IJCRR - 13(17), September, 2021
Pages: 161-166
Date of Publication: 12-Sep-2021
Print Article
Download XML Download PDF
A Panorama of the Applications of Midazolam in Dentistry and Recent Advances
Author: Jason ASD, Manisha, Samuel VA
Category: Healthcare
Abstract:The prevalence of dental fear is ubiquitous and so is the need; to remove fear and anxiety. Depression of the individual's consciousness during the treatment aids tremendously in a positive patient outcome. It also contributes to a better overall oral health of the community. All the sedative agents of old have either caused more harm than good or failed in their effectiveness. With the introduction of midazolam in1975 sedation has not only become safe but also highly effective. Midazolam acts by enhancing the activity of the GABA receptors in the central nervous system. Alongside the sedative effect, the drug shows anxiolytic, muscle relaxant, anticonvulsant, hypnotic and amnesic properties. Literature supports the use of midazolam as an emergency drug for seizures, for conscious sedation and as a part of the pre-anaesthetic medication. Midazolam has been used extensively to achieve positive behaviour in children undergoing dental therapy. Certain side effects have been reported with the use of this drug. With modern delivery systems such as Mucosal Atomization Device (MAD), the rapidity of onset of the drug is enhanced along with a reduction of the dose. This review article stands as a testimony to the use of midazolam in dentistry.
Keywords: Dental Fear, Anxiety, Midazolam, Sedation Dentistry, Conscious Sedation, Mucosal Atomization Device
Full Text:
INTRODUCTION
Fear is an unpleasant feeling often caused due to the awareness of danger or hurt.1The most pragmatic way to define fear is as the neurophysiological processes that prepare an organism to perform innate or learned responses to cope with danger.2,3Dental fear has been a significant contributor to the evasion of dental health care.4,5,6
Anxiety precedes fear, wherein anxiety occurs before the presence of a stimulus that, more often than not, is threatening.7,8Anxiety alters reality which leads to patients experiencing a change in the quality of pain perceived by them and instils an everlasting pain-tinted dental experience.9 the dentist has to identify the aspects of the dental setting which would likely aggravate the anxiety, the need for the current appointment and the previous dental experiences of the patient.7,10,11The components of pharmacological anxiolysis include sedation and general anaesthesia.12Factors to be considered are the risks of the pharmacological management versus benefit, selection of the appropriate drug, the level of anxiety, dentist’s expertise, presence of equipment and emergency care.13
Sedation is defined as the use of a drug or combination of drugs to depress the central nervous system, thus reducing patients’ awareness of their surroundings.14Conscious sedation has been employed as a means to remove fear and anxiety from dental care and it is considered of paramount importance. Anxiolysis is a drug-induced state during which patients respond normally to verbal commands.15,16It is mandatory to note that the use of conscious sedation should be taken bearing the patient’s thorough medical and dental history. Barbiturates were a few of the earliest sedative agents used for conscious sedation. With the introduction of benzodiazepines (Midazolam), conscious sedation included anxiolysis along with profound amnesia. They are considered the gold standard in sedation and are regarded as very safe drugs.17
The dentist must alleviate the anxiety and fear as it can cause exhaustion post-treatment and a ripple in the normal facets of one’s daily activities including personal, social interactions and sleep deprivation.18,19Midazolam as a sedative has made a significant contribution towards conscious sedation. A plethora of studies backs midazolam in terms of efficiency, ease of administration and safety. This article provides a meticulously prepared agglomerate of the scientific literature with regards to the use of midazolam for conscious sedation in dental practice.
HISTORY
The need for the removal of fear and pain from the dental office has existed as long as the existence of the art of dentistry. In the 15th century ether was used as the first anaesthetic agent alongside, a distillate of sulphuric acid and diethyl ether called ‘sweet oil of vitriol’ which was widely used in dentistry.20The 17th century saw the discovery of nitrous oxide by Joseph Priestley. Humphrey Davy commented on the uses of nitrous oxide in surgeries and its potency in alleviating pain.21The first benzodiazepines were created by Hoffmann-La Roche and Leo Sternbach in 1955. Diazepam (Valium) was discovered a little later but grew very famous. Molecular changes were made to meet the demands and also counteract any undesirable quality.22Midazolam was created in 1975 by Walser and Fryer.23
CHEMICAL STRUCTURE
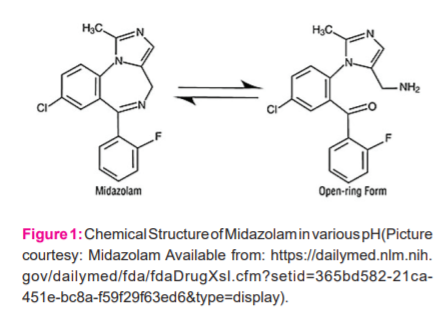
Midazolam is a water soluble, crystalline yellow to white salt.24The IUPAC name for midazolam hydrochloride is 8-chloro-6-(2-fluorophenyl)-1-methyl-4H-imidazo[1,5-a][1,4]benzodiazepine hydrochloride and the molecular formula is C18H13ClFN3 • HCl.25 In low pHthe salt is hydrophilic and has an open diazepine ring which closes shut at high pHto form the physiologically active lipophilic product as in Figure 1.It has a molecular weight of 325.8 g/mol.24
MECHANISM OF ACTION
Midazolam is a short-acting benzodiazepine with pharmacological uses such as anxiolytic, amnestic, muscle relaxant and sedative uses.26The mechanism of action of midazolam as a sedative is based on its effect on the GABA (gamma-aminobutyric acid) receptors. It works by enhancing the affinity of the GABA to the GABA receptor.21GABA is a major inhibitory neurotransmitter present in the central nervous system.27Benzodiazepines do not have a direct agonistic activity on GABA rather it has a boosting effect on the action of GABA.26The GABA receptors are classified into GABAa and GABA receptors. GABAa receptors have subtypes α1 and α2. Of these α1 subtype mediates sedation, anti-convulsant and amnesia activity while the α2 subtype mediates anxiolysis and muscle relaxation. They do not act on GABA receptors.
Midazolam has both hydrophilic and lipophilic properties depending on the pH of the solution. When midazolam is absorbed it has to bio transform through both the microsomal oxidation and glucuronide conjugation. First, it gets hydroxylated with the help of cytochrome CYP3A4, CYP3A5.28Through the hydroxylation process two pharmacologically active agents namely, α-hydroxymidazolam and 4-hydroxymidazolam are formed. They undergo rapid glucuronide conjugations to form pharmacologically inactive compounds.29Midazolam gets bounded to the plasma protein and is well distributed.30
PHARMACOKINETICS
Absorption
Midazolam is available in its salt form which is hydrophilic and maintains its hydrophilicity at a low pH. The oral midazolam tablet often stays hydrophilic due to the low pH in the stomach. With the change in pH in the gastrointestinal tract to the physiological pH, the ring structure of midazolam closes forming the lipophilic form.31Midazolam is absorbed through the gastrointestinal tract following oral administration, with peak effect 30-90 minutes after administration. Owing to the first pass metabolism only 40-50% of the administered dose reaches circulation.32Midazolam has shown rapid onset and increased bioavailability of 90% through the intramuscular route.33The intranasal route of administration has shown superiority in the onset duration and ease of use when compared with the oral route.34It is important to consider the painless quality of the intranasal route compared to the intramuscular and the intravenous routes.35
Distribution
Midazolam distribution is higher among obese people as it gets distributed to the adipose tissue. The volume of distribution has been found to be 1-2.5 l/kg.36The distribution is greater in women compared to men.37Midazolam has a good affinity to plasma proteins and is mostly bound to them only about 4% of the given dosage is available as free faction.38
Elimination
Metabolites of midazolam in the form of α-hydroxymidazolam and glucuronide conjugate are excreted by the kidney through urine. Almost all of the midazolam gets conjugated, less than 0.5% gets excreted unchanged. The plasma clearance seemed to increase in patients in supine position owing to the 40-60% increase in the hepatic blood flow.24
PHARMACODYNAMICS
The action of midazolam in the body is chiefly based on its highly sedative potency. Besides its sedative nature, it has antiepileptic properties, acts as a muscle relaxant and causes anterograde amnesia. Once the effect wears off, the patient’s cognitive and psychomotor skills are retained.37Minimal cardiovascular changes are evoked by this drug. Midazolam could decrease vascular resistance.39Midazolam causes an increase in the frequency of respiratory rate with a decrease in tidal volume.40It leaves the cortisol and renin responses unaltered during surgical stress. It preserves the blood flow to the brain and myocardium while reducing flow to the liver and kidneys.41
SIDE EFFECTS
Midazolam like any other drug is a slave to the side effects it manifests. The side effects are cardiac arrest, heart rate variations, a fall in blood pressure, convulsions, anaphylaxis, thrombosis, laryngospasm, bronchospasm, respiratory depression, gastrointestinal changes, xerostomia, hiccups, increased appetite, jaundice, drowsiness, confusion, dysarthria, urinary retention or incontinence, blood disorders, muscle weakness, visual disturbances including diplopia, salivation changes, skin reactions along with any skin changes in the intravenous route injection site. When given through the intranasal route, midazolam is known to produce a burning sensation, irritation to the nasal mucosa and lacrimation.24,25,42 When taken orally there is a delay in onset and there is no IV access for a reversal agent in case of overdose.43
DRUG INTERACTION
Drug interactions between midazolam and other drugs are chiefly governed by the cytochrome P450 oxidase system in the liver where midazolam gets metabolized. Drugs such as cimetidine, ranitidine, omeprazole, macrolides and oral contraceptives inhibit the metabolism of midazolam causing reduced clearance and increased half-life.36,44,45 Rifampin is a cytochrome P450 enzyme inducer that increases the clearance of midazolam.46
DISCUSSION
Midazolam has shown anxiolytic, sedative, muscle relaxant, anticonvulsant, hypnotic and amnesic properties which can be exploited in the dental setting.26,47, 48, 49
Midazolam as an emergency drug in the dental office
Seizures are commonly encountered in the dental office with a worldwide prevalence of 0.5-0.9% The management of epilepsy is achieved through the depression of the central nervous system which could be achieved with benzodiazepines.50Midazolam has been included in the additional emergency drugs for the management of dental emergencies.51,52The muscle relaxant property of midazolam has been exploited in the rapid sequence intubation for establishing a patent airway in the emergency department in dosage of 0.1mg/kg.53,54Besides these the property of amnesia, anxiolysis and sedation play their role in making midazolam a must-possess emergency drug.27,55
Midazolam as a pre-anaesthetic agent in the pediatric population
Children in the initial stage of anaesthesia could experience unpleasantness, have anxiety and suffer from separation from parents leading to hypersalivation, breath-holding and laryngospasm.56Besides these, there could be traumatic experiences deeply rooted in the child’s mind from the induction room.57, 58
Midazolam is chosen as a pre-anaesthetic medication as it is predictable and has good patient acceptance. It is consistent and has few side effects which are the ideal characteristics of a premedicament.59Various drug dosages have been tried by various authors when using midazolam as a pre-anaesthetic agent.60 The most effective dosage and safest dose for children has been identified as 0.75mg/kg considering the age and weight of the child.61
Midazolam in conscious sedation
Conscious sedation in dentistry plays a major role in achieving a positive psychological effect on the patient while also preserving the consciousness and the responsiveness to verbal commands.7Midazolam is one of the most commonly used benzodiazepine drugs.62 In conscious sedation, the consciousness of the patient remains uncompromised as compared to general anaesthesia and deep sedation; hence it provides a wide margin of safety.15
A few reported disadvantages of nitrous oxide inhalation include expensive equipment, patients should breathe through their nose and interference of nasal mask with maxillary injection techniques.63 Chronic exposure to nitrous oxide showed devastating effects on the health of the dental personnel. It could decrease the fertility of female doctors and assistants and cause a 1.7 fold increase in liver disease among men. Midazolam for conscious sedation is available in various routes such as oral, intravenous and intranasal.64 Oral midazolam is the go-to technique among the pediatric population. A 0.5 mg/kg dosage is given 20 minutes before the procedure which causes significant anxiolysis and results in a more positive environment.65 Besides, midazolam causes anterograde amnesia changing the postoperative perspective of the patient towards dental treatment.66
Studies indicate intravenous midazolam given at 0.06mg/kg dosage produced adequate anxiolysis. The onset was significantly faster. 5 minutes post-administration the effects of sedation started to manifest. The children administered IV midazolam showed lesser movement in-between treatments, cried less and mostly fell asleep during the entire procedure.67 The intranasal route has the benefits such as a large surface area of the nasal mucosa and the drug escapes the first-pass metabolism. Though various anatomic, physiologic and drug characteristics play a major role in the absorption one of the most important criteria is that the drug needs to be lipophilic for absorption to occur through the mucosa.68 Literature claims the intranasal route to be effective in terms of ease of use and reduced duration of onset with a dosage of 0.3-0.5mg/kg.69-73
The intranasal use of midazolam has been enhanced with the introduction of MAD® (Mucosal Atomization Device, Wolfe Tory Medical Inc., Salt Lake City, UT, USA) Figure 2. The MAD® atomizes the drug into particles of 30-100 microns. Particles this small are readily absorbed through the nasal mucosa. The soft plug gives a neat seal, reducing the run-off. The procedure is painless and less cumbersome compared to the other injection techniques.74The use of this spray has proven to be more efficient in terms of acceptability and the induction of sedation compared to intranasal drops and the oral route.75,76 The use of such a device is explicit in the emergency setting and to attain anxiolysis before diagnostic scans chiefly due to the ease of administration and quick onset.74,77
CONCLUSION
Of the many challenges that confront the dentist, the obliteration of fear from the dental setting proves fit to test the mettle of the dentist. Midazolam has made sedation easy for patients and dentists alike. Midazolam is very safe for use in the pediatric population, where the need to remove fear is even more important to develop a positive attitude in children, which would drastically improve their overall oral health. With the introduction of newer technologies, the figments of painless, fearless dentistry have come closer to reality.
ACKNOWLEDGEMENT
The authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors/editors/publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
SOURCE OF FUNDING
Not applicable as there is no source of funding
CONFLICT OF INTEREST
The authors declare no conflict of interest.
AUTHOR’S CONTRIBUTION
Samuel VA conceptualized the work. Data collection was carried out by Jason ASDand Manisha. The article was drafted by Jason ASD with support from Manisha and Samuel VA. Critical revision of the article was done by Manisha and Samuel VA. The final approval of the version of the article to be published was done by Samuel VA.
References:
-
Webster's third new international dictionary of the English language. 10th ed. Springfield (Massachusetts): Merriam-Webster; 2002 Fear; p. 924
-
Keifer OP Jr, Hurt RC, Ressler KJ, Marvar PJ. The Physiology of Fear: Reconceptualizing the Role of the Central Amygdala in Fear Learning. Physiology (Bethesda). 2015;30(5):389-401.
-
Adolphs R. The Biology of Fear. Curr Biol. 2013;23(2): R79-93.
-
Pohjola V, Lahti S, Vehkalahti MM, Tolvanen M, Hausen H. Association between dental fear and dental attendance among adults in Finland. Acta Odontologica Scandinavica. 2007;65(4):224-30.
-
Ramakrishnan M, Banu S, Ningthoujam S, Samuel VA. Evaluation of knowledge and attitude of parents about the importance of maintaining primary dentition - A cross-sectional study. J Family Med Prim Care. 2019 Feb;8(2):414-8.
-
Ravikumar D, Gurunathan D, Karthikeyan S, Subramanian E, Samuel VA. Age and Environment Determined Children's Preference Towards Dentist Attire - A Cross-Sectional Study. J Clin Diagn Res. 2016 Oct;10(10): ZC16-9.
-
Appukuttan D. Strategies to manage patients with dental anxiety and dental phobia: a literature review. Clin CosmetInvestig Dent. 2016;8:35-50
-
Diagnostic and Statistical Manual of Mental Disorders. DSM-III. American Psychiatric Association: Washington, D.C.1980. Psychol Med 1981;11(1):215.
-
Weisenberg M, Aviram O, Wolf Y, Raphaeli N. Relevant and irrelevant anxiety in the reaction to pain. Pain. 1984;20(4):371-83.
-
Jöhren P, Jackowski J, Gängler P, Sartory G, Thom A. Fear reduction in patients with dental treatment phobia. Br J OralMaxillofac Surg. 2000;38(6):612-6.
-
Sharna N, Ramakrishnan M, Samuel V, Ravikumar D, Cheenglembi K, Anil S. Association between Early Childhood Caries and Quality of Life: Early Childhood Oral Health Impact Scale and Pufa Index. Dent J. 2019;7(4):95.
-
Folayan M, Faponle A, Lamikanra A. A review of the pharmacological approach to the management of dental anxiety in children. Int J Paediatr Dent. 2002;12(5):347-54.
-
Newton T, Asimakopoulou K, Daly B, Scambler S, Scott S. The management of dental anxiety: time for a sense of proportion?. BrDentJ 2012;213(6):271-4.
-
Morita T., Tsuneto, S., Shima Y. Definition of sedation for symptom relief: a systematic literature review and a proposal of operational criteria. J Pain Symptom Manag. 2002:24(4), 447-53.
-
An Updated Report by the American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists. Practice Guidelines for Sedation and Analgesia by Non-Anesthesiologists. Anesthes. 2002 Apr 1;96(4):1004–17.
-
Holroyd I. Conscious sedation in pediatric dentistry. A short review of the current UK guidelines and the technique of inhalational sedation with nitrous oxide.Paediatr Anesth. 2008 Jan;18(1):13-7.
-
Lauven PM. Pharmacology of Drugs for Conscious Sedation. Scand J Gastroenterol. 1990 Jan 1;25(sup179):1–6.
-
Cohen S, Fiske J, Newton J. The impact of dental anxiety on daily living. Br Dent J. 2000;189(7):385-90.
-
Moore R, Brodsgaard I. Dentists' perceived stress and its relation to perceptions about anxious patients. Community Dent Oral Epidemiol. 2001;29(1):73-80.
-
Robinson DH, Toledo AH. Historical development of modern anaesthesia. J Invest Surg. 2012 Jun;25(3):141-9.
-
Haridas RP. Horace Wells’ Demonstration of Nitrous Oxide in Boston: Anesthesiology. 2013 Nov;119(5):1014–22.
-
Wick JY. The History of Benzodiazepines. Consult Pharm. 2013 Sep 1;28(9):538–48.
-
Walser A, Flynn T, Fryer RI. Quinazolines and 1,4-benzodiazepines. LXXXV syntheses of 3-substituted lmidazo[1,5-a] [1,4]benzodiazepines. J HeterocyclChem. 1978;15(4):577–83.
-
PubChem [Internet]. Bethesda (MD): National Library of Medicine (US), National Center for Biotechnology Information; 2004-. PubChem Compound Summary for CID 4192, Midazolam; [cited 2021 Apr. 8].
-
Sabarathinam S, Vijayakumar TM. RP-hplc method development and validation of midazolam: A cyp3a4 probe drug. ResJPharmTechnol. 2020;13(8):3565-8
-
Richter JJ. Current Theories about the Mechanisms of Benzodiazepines and Neuroleptic Drugs: Anesthesiology. 1981 Jan;54(1):66–72.
-
Braestrup C, Squires RF. Brain-specific benzodiazepine receptors. Br J Psychiatry. 1978 Sep;133:249–60.
-
Wandel C, Böcker R, Böhrer H, Browne A, Rügheimer E, Martin E. Midazolam is metabolized by at least three different cytochrome P450 enzymes. Br J Anaesth. 1994 Nov;73(5):658–61.
-
Heizmann P, Eckert M, Ziegler WH. Pharmacokinetics and bioavailability of midazolam in man.Br J Clin Pharmacol. 1983;16 Suppl 1:43S-9S.
-
Olkkola KT, Ahonen J. Midazolam and Other Benzodiazepines. Modern Anesthetics. Berlin, Heidelberg: Springer Berlin Heidelberg.HandbExpPharmacol. vol. 182.; 2008. p. 335–60.
-
Burstein AH, Modica R, Hatton M, Forrest A, Gengo FM. Pharmacokinetics and Pharmacodynamics of Midazolam After Intranasal Administration. J Clin Pharmacol. 1997 Aug;37(8):711–8.
-
Kanto JH. Midazolam: the first water-soluble benzodiazepine. Pharmacology, pharmacokinetics and efficacy in insomnia and anaesthesia. Pharmacotherapy. 1985 Jun;5(3):138–55.
-
Taylor JW, Simon KB. Possible intramuscular midazolam-associated cardiorespiratory arrest and death.Drug Intell Clin Pharm. 1990 Aug;24(7–8):695–7.
-
Musani I, Chandan N. A comparison of the sedative effect of oral versus nasal midazolam combined with nitrous oxide in uncooperative children. EurArch Paediatr Dent. 2015;16(5):417-24.
-
Li A, Yuen VM, Goulay-Dufaÿ S, Sheng Y, Standing JF, Kwok PCL, et al. Pharmacokinetic and pharmacodynamic study of intranasal and intravenous dexmedetomidine. BrJ Anaesth. 2018;120(5):960-8.
-
Nordt SP, Clark RF. Midazolam: A review of therapeutic uses and toxicity. J Emerg Med. 1997 May 1;15(3):357–65.
-
Dundee JW, Halliday NJ, Harper KW, Brogden RN. Midazolam. Drugs. 1984 Dec 1;28(6):519–43.
-
Reves JG, Fragen RJ, Vinik HR, Greenblatt DJ. Midazolam: pharmacology and uses. Anesthesiology. 1985 Mar;62(3):310–24.
-
Boralessa H, Senior DF, Whitwam JG. Cardiovascular response to intubation. A comparative study of thiopentone and midazolam. Anaesthesia. 1983 Jul;38(7):623–7
-
Power SJ, Morgan M, Chakrabarti MK.Carbon dioxide response curves following midazolam and diazepam.Br J Anaesth.1983 Sep;55(9):837–41
-
Daneshmend TK, Jackson L, Roberts CJ. Physiological and pharmacological variability in estimated hepatic blood flow in man. Br J Clin Pharmacol. 1981;11(5):491–6.
-
Kowalczuk J. British National Formulary for Children 2005. Qual Saf Health Care. 2006 Feb;15(1):76.
-
Papineni McIntosh A, Ashley PF, Lourenço-Matharu L. Reported side effects of intravenous midazolam sedation when used in paediatric dentistry: a review. Int J Paediatr Dent. 2015 May;25(3):153–64.
-
Olkkola KT, Aranko K, Luurila H, Hiller A, Saarnivaara L, Himberg JJ, et al. A potentially hazardous interaction between erythromycin and midazolam. Clin Pharmacol Ther. 1993;53(3):298–305.
-
Abernethy DR, Greenblatt DJ, Divoll M, Arendt R, Ochs HR, Shader RI. Impairment of diazepam metabolism by low-dose estrogen-containing oral-contraceptive steroids. N Engl J Med. 1982 Apr 1;306(13):791–2.
-
Ohnhaus EE, Brockmeyer N, Dylewicz P, Habicht H. The effect of antipyrine and rifampin on the metabolism of diazepam.Pharmacol Ther. N Engl J Med .1987:42: 148-56.
-
Kupietzky A, Houpt MI. Midazolam: a review of its use for conscious sedation of children. Pediatr Dent. 1993 Aug;15(4):237–41
-
Bergman SA. The Benzodiazepine Receptor.Anesth Prog.1986;33(5):213–9.
-
Greenblatt DJ, Shader RI, Abernethy DR. Drug therapy. Current status of benzodiazepinesN Engl J Med. 1983 Aug 18;309(7):410–6.
-
Turner MD, Glickman RS. Epilepsy in the Oral and Maxillofacial Patient: Current Therapy. J Oral Maxillofac Surg. 2005 Jul;63(7):996–1005.
-
Haas DA. Emergency drugs. Dent Clin North Am. 2002 Oct;46(4):815-30.
-
Haas DA. Management of Medical Emergencies in the Dental Office: Conditions in Each Country, the Extent of Treatment by the Dentist.Anesth Prog. 2006;53(1):20–4.
-
Wroblewski BA, Joseph AB. Intramuscular midazolam for treatment of acute seizures or behavioural episodes in patients with brain injuries.JNeurol Neurosurg Psychiatry. 1992 Apr;55(4):328–9.
-
Sagarin MJ, Barton ED, Sakles JC, Vissers RJ, Chiang V, Walls RM; National Emergency Airway Registry Investigators. Underdosing of midazolam in emergency endotracheal intubation. Acad Emerg Med. 2003 Apr;10(4):329-38.
-
Malinovsky JM, Populaire C, Cozian A, Lepage JY, Lejus C, Pinaud M. Premedication with midazolam in children. Effect of intranasal, rectal and oral routes on plasma midazolam concentrations. Anaesthesia. 1995;50(4):351–4.
-
De Soto H. The Pediatric Anesthesia Handbook. Anesthesiology. 1997 Nov 1;87(5):1266.
-
Mathai A, Nazareth M, Raju RS. Preanesthetic sedation of preschool children: Comparison of intranasal midazolam versus oral promethazine.Anesth EssaysRes. 2011;5(1):67–71.
-
Kain ZN, Hofstadter MB, Mayes LC, Krivutza DM, Alexander G, Wang SM, et al. Midazolam: Effects on Amnesia and Anxiety in Children. Anesthesiology. 2000 Sep;93(3):676–84.
-
Coté CJ, Cohen IT, Suresh S, Rabb M, Rose JB, Weldon BC, et al. A comparison of three doses of a commercially prepared oral midazolam syrup in children.Anesth Analg. 2002 Jan;94(1):37–43.
-
Kaviani N, Shahtusi M, Haj Norousali Tehrani M, Nazari S.. Effect of Oral Midazolam Premedication on Children’s Co-operation Before General Anesthesia in Pediatric Dentistry.JDent(Shiraz). 2014 Sep;15(3):123–8.
-
McMillan CO, Spahr-Schopfer IA, Sikich N, Hartley E, Lerman J. Premedication of children with oral midazolam. Can J Anesth. 1992 Jul;39(6):545–50.
-
Finder RL, Moore PA. Benzodiazepines for intravenous conscious sedation: agonists and antagonists. Compendium. 1993 Aug;14(8): 976-80.
-
Mohan R, Asir VD, Shanmugapriyan, Ebenezer V, Dakir A, Balakrishnan, et al. Nitrous oxide as a conscious sedative in the minor oral surgical procedure. J Pharm Bioallied Sci. 2015 Apr;7(Suppl 1): S248–50.
-
Howard WR. Nitrous oxide in the dental environment: assessing the risk, reducing the exposure. J Am Dent Assoc. 1997 Mar;128(3):356–60.
-
Wan K, Jing Q, Zhao JZ. Evaluation of oral midazolam as conscious sedation for pediatric patients in oral restoration. ChinMed Sci J. 2006 Sep;21(3):163–6.
-
Twersky RS, Hartung J, Berger BJ, McClain J, Beaton C. Midazolam enhances anterograde but not retrograde amnesia in pediatric patients. Anesthesiology. 1993 Jan;78(1):51–5.
-
Tyagi P, Tyagi S, Jain A. Sedative effects of Oral Midazolam, Intravenous Midazolam and Oral Diazepam in the Dental Treatment of Children. J Clin Pediatr Dent. 2013 Apr;37(3):301–6.
-
Grassin-Delyle S, Buenestado A, Naline E, Fairy C, Blouquit-Laye S, Couderc LJ, et al. Intranasal drug delivery: An efficient and non-invasive route for systemic administration: focus on opioids. Pharma col Ther.2012 Jun;134(3):366–79.
-
Peerbhay F, Elsheikhomer A. Intranasal Midazolam Sedation in a Pediatric Emergency Dental Clinic. Anesth Prog 2016;63(3):122-30.
-
Lee-Kim SJ, Fadavi S, Punwani I, Koerber A. Nasal versus oral midazolam sedation for pediatric dental patients. J Dent Child (Chic). 2004 May-Aug;71(2):126-30.
-
Özen B, Malamed SF, Cetiner S, Özalp N, Özer L, Altun C. Outcomes of moderate sedation in paediatric dental patients. AustDentJ. 2012;57(2):144-50.
-
Malinovsky JM, Lejus C, Servin F, Lepage JY, Le Normand Y, Testa S, et al. Plasma Concentrations Of Midazolam After I.V., Nasal Or Rectal Administration In Children. Br J Anaesth. 1993;70(6):617-20.
-
Kogan A, Katz J, Efrat R, Eidelman LA. Premedication with midazolam in young children: a comparison of four routes of administration. Pediatr Anesth. 2002;12(8):685-9.
-
Corrigan M, Wilson SS, Hampton J. Safety and efficacy of intranasally administered medications in the emergency department and prehospital settings.Am JHealth-SystPharm. 2015 Sep 15;72(18):1544–54.
-
Primosch RE, Guelmann M. Comparison of drops versus spray administration of intranasal midazolam in 2 and 3-year-old children for dental sedation.Pediatr Dent J. 2005 Oct;27(5):401–8.
-
Fallahinejad Ghajari M, Ansari G, Soleymani AA, Shayeghi S, Fotuhi Ardakani F.Comparison of Oral and Intranasal Midazolam/Ketamine Sedation in 3?6-year-old Uncooperative Dental Patients. J Dent Res Dent Clin Dent Prospects. 2015;9(2):61-5.
-
Hollenhorst J, Münte S, Friedrich L, Heine J, Leuwer M, Becker H, et al. Using Intranasal Midazolam Spray to Prevent Claustrophobia Induced by MR Imaging. Am J Roentgenol. 2001;176(4):865-8.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License