? L, Situm M, Turcin J, Sinkovi? A. Contact allergy in the mouth: diversity of clinical presentations and diagnosis of common allergens relevant to dental practice. ActaClin Croat. 2011 Dec 14;50(4):553-61.
-
Kim H, Johnson JW. Corrosion of stainless steel, nickel-titanium, coated nickel-titanium, and titanium orthodontic wires. Angle Orthod. 1999 Feb;69(1):39-44
-
Rahilly, G. Current Products and Practice: Nickel allergy and orthodontics. J Orthod. 2003 June; 30(2):171-174
-
Patel A, Burden DJ, Sandler J. Medical disorders and orthodontics. J Orthod. 2009 Dec;36 Suppl:1-21
-
Neiburger EJ. A case of possible latex allergy. J Clin Orthodon : JCO. 1991 Sep;25(9):559-560.
-
Hain MA, Longman LP, Field EA, Harrison JE. Natural rubber latex allergy: implications for the orthodontist. J Orthod. 2007 Mar;34(1):6-11
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License