IJCRR - 13(17), September, 2021
Pages: 105-115
Date of Publication: 12-Sep-2021
Print Article
Download XML Download PDF
Bone Graft Materials in Late Secondary and Tertiary Alveolar Bone Grafting: A Review
Author: Mallick Rizwana, Pisulkar Sweta Kale, Reddy Srinivas Reddy, Jain Vanshika
Category: Healthcare
Abstract:Introduction: Bone grafting of the alveolar cleft is necessary to facilitate unhindered growth of maxillofacial complex and eruption of permanent teeth in defect region when not congenitally missing. Secondary grafting undertaken during mixed dentition helps achieve these two functions. However, due to varying reasons, socioeconomic concerns being one of them, many patients do not undergo this procedure and report at a time when late grafting is the only option to overcome the deficit bone. Aims: To identify the different grafting materials that have been utilized for the 2 surgical procedures. Methodology: Electronic databases were searched to find bone sources used for secondary and tertiary bone grafting to identify their characteristics and clinical outcomes. Attention was paid to literature which elucidated potential use of dental implants in the grafted site and presented its clinical course. Results: Over the years, many graft materials have been researched upon with autologous sources being considered as the gold standard and being the most commonly utilized. Additionally, graft characteristics, observations of the published authors, and success of implant rehabilitation, where used showed a mixed bag of results. Certain other potential bone sources were also identified that have shown in-vitro or animal model success but have not yet made a clinical presence for the reviewed procedures. Conclusion: Choice of bone graft depends on numerous factors such as defect size, surgeon preference and patient acceptance. To understand further each graft source and its characteristics, randomized control trials should be conducted to provide better clinical evidence.
Keywords: Alveolar bone grafting, Alveolar cleft, Congenital abnormalities, Dental implants, Rehabilitation, Tertiary grafting
Full Text:
INTRODUCTION
The multidisciplinary team involved in the treatment and repair of the orofacial cleft has faced challenges of successfully and satisfactorily repairing and rehabilitating the affected region. Advances in surgical knowledge, techniques, and materials, have kept the quest open, to find a universally accepted ideal bone grafting material. Secondary alveolar bone grafting (SABG) is done during the mixed dentition to facilitate permanent teeth eruption and minimizes functional and esthetic compromise. In cases where the permanent tooth in the cleft region fails to form or is indicated for extraction, it inadvertently requires prosthetic replacement which cannot be done till the patient attains skeletal maturity.
Removable and fixed partial dentures (RPD and FPD) are the oldest rehabilitative substitutes that, though easy to fabricate, provide limited esthetics. They also do not contribute to functional graft stimulation, thereby leading to increased resorption.1 With overtime use, RPDs require frequent replacement and irritate the underlying mucosa. Contrarily, FPDs compromise the adjacent healthy hard and soft tissue. Thus, both modalities add to patient’s physical stress of frequent and multiple visits, often denting them psychologically. Dental implants are a welcome alternative however, by the time a patient completes facial growth, the previously grafted bone inadvertently undergoes resorption, providing poor dimensions for implant support, thus failing the test of time. In such cases, tertiary bone grafting is undertaken to restore the dimensions and proceed with the treatment. In many cases, patients are not subjected to SABG and report after the eruption of all permanent teeth. These patients also require an initial repair of the bone defect before proceeding with dental implant-based rehabilitation, if permitted by other factors.
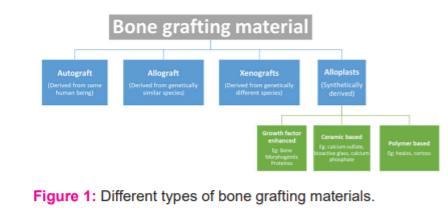
This current review is written to identify bone graft materials used for either late secondary or tertiary alveolar bone grafting in cleft patients (figure 1). It also discusses the qualitative and quantitative success of these materials as identified by the respective authors and the possibility of placing dental implants, wherever adequately provided.
To avoid ambiguity, the review considers certain terminologies as:
-
Primary alveolar bone grafting: any procedure performed to repair lip and/ or alveolar cleft at less than two years of age.
-
SABG: a surgical procedure performed during the mixed dentition phase before the eruption of the permanent maxillary canine.
-
Late secondary alveolar bone grafting: a surgical procedure performed after the eruption of permanent maxillary canine, without prior history of grafting procedure except primary alveolar grafting.
-
Tertiary grafting: alveolar cleft repair in a patient more than 18 years of age and with a positive history of SABG or late SABG.
AUTOLOGOUS GRAFTS
The use of autologous grafts is the most widely accepted as it is autologous origin avoids graft rejection. Various anatomical sites have been explored that provide adequate quantity without causing substantial donor site morbidity, is well accepted at the recipient site and maintains form over time.
Iliac bone graft
Autogenous bone graft from the iliac crest is one of the oldest sources, use of which is not limited to repair of maxillofacial defects. The many associated advantages and anatomy make iliac bone a “gold standard” grafting material. Mesenchymal in origin, it provides a rich quantity of cancellous bone which can be harvested with minimal complications.1 Three varieties of graft can be obtained from the iliac crest namely; cortical graft found in the outer bone layer comprising of compact bone, most widely used cancellous bone, the porous inner layer made of trabecular bone and corticocancellous bone which is a combination of the two. Vascularized grafts can also be obtained which provides predictable results.2 Anterior or posterior approach is used for bone harvesting with the latter showing superior results although it negates the advantage of simultaneous operation at two sites and has a slightly higher donor site morbidity.3,4
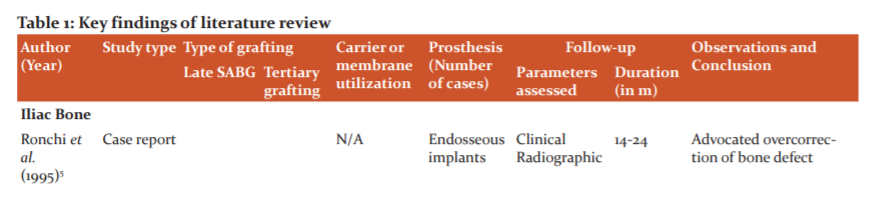
In probably the first of its kind published report, Ronchi et al,5did a late secondary procedure in three patients followed by endosseous implants placed after 8-12 months. The cancellous iliac graft was used in two patients while corticocancellous crest bone was harvested in the third patient. Overcorrection of bone defects was advocated to avoid repeat procedures during implant surgery.
Brauner et al.6 conducted tertiary grafting using heterologous cancellous bone with collagen membrane to restore bone dimensions in the affected site followed by dental implants after six months. Although no qualitative or quantitative assessments were provided for the regenerated bone, they concluded that tertiary grafting provided predictable and satisfactory esthetic results.
Performing SABG and late alveolar grafting, Takahashi et al.7 utilized autogenous cancellous iliac bone followed by endosseous implant placement after at least 1.4 years. Before implant surgery, the amount and density of trabecular bone were assessed and onlay graft using chin during implant surgery was conducted in some patients. At follow-up, in two of the concerned patients, the chin graft was partially lost because of wound dehiscence. Two implants were lost which was attributed to the short length and class 4 bone type formed by the graft. In a similar long-term follow-up study, due to insufficient vertical bone height after SABG, tertiary bone grafting was performed using only mandibular symphysis graft with simultaneous implant placement.8 Assessment of interdental alveolar bone height (IABH) was done for up to six years. From among the patient of interest for our review, only one case showed IABH reduction from score 3 to score 2 with no changes observed in other cases.
Hartel et al.9 retrospectively analyzed the data of cleft patients who were rehabilitated using implants. All patients received cancellous iliac chips as tertiary graft followed by additional augmentation using iliac or chin bone chips before implant placement due to partial or complete bone resorption. Need for the second graft varied from 7-60 months in most patients with re-graft being done as early as 5-7 weeks following tertiary grafting in three patients. Clinical and radiological follow-up presented one-fourth to two-third of resorption of the grafted bone around the implant in 70% of cases which were attributed to scars of previous surgical repairs.
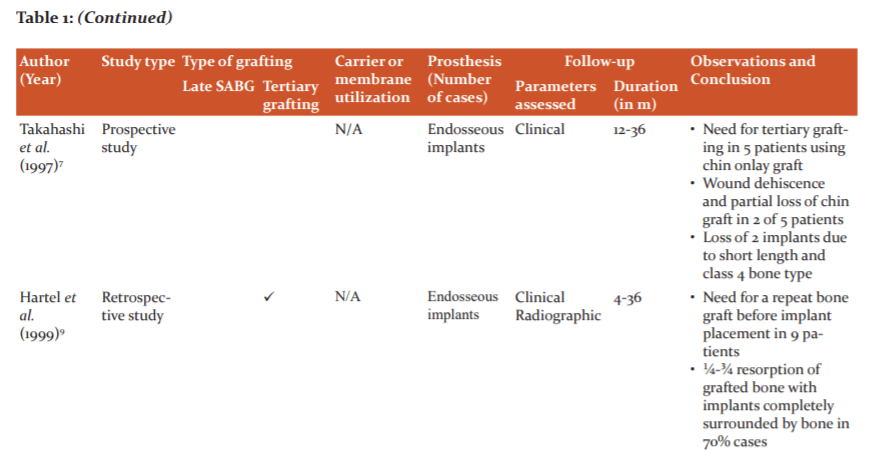
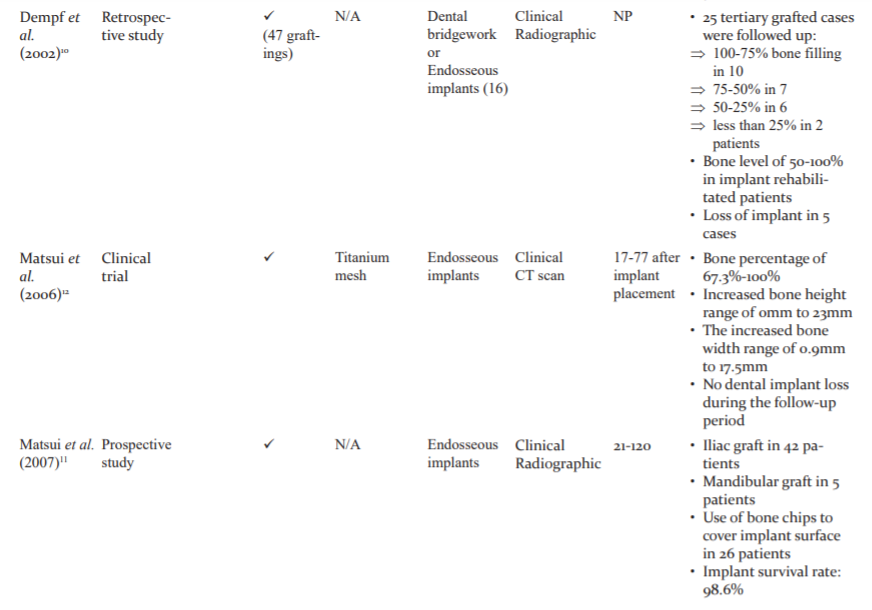
Comparing SABG with tertiary grafting, Dempf et al.10 used cancellous iliac chips for overcorrection of defect to compensate for post-operative physiological resorption. 47 tertiary grafting were done with an aim of prosthodontic rehabilitation. During follow-up, compared to a single patient (1.7%) in the SABG group, two tertiary grafted cases (8%) exhibited bone levels between 0-25%. Excellent bone stock (75-100%) was found in 10 patients (40%) in the latter group compared to 25 patients (41.7%) in the former. Complete graft resorption was not seen in any case, though lower resorption was reported for secondarily grafted cases.
Matsui et al.11 performed late secondary and tertiary grafting using versatile materials for implant-based rehabilitation in 47 patients. In 26 patients, 39 implants required the use of additional bone chips for coverage which were taken from the adjacent area. Appropriate distribution of these patients according to the previously performed bone grafting could not be determined. No statistically significant level of marginal bone loss (MBL) was seen between implants requiring bone chips and their counterparts. Acceptable results by the same author have been shown in another published work.12
From an orthodontic perspective, the use of iliac graft in late secondary grafting followed by maxillary expansion showed higher bone density than cases treated first with maxillary expansion followed by late grafting.13 At 12 months postoperatively, no significant difference in mean graft volume and bone density were observed between the two protocols.
Many other conducted studies have successfully used iliac crest graft, showing a mixed bag of results.14–18
Tibial graft
Proximal and distal tibia provide good quality, sufficiently stiff 25-70cm3 corticocancellous bone, without causing significant morbidity.2 Compared to iliac graft, tibial graft shows decreased inter-operative bleeding and surgical time (approximately 15 minutes), post-operative pain, scarring and hospitalization time with faster ambulation.19,20
Kaalaji et al.21 presented the retrospective success of tibial graft in repairing the alveolar cleft defect. Of the 39 patients, five underwent late secondary grafting followed by dental implant placement while the remaining patients were subjected to SABG. Patient follow-up reported the absence of complications; however, individual data for late grafting cases could not be elucidated.
Hussain20 performed alveolar bone grafting in nine patients of which six underwent tertiary grafting. The mean efficacy of material in terms of pre-and post-operative volume or area of the defect was calculated in tertiary grafted cases(71.72 ± 4.86) which were comparable to secondary grafting values (79.53 ± 9.07). They concluded tibial graft to be at par with usual grafting materials (iliac and rib graft) for cleft repair. Other authors have also reported successful use of tibial graft.22
Mandibular bone block
Mandibular symphysis and the retromolar area being embryonically like maxillary bone (ectomesenchymal origin), provides up to 3cm membranous bone (sufficient for small defects) with faster revascularization potential and lower resorption rate.1 Also, the procedure can be done under local anesthesia, in the same operative field as for cleft repair, thereby reducing post-operative discomfort.23
One of the oldest comparisons between autologous iliac and mandibular bone graft was made by Koole et al.1 who concluded that grafted mandibular bone showed a maximum of 37% resorption (52% patients) which was lesser than 50-100% resorption seen with iliac graft (44% patients).
Dolanmaz et al.23 did alveolar defect reconstruction using autologous mandibular block wherein procedures performed were either late secondary or tertiary grafting. In follow-up did two weeks following surgery, graft exposure was encountered only in three patients. 36 endosseous implants were placed, none of which showed clinical signs of failure except in one case where implant insertion led to graft mobilization. The accurate number of implants in cleft defect could not be assessed.
Sawaki et al.24 undertook bone height augmentation using ramus onlay graft in the bilateral cleft case due to insufficient available bone post SABG. The implant was placed in the grafted bone after five months which showed no clinical or radiographic signs of failure.
Calvarial bone
In probably the first of its kind study, Sadove et al evaluated the bone-forming potential of calvarial bone harvested to that of iliac bone for SABG.25 Comparable results were seen with the two graft types, however, craniotome use for obtaining calvarial graft was discouraged. Though technique sensitive, calvarial graft presents lower complications and resorption rate (9% to 19%) compared to approximately 50% resorption rate seen with iliac graft.26,27
Smolka et al.27 used calvarial bone for tertiary repair followed by implant-based rehabilitation after 4-6 months of grafting. In all cases, successful graft uptake and implant survival were reported, thereby supporting the use of calvarial bone.
Autogenous tooth bone (AutoBT)
Showing promising results, the use of permanent teeth (most commonly impacted third molars) as bone graft material is a recent advancement attributed to the osteoconductive nature of organic tooth structure.28 Based on the degree of demineralization, three types of dentin are evident namely; demineralized dentin, partially demineralized dentin matrix (70% decalcified), and demineralized dentin matrix, all of which show different results.28
Operating on the 19-year boy, Jeong et al.29 did the cleft repair using AutoBT obtained from the extracted mandibular third molar. The patient had a history of cleft lip and palate repair at 5-months and 6-years of age with the absence of further surgical details. Thus, the performed repair was either late secondary or tertiary grafting. Particulate AutoBT with collagen membrane was placed in the defect site and re-entered after 3.5 months for implant surgery which was subsequently loaded after six months. Six months follow-up post prosthesis placement showed no evident clinical or radiographic finding directing towards implant failure.
ALLOGRAFTS
While autografts avoid rejection, they are often unacceptable to patients because of second surgical procedure, associated pain, risk of injury and increased hospitalization time especially during tertiary grafting. Also, large defects often warrant an increased amount of graft which the autologous sites may fail to provide due to anatomical and functional limitations. When using tibial grafts, it is observed that graft from both legs might be required to meet the recipient’s need, while mandibular graft has an increased risk of sensory alteration and damage to teeth roots.30 Alloplastic grafts do not limit supply and make the procedure less invasive, countering these drawbacks. It also eliminates the requirement of additional professionals for obtaining autologous bone. However, economic considerations show mixed observations.31 Exhibiting substantial osteogenic and angiogenic potential, allografts are commonly used in combination with autologous sources to decrease integration time and achieve enhanced results.
Blume et al.32 did tertiary grafting using alloplastic graft from cancellous femur head of patient undergoing total hip replacement. The graft was milled using 3-dimensional (3D) models and augmented with autologous platelet-rich fibrin (PRF) matrix at the time of placement. Two dental implants were placed at the site after six months and cone-beam computed tomography was recorded as baseline data. These baselines were compared six months post-operatively which revealed bone resorption of approximately 3% and 1% in horizontal and vertical bone levels, respectively.
As a randomized control trial (RCT), Shirani et al.33 compared the effectiveness of autogenous iliac bone+plasma with freeze-dried bone+plasma wherein they did not associate the material to the type of bone grafting but concluded autogenous bone to be superior.
XENOGRAFT
Xenografts are obtained from species different from humans and are mostly of bovine or porcine origin. They have shown good results and can be used alone or in combination with other synthetic materials.
Hengjeerajaras et al.34 treated a cleft patient with xenogenic graft and resorbable collagenous membrane. A dental implant was placed six months after a repair which was loaded after additional three months. At a 10-year follow-up, bone levels of the area were maintained with satisfactory esthetics and functionality.
ALLOPLASTIC GRAFT MATERIALS
Synthetic in origin, alloplastic provides excellent osteogenic, osteoconductive, mesenchymal differentiation and angiogenic properties.35 These can be based on various compositions such as ceramic, polymer or growth factor enhanced and have been used for a variety of craniomaxillofacial defects. They also potentiate the bone-forming capabilities of autogenous or allogenic grafts.35
Bone morphogenetic protein (BMP)
BMPs belong to the superfamily of transforming growth factor-beta with potent bone and cartilage forming capacity.35 Depending on micro-environment and interactions, they contribute to differentiation, proliferation, growth inhibition, and maturation arrest of various cells.36 Recombinant human BMP (rhBMP-2 and -7) are growth factor enhanced materials, commercially available for craniofacial surgeries.37
Le et al.31 successfully utilized human mineralized allograft alone and in combination with BMP for alveolar repair and implant placement. While one case was treated as late secondary alveolar bone grafting, the second underwent tertiary grafting. Both showed good quality bone formation with minimal resorption and the absence of repeat procedures at the time of implant placement. Histologic assessment showed new bone formation with properties comparable to the native bone.
Comparing BMP-2 and iliac bone for late secondary cleft repair, Dickinson.38 found fewer complications in patients treated with the former. Statistically significant, higher values for graft uptake (2.8±0.2) with better radiographic bone healing were seen with BMP-2 compared to iliac bone (1.9±0.4) (p-value <0.05). BMP-2 also showed enhanced bone mineralization on panoramic and 3D assessments (2.9±0.3 compared to 2.0±0.8; p-value <0.05).
Tricalcium phosphate (TCP) and biphasic calcium phosphate (BCP)
β-TCP is one of the many available forms of calcium-based ceramic with excellent osteoconductive properties. They have lower calcium to phosphate ratio than in hydroxyapatites (HA) which may help in its faster degradation and absorption.35 β-TCP has found application in SABG in few conducted studies with favorable results, however, its ability as of late secondary or tertiary grafting material largely remains unexplored.39
Du et al.39 in their 12-month follow-up trial, performed SABG or late secondary grafting in 20 unilateral cleft patients. Based on the patient’s wish, 10 were treated with autogenous iliac crest graft (group 1) and the remaining were treated with bone marrow mononuclear cells from iliac bone combined with β-TCP (group 2). Only four patients received late grafting, two in each group. Both patients of group 2, assessed radiographically, had non-union of bone after 12 months. The study derived no conclusions on this aspect and cumulatively observed equivalent radiographic results for both groups.
Saint-Surin et al.40 used a bone graft from autogenous (cranial or endo-oral sampling) or allogenic (BCP-based) material for restoration with no loss of implant integrity in any case. Due to lack of available information, accuracy regarding late secondary, or tertiary grafting could not be determined but all cases were performed in more than 18-year old.
DISCUSSION
Treatment prospective for replacing missing teeth has shifted from “meeting functional requirements” to a holistic approach encompassing functional and esthetic needs.41 Dental implant-based rehabilitation is increasingly used, not just for healthy individuals, but also for cleft patients. However, it's common to have inadequate bone levels in defect sites despite performing SABG. Secondary grafting is performed around 9-12 years of age, and dental implants cannot be placed till skeletal maturity is achieved, to avoid hindrance in the growth of the maxillofacial complex. 3D evaluation has reported 51% and 52% bone loss after one and two years of grafting, respectively. This value can be as high as 95% at the end of one year if the repaired cleft is adjacent to an absent tooth.42 Also, a few patients do not undergo secondary grafting at the desired time, presenting a bone of poor quality, the deficit for prosthesis support.20 In these cases it is a pre-requisite to perform grafting for bone augmentation.
In addition to the patient’s medical history, environmental and habitual factors, the implant’s clinical success is strongly dependent on achieved osseointegration. It is important that the used material exhibits properties of osteogenesis, osteoinduction and, osteoconduction.35
One of the first observations through the current review is the absence of unanimous meaning of different alveolar cleft grafting procedures. This was especially seen with the use of late secondary and tertiary grafting. This at times led to difficulty in interpreting the study’s findings. This is highlighted because uniformity of terms is important so that further comparisons and illustrations, such as the one presented, are done smoothly, and can provide observations based on published findings rather than self-derivations and interpretations.
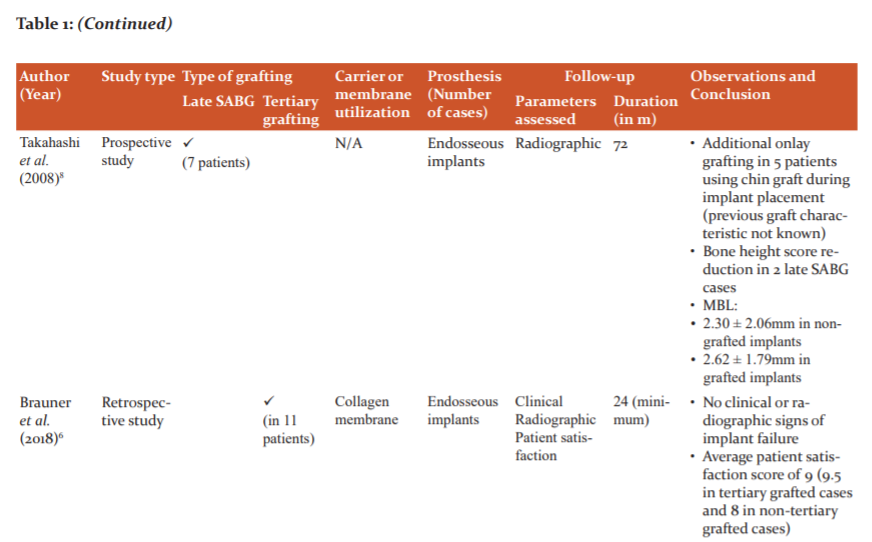
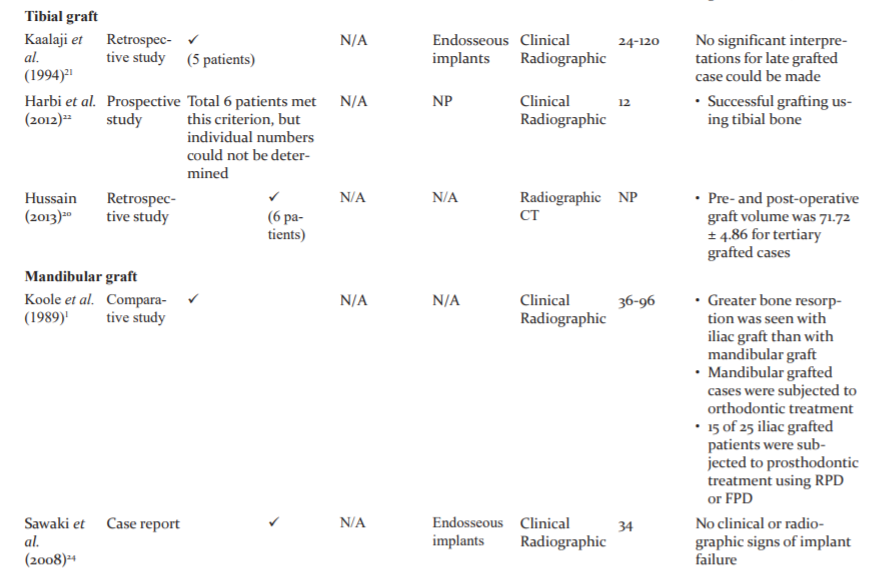
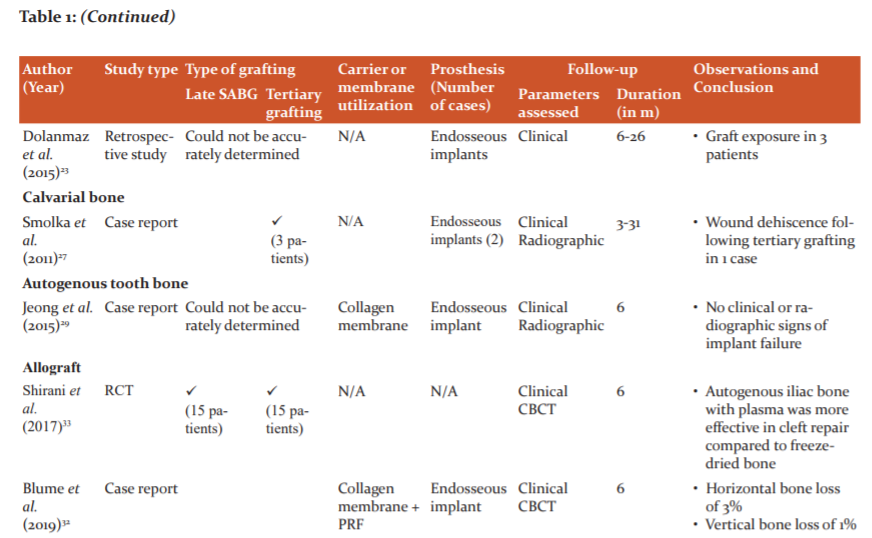
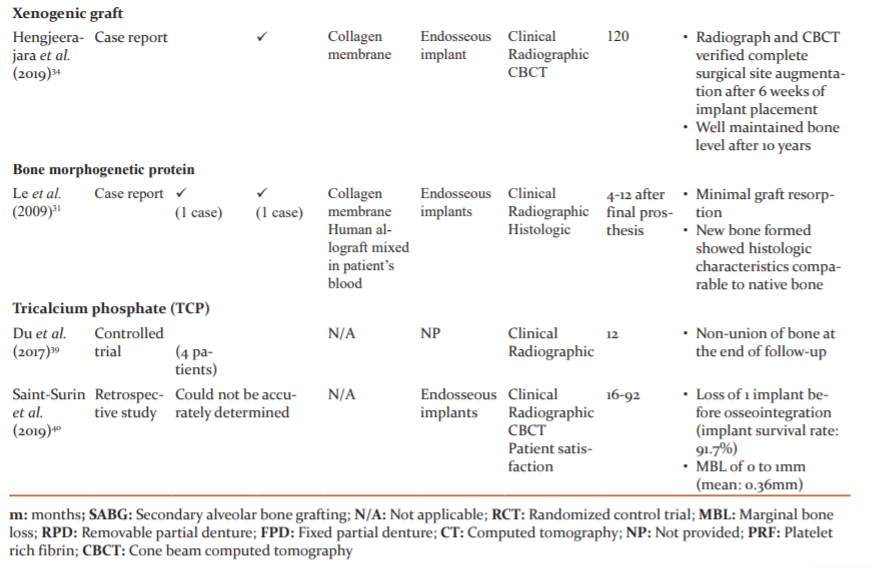
A variety of materials are available most of which have been used for SABG. However, there is limited knowledge involving the success of materials used for late and tertiary grafting. Our search showed that most of the published literature is retrospectively analyzed, emphasizing the need for prospective studies, preferably RCTs. Also, these researches have focused more on patient satisfaction and esthetics with only a few of assessing the quality and quantity of graft (Table 1). While knowing patient satisfaction and esthetics is important, other aspects such as graft characteristics should be given due consideration.
Autogenous iliac bone graft was most popular choice despite concerns about hospital stay, associated pain and post-operative gait modifications. This can be because autologous iliac grafts are time-tested and present negligible disadvantages compared to many advantages. However, new grafts are actively searched for because of increased resorption of iliac graft (30% to 43.1%).11
Many studies compared clinical outcomes of secondary and late secondary grafting wherein the former had a higher podium standing.17,19 However, these reports did not report long-term follow-up findings and rehabilitations.13,18 Thus, it is difficult to comment whether a need for future repeat grafting in SABG cases when adequately performed with a specific graft material was eliminated or not. Also, it restricted our findings to a listing of grafting materials used instead of a wholesome evaluation of graft characteristics.
Other anatomic sources have also been utilized like the fifth to the seventh rib.42,43 However for cleft cases the source is not very popular due to donor site morbidity, visible scarring, and graft overgrowth.7,21 Calvarial bone provides remarkable mechanical properties with decreased resorption which makes it a popular choice for rectifying craniofacial defects including the alveolar cleft.29,30,44 Although requiring more precision, a full-thickness calvarial cortex can be safely harvested in adults.7 In our search we came across only a few studies using calvaria for tertiary grafting, highlighting the need for further probing.30
There are a plethora of allogenic and alloplastic materials which have found substantial basing in bone repair. Focus is gradually shifting towards alloplastic as it overcomes the limitation of available quantity which can be a potential issue even with allografts. It also negates the possible prospect of immunogenic response, a great risk factor with allografts.
Stem cell regenerative medicine is fast gaining popularity among researchers with bone marrow mesenchymal cells from iliac aspirate being the most widely used source. There are also other potential sources including those in the oral cavity which are easily accessible to a maxillofacial surgeon.45 There application in cleft repair is not limited to SABG but has its use in adults as well, discussing which is not under the scope of this review.46
Successful use of 3D scaffolds in animal models is a new development that combines technology with surgical skills.47These results instil hope for their clinical use in humans.
It has been hypothesized that; functional loading of the grafted bone helps in maintaining the alveolar dimensions. Dental implants meet this aspect which conventional replacements fail to achieve. There are huge variations in the time duration between grafting and implant placement. For SABG, according to one hypothesis, implants should be placed within 4-6 months of grafting with a lack of similar consensus for late secondary or tertiary grafting.11 This highlights the need for prospective follow-up studies.
CONCLUSION
Autologous, allogeneic, and alloplastic grafts have proven their worth as suitable grafting materials and present their advantages and limitations. Recipient site, operator’s expertise, patient’s acceptance and monetary capabilities direct the selection of appropriate bone graft material. Stem cells and 3D printing provide promising results for the future and any minor findings should be encouraged. Clinicians should also be encouraged to undertake long-term follow-up RCTs, wherein information of both, grafting and rehabilitative procedure outcomes are reported.
Acknowledgement: Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
Conflict of Interest: Nil
Source of funding: Nil
Author Contribution
Dr. Rizwana Mallick: Concept design, Definition of intellectual content, Literature search, Data acquisition, Data analysis, Manuscript preparation, Manuscript editing, Manuscript review
Dr. Sweta K. Pisulkar: Concept design, Manuscript editing, Manuscript review
Dr. Srinivas Gosla Reddy: Concept design, Manuscript editing, Manuscript review
References:
1. Koole R, Bosker H, Dussen FN van der. Late Secondary Autogenous Bone Grafting in Cleft Patients Comparing Mandibular (Ectomesenchymal) and Iliac Crest (Mesenchymal) Grafts. J Oral Maxillofac Surg. 1989; 17(Suppl 1):28–30.
2. Myeroff C, Archdeacon M. Autogenous bone graft: donor sites and techniques. J Bone Joint Surg Am. 2011; 93(23):2227–36.
3. Ahlmann E, Patzakis M, Roidis N, Shepherd L, Holtom P. Comparison of Anterior and Posterior Iliac Crest Bone Grafts in Terms of Harvest-Site Morbidity and Functional Outcomes. J Bone Joint Surg Am. 2002; 84(5):716–20.
4. Abramowicz S, Katsnelson A, Forbes PW, Padwa BL. Anterior versus posterior approach to iliac crest for alveolar cleft bone grafting. J Oral Maxillofac Surg. 2012; 70(1):211–5.
5. Ronchi P, Chiapasco M, Frattini D. Endosseous implants for prosthetic rehabilitation in bone grafted alveolar clefts. J Craniomaxillofac Surg. 1995; 23(6):382–6.
6. Brauner E, De Angelis F, Jamshir S, Mezi S, Tiroli RC, Pompa G et al. Aesthetic satisfaction in lip and palate clefts: A comparative study between secondary and tertiary bone grafting. Clin Ter. 2018; 169(2):e62–6.
7. Takahashi T, Fukuda M, Yamaguchi T, Kochi S. Use of endosseous implants for dental reconstruction of patients with grafted alveolar clefts. J Oral Maxillofac Surg. 1997; 55(6):576–83.
8. Takahashi T, Inai T, Kochi S, Fukuda M, Yamaguchi T, Matsui K et al. Long-term follow-up of dental implants placed in a grafted alveolar cleft: evaluation of alveolar bone height. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 105(3):297–302.
9. Härtel J, Pögl C, Henkel KO, Gundlach KKH. Dental implants in alveolar cleft patients: a retrospective study. J Craniomaxillofac Surg. 1999; 27(6):354–7.
10. Dempf R, Teltzrow T, Kramer FJ, Hausamen JE. Alveolar bone grafting in patients with complete clefts: A comparative study between secondary and tertiary bone grafting. Cleft Palate Craniofac J. 2002; 39(1):18–25.
11. Matsui Y, Ohno K, Nishimura A, Shirota T, Kim S, Miyashita H. A long-term study of dental implants placed into alveolar cleft sites. Cleft Palate Craniofac J. 2007; 44(4):444–7.
12. Matsui Y, Ohta M, Ohno K, Nagumo M. Alveolar Bone Graft for Patients with Cleft Lip/Palate Using Bone Particles and Titanium Mesh: A Quantitative Study. J Oral Maxillofac Surg. 2006; 64(10):1540–5.
13. Uzel A, Benliday? ME, Kürkçü M, Kesikta? E. The Effects of Maxillary Expansion on Late Alveolar Bone Grafting in Patients with Unilateral Cleft Lip and Palate. J Oral Maxillofac Surg. 2019; 77(3):607–14.
14. Mahajan R, Ghildiyal H, Khasgiwala A, Muthukrishnan G. Evaluation of Secondary and Late Secondary Alveolar Bone Grafting on 66 Unilateral Cleft Lip and Palate Patients. Plast Surg (Oakv). 2017; 25(3):194–9.
15. Jeyaraj P, Sahoo NK, Chakranarayan A. Mid Versus Late Secondary Alveolar Cleft Grafting Using Iliac Crest Corticocancellous Bone Graft. J Maxillofac Oral Surg. 2014; 13(2):195–207.
16. Garcia MA, Yatabe M, Fuzer TU, Calvo AM, Trindade-Suedam IK. Ideal Versus Late Secondary Alveolar Bone Graft Surgery: A Bone-Thickness Cone-Beam Computed Tomographic Assessment. Cleft Palate Craniofac J. 2018; 55(3):369–74.
17. Trindade-Suedam IK, Filho OGS, Carvalho RM, Faco RAS, Calvo AM, Ozawa TO et al. Timing of Alveolar Bone Grafting Determines Different Outcomes in Patients With Unilateral Cleft Palate. J Craniofac Surg. 2012; 23(5):1283–6.
18. Chowdhury SKR, Menon PS, Vasant MR, Jayan B, Dhiman RK, Karkun S. Secondary and delayed bone grafting in alveolar and anterior palatal clefts. Med J Armed Forces India. 2006; 62(3):231–5.
19. Coots BK. Alveolar bone grafting: Past, present, and new horizons. Semin Plast Surg. 2012; 26(4):178–83.
20. Hussain S. Evaluation of alveolar grafting with tibial graft in adolescent patients. Indian J Dent Res. 2013; 24(6):659–63.
21. Kalaaji A, Lilja J, Elander A, Friede H. Tibia as Donor Site for Alveolar Bone Grafting in Patients With Cleft Lip and Palate: Long-Term Experience. Scand J Plast Reconstr Surg Hand Surg. 2001; 35(1):35–42.
22. Al Harbi H, Al Yamani A. Long-term follow-up of tibial bone graft for correction of alveolar cleft. Ann Maxillofac Surg. 2012; 2(2):146.
23. Dolanmaz D, Esen A, Y?ld?r?m G, ?nan Ö. The use of autogenous mandibular bone block grafts for reconstruction of alveolar defects. Ann Maxillofac Surg. 2015; 5(1):71-6.
24. Sawaki M, Ueno T, Kagawa T, Kanou M, Honda K, Shirasu N et al. Dental Implant Treatment for a Patient With Bilateral Cleft Lip and Palate. Acta Med Okayama. 2008; 62(1):59–62.
25. Sadove AM, Nelson CL, Eppley BL, Nguyen B. An Evaluation of Calvarial and Iliac Donor Sites in Alveolar Cleft Grafting. Cleft Palate Craniofac J. 1990; 27(3):225–9.
26. Smolka W, Eggensperger N, Carollo V, Ozdoba C, Iizuka T. Changes in the volume and density of calvarial split bone grafts after alveolar ridge augmentation. Clin Oral Implants Res. 2006; 17(2):149–55.
27. Smolka W, Smolka K. Tertiary bone grafting using calvarial bone transplants in patients with cleft lip and alveolus. Oral Surg. 2011; 4(3):135–9.
28. Gual-Vaqués P, Polis-Yanes C, Estrugo-Devesa A, Ayuso-Montero R, Marí-Roig A, López-López J. Autogenous teeth used for bone grafting: A systematic review. Med Oral Patol Oral Cir Bucal. 2018; 23(1):e112–9.
29. Jeong K-I, Lee J, Um I-W, Kim Y-K. Alveolar Cleft Restoration Using Autogenous Tooth Bone Graft Material for Implant Placement: A Case Report. J Oral Implantol. 2015; 41(4):487–90.
30. Reininger D, Cobo-Vázquez C, Monteserín-Matesanz M, López-Quiles J. Complications in the use of the mandibular body, ramus and symphysis as donor sites in bone graft surgery. A systematic review. Med Oral Patol Oral Cir Bucal. 2016; 21(2):e241–9.
31. Le BT, Woo I. Alveolar Cleft Repair in Adults Using Guided Bone Regeneration With Mineralized Allograft for Dental Implant Site Development: A Report of 2 Cases. J Oral Maxillofac Surg. 2009; 67(8):1716–22.
32. Blume O, Back M, Born T, Donkiewicz P. Reconstruction of a Unilateral Alveolar Cleft Using a Customized Allogenic Bone Block and Subsequent Dental Implant Placement in an Adult Patient. J Oral Maxillofac Surg. 2019; 77(10):2127.e1-11.
33. Shirani G, Abbasi AJ, Mohebbi SZ, Moharrami M. Comparison between autogenous iliac bone and freeze-dried bone allograft for the repair of alveolar clefts in the presence of plasma rich in growth factors: A randomized clinical trial. J Craniomaxillofac Surg. 2017; 45(10):1698–703.
34. Hengjeerajaras P, Froum S, Adawi H, Yu P, Cho S-C. Anterior Tooth Replacement with an Implant in a Grafted Alveolar Cleft Site: Case Report with a 10-Year Follow-up. Int J Periodontics Restorative Dent. 2019; 39(4):511–5.
35. Kumar P, Vinitha B, Fathima G. Bone grafts in dentistry. J Pharm Bioallied Sci. 2013; 5(SUPPL.1):1–6.
36. Chenard KE, Teven CM, He TC, Reid RR. Bone morphogenetic proteins in craniofacial surgery: Current techniques, clinical experiences, and the future of personalized stem cell therapy. J Biomed Biotechnol. 2012; 2012.
37. Dickinson BP, Ashley RK, Wasson KL, O’Hara C, Gabbay J, Heller JB et al. Reduced morbidity and improved healing with bone morphogenic protein-2 in older patients with alveolar cleft defects. Plast Reconstr Surg. 2008; 121(1):209–17.
38. Janssen NG, Schreurs R, de Ruiter AP, Sylvester-Jensen HC, Blindheim G, Meijer GJ et al. Microstructured beta-tricalcium phosphate for alveolar cleft repair: a two-centre study. Int J Oral Maxillofac Surg. 2019; 48(6):708–11.
39. Du F, Wu H, Li H, Cai L, Wang Q, Liu X et al. Bone Marrow Mononuclear Cells Combined with Beta-Tricalcium Phosphate Granules for Alveolar Cleft Repair: A 12-Month Clinical Study. Sci Rep. 2017; 7(1):1–8.
40. Saint-Surin I, Roman T, Touzet-Roumazeille S, Ferri J, Lauwers L. Implant-borne rehabilitation for alveolar dental cleft: Retrospective analysis of thirty-nine cases. J Stomatol Oral and Maxillofac Surg. 2020. 121(4):339-43.
41. Pisulkar SK, Agrawal R, Belkhode V, Nimonkar S, Borle A, Godbole SR. Perception of Buccal Corridor Space on Smile Aesthetics among Specialty Dentist and Layperson. J Int Soc Prev Community Dent. 2019; 9(5):499–504.
42. Feichtinger M, Zemann W, Mossböck R, Kärcher H. Three-dimensional evaluation of secondary alveolar bone grafting using a 3D- navigation system based on computed tomography: a two-year follow-up. Br J Oral Maxillofac Surg. 2008; 46(4):278–82.
43. Witsenburg B, Freihofer HPM. Autogenous rib graft for reconstruction of alveolar bone defects in cleft patients. J Craniomaxillofac Surg. 1990; 18(2):55–62.
44. Balaji S. Maxillary Cleft Surgery with Rib Graft. 2019. Available from: https://www.smbalaji.com/maxillary-cleft-surgery-with-rib-graft/
45. Hudak KA, Hettinger P, Denny AD. Cranial Bone Grafting for Alveolar Clefts: A 25-year Review of Outcomes. Plast Reconstr Surg. 2014; 133(5):662e-8e.
46. Sybil D, Jain V, Mohanty S, Husain SA. Oral stem cells in intraoral bone formation. J Oral Biosci. 2020; 62(1):36–43.
47. Korn P, Ahlfeld T, Lahmeyer F, Kilian D, Sembdner P, Stelzer R et al. 3D Printing of Bone Grafts for Cleft Alveolar Osteoplasty – In vivo Evaluation in a Preclinical Model. Front Bioeng Biotechnol. 2020; 8:217.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License