IJCRR - 13(16), August, 2021
Pages: 123-128
Date of Publication: 30-Aug-2021
Print Article
Download XML Download PDF
Assessment of Psychiatric Illness Among Patients with Dermatological Disorders Attending a Tertiary Care Hospital of Rajnandgaon District (C.G), India
Author: Pooja Pandey, Sharad M Manore, Prabhat Pandey, Neeraj Dokania
Category: Healthcare
Abstract:Introduction: Skin plays a major role in social and sexual communication. Healthy normal skin is essential for a person's physical and mental well-being and sense of self-confidence. Material and Method: The cross-sectional study with consecutive sampling was conducted at a tertiary care hospital at BRLSA�BVM Medical College and hospital, Rajnandgaon (C G), India. A total of 170 patients participated in the study. Patients suffering from dermatologic diseases who accepted to participate in the study were included in the study population regardless of their sex, age, education level and marital status. Patients were asked to complete five other areas questionnaires: DLQI, PHQ-9, PHQ-15, HAM-D and GAD-7. Results: The mean age of the participants was 27.25. Out of 170 patients, Acne with scar is the common diagnosis i.e., 61 (35.9%) followed by fungal infection 45 (26.5%) and Pigmentary disorder 25 (14.7%). There was a significant relationship between dermatological disorders with DLQI score, PHQ-9, HAM-D and PHQ-15. However, no significant relationship was observed between the GAD-7 with the dermatological disorder. Conclusion: There is a need for a thorough assessment of psychiatric illness in patients with dermatological conditions and regarding improving the patient management and overall quality of life.
Keywords: Anxiety, Depression, Acne, Fungal infection, Dermatological disorder, Psychological problem
Full Text:
INTRODUCTION -
Skin plays a major role in social and sexual communication. Healthy normal skin is essential for a person’s physical and mental well-being and sense of self-confidence.1The relation between psychiatry and skin diseases can be evaluated from two aspects: On one hand, psychiatric co-morbidity influences the development and course of dermatologic diseases via the effects of stress, depression, and anxiety.2 On the other hand, cosmetically disfiguring dermatologic diseases may cause significant psychosocial distress for patients.3 Co-morbid mental illness plays a substantial role in the course, severity, response to therapy and therefore the psychosocial well-being of the dermatologic patients. It seems that co-morbid mental illness and its consequences on patients' quality of life have been underappreciated. Therefore, understanding the prevalence of psychiatric co-morbidity and its potential effects on patients' lives may lead to changes in management approaches and ultimately to improve the patients' outcome.
As per available previous studies, strong association is found between dermatological condition and psychological problems.4Approximately 30% and 40% incidence of psychiatric disorders among dermatological patients was observed.5
When assessing dermatological patients, it is best to adopt a multidimensional, biopsychosocial approach, which allows for relative contributions of biological, psychiatric and psychosocial factors, because it may not be possible clearly to determine whether a psychiatric syndrome is primary or entirely secondary to the dermatological condition.6Acne, tineacorporis, vitiligo, scabies, melasma, STIs etc are some commonly occurring disorders and can be psychologically devastating to patients with darker skin type. It can lead to cosmetic disfigurement and affect psychosocial and psychosexual identity. Research have shown that resolution of all these disorders can improve the quality of life. Improvements have been seen in the areas of feeling self-conscious about the skin or being scrutinized by others, feeling unattractive, using cosmetics to cover up the disease and limiting social or leisure activities because of appearance of the skin.7As per available previous research, visible dermatologic skin conditions were significantly affecting the quality of life and psychosocial functioning.8-11
In the present study the aim is to find out the magnitude of anxiety and depression in common dermatological patients and its association with dermatological diagnosis.
MATERIAL AND METHODS-
This cross-sectional study with consecutive sampling was conducted at BRLSABVM Medical College and hospital, Rajnandgaon (C G), India. A total of 170 patients participated in the study during the period July 2020 to December 2020.
Patients suffering from dermatologic diseases who gave informed consent to participate in the study were included in study population regardless of their age, sex, education level and marital status. Subjects were evaluated on a brief semi-structured Performa for collecting demographic and clinical information. Performa was converted in the local language for their convenience. Ethical consideration was made through institutional ethical committee (No./13/GMC/I.E.C./2017. Rajnandgaon)
The questionnaire consists of two parts. In the first part, the demographic characteristics and its related information were collected; and in the second part, five other areas questionnaires were used: DLQI, PHQ-9, HAM-D and GAD-7, PHQ-15. 12-16
Inclusion criteria- Patients suffering from dermatological problem attended OPD.
Exclusion criteria-
-
Patients having chronic diseases other than dermatological problem.
-
Past history of psychological illness.
-
Apparent life stress other than skin disease.
-
Those who were younger than 15 years of age and who did not give informed consent.
Data was recorded in MS Excel and checked for its completeness and correctness then it was analyzed by using suitable statistical software and p-value < 0.05 was considered as statistically significant.
RESULTS-
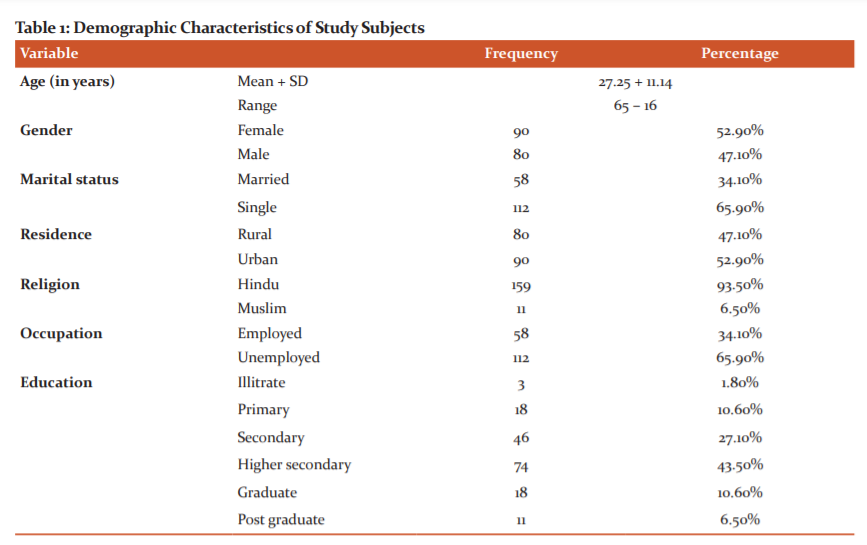
Majority of the patients 60% belongs to the age group of 16 to 25 years. Out of the total 170 study subjects, 47.1% were males and 52.9% were females. 34.1% of the study subjects were married and 65.9% were single. Most of study patients were Hindu by religion and out of 170 patients 90 were from urban and 80 were from rural background. 65.9% of the study subjects were unemployed and 34.1% were employed. Majority of the study subjects 43.5% studied up to higher secondary and only 6.5% were post-graduate.TABLE.1
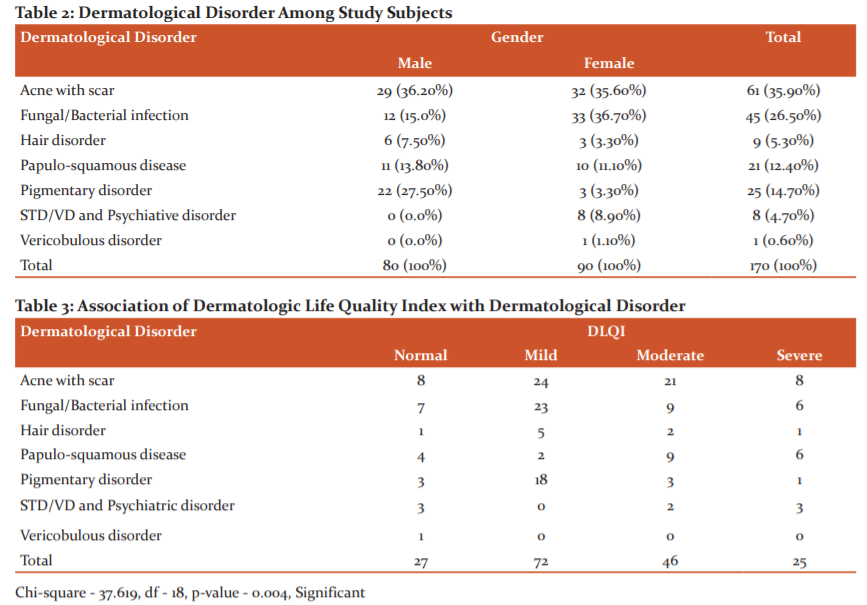
Out of 170 patients, Acne with scar is the common diagnosis i.e., 61 (35.9%) followed by fungal infection 45 (26.5%) and Pigmentary disorder 25 (14.7%). TABLE.2
Among the patients with Acne, the quality of life of most of the patients was severely affected, indicating a poor quality of life. Most of them with Bacterial infection also scored high in the DLQI score and were mild, moderately and severely affected. The majority with Papulo-squamous disease were mild, moderately and severely affected. There was a significant association between quality of life and Dermatological Disorder. TABLE.3
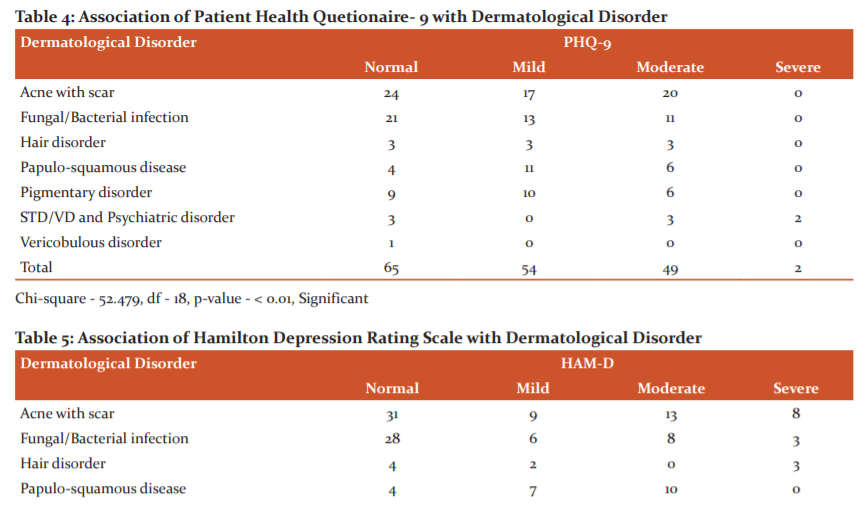
On assessing the severity of depression using PHQ-9, Only 2 patients had severe depression due to STD/VD and Psychiatric disorder and the majority of the subjects had mild and moderate depression due to Acne with scar. Diagnosed depression and grade severity of symptoms in general medical and mental health was found statistically significantly associated with Dermatological Disorder. TABLE.4
Thirty patients with acne had clinical depression followed by 34 patients with mild, moderate and severe depression due to bacterial infection and Papulo-squamous disease.Dermatological Disorder were found to be associated to depression.TABLE.5
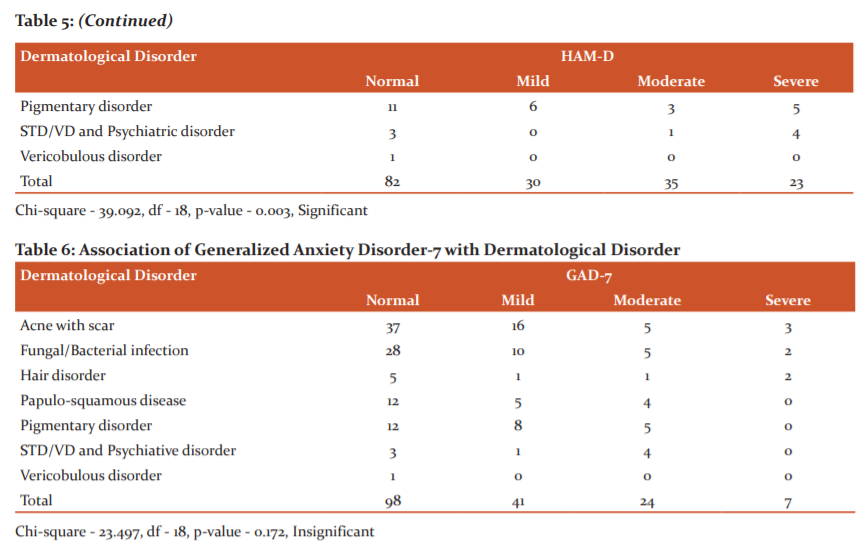
Out of total 170 subjects, Majority of them had mild, moderate and severe anxiety due to Acne with scar. There was no significant association found between Dermatological Disorder and anxiety. TABLE.6
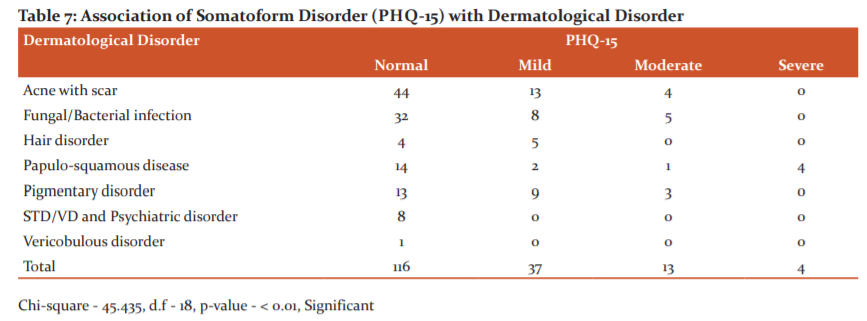
On assessing the somatic symptom subscale using PHQ-9, 13 patients had mild and 4 patients had moderate somatic disorder due to Acne. Only 4 patients had severe somatic disorder Papulo-squamous disease. Somatic disorder was found statistically significantly associated with Dermatological Disorder.TABLE.7
DISCUSSION-
Dermatological problems varies from region to region all over the world and also vary depending on different socio-demographic, socio-economic and climatic factors. In the present study, relatively more females (n = 90) attended the OPD than males (n = 80). A similar pattern female to male proportion was found in the study by Kosaraju S.K et al. and Kuruvilla et al. in South India. The more male patient proportion was found in the study conducted by Kar et al. in a Tertiary Care Centre.17-19Most of the patients were from below <45 years age group and females were more. Similar type of finding were also known by Emmanouil K.S et al. in their study and Baur D.B et al.20,21In our study Hindu patients were more whereas this was contrary to a study done by Baur D.B et al. The study by Florence Dalgard et al. showed that there were ethnic and gender differences in the reporting of skin complaints.22
Our study showed that Acne with scar was the commonest form of dermatological presentation, followed by Bacterial infection. Whereas in a study done by Baur D.B et al. Scabies was the commonest form of dermatological presentation, followed by Tinea infection. 21In the study done by Emmanouil K S found Allergic dermatitis and Urticaria (35.7%) were most commonly found cutaneous disorder followed by infectious diseases (26.1%).20The study in Dermatology O.P.D of Gauhati Medical college in India by Das KK observed that Eczema, Pyoderma, Fungal infections and Psoriases were the major dermatological problems whereas Devi T in their study found that Eczema, Fungal, Pyoderma and Scabies were the major skin diseases.23,24 Skin diseases with high prevalence of psychiatric disorders in our study included acne with scar Bacterial infection, Pigmentary disorder and Papulo-squamous disease. The higher anxiety level in patients with acne was expected because of the widely recognized psychological impact of the disease. Many studies have reported elevated anxiety, marked impairment in emotional well being, death wishes and suicidal tendencies in patients with acne.25
The proportion of depression in dermatological patients varies according to the location, diagnosis of the patients and the tool used to assess depression.26,27Acne has a demonstrable association with depression and anxiety and psychiatric co-morbidity of acne vulgaris includes body image disorder, depression, anxiety, obsessive-compulsive disorder (OCD), delusional disorders, personality disorders and social phobias.28,29It has been reported that young men with severe scarring acne are at particular risk of depression and suicide.30In the current study, the proportion of depression and anxiety in dermatological patients was 51.76 % and 42.5% respectively. Kim et al. in his study also found that nearly 62.5% of the patients with skin diseases had clinical depression.31
CONCLUSION-
The present study confirmed an association between dermatological condition and psychiatric illness. Female patients suffered from more anxiety and depression than males. It can be concluded that there is a need for a thorough assessment of psychiatric illness in patients with long-term dermatological conditions, this will help in improving the patient management and overall quality of life. Dermatologists should be aware about the psychiatric illness and appropriate referral should be made.
CONFLICT OF INTERESTS-
The authors declare that they have no conflict of interests.
FINANCIAL SUPPORT- None
ACKNOWLEDGMENTS- Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
-
Aktan S, Ozmen E, Sanli B. Psychiatric disorders in patients attending a Dermatology outpatient clinic. Dermatology 1998; 197: 230-4.
-
Schultz HY. Society for Investigative Dermatology Skin Disease Comorbidities Project Launch Conference Proceedings. J Invest Dermatol 2009; 129: 525–528.
- Gupta MA. Psychiatric comorbidity in dermatologic disorders. In: walker C ,papadoulos L, eds. Psychodermatology. Cambridge: Cambridge University Press; 2005.
-
Shenoi SD, Prabhu S, Nirmal B, Petrolwala S. Our experience in a psychodermatology liaison clinic at Manipal, India. Indian J Dermatol.2013;58:53-5.
-
Ghosh S, Behere RV, Sharma P, Sreejayan K. Psychiatric evaluation in dermatology: An overview. Indian J Dermatol. 2013;58:39–43.
-
Gupta MA, Gupta AK, Ellis CN, Koblenzer CS. J CosmetDermatol. Psychiatric evaluation of the dermatology patient. 2008 Sep;7(3):164-8.
-
Taylor A, Pawaskar M, Taylor SL, Balkrishnan R, Feldman SR. Prevalence of pigmentary disorders and their impact on quality of life: a prospective cohort study.
-
Langley RG et al. Ustekinumab signi?cantly improves symptoms of anxiety, depression, and skin-related quality of life in patients with moderate-to-severe psoriasis: results from a randomized, double-blind, placebo-controlled phase III trial. J Am AcadDermatol. 2010;63:457–65.
-
Yazici K et al. Disease-speci?c quality of life is associated with anxiety and depression in patients with acne. J EurAcadDermatolVenereol. 2004;18:435–
-
Linnet J, Jemec GB. An assessment of anxiety and dermatology life quality in patients with atopic dermatitis. Br J Dermatol. 1999;140:268–72.
-
Kurd SK, Troxel AB, Crits-Christoph P, Gelfand JM. The risk of depression, anxietyand suicidality in patients with psoriasis: a population-based cohort study. Arch Dermatol. 2010;146:891–5.
-
Aghaei S, Sodaifi M, Jafari P, Mazharinia N, Finlay AY. DLQI scores in vitiligo: reliability and validity of the Persian version. BMC Dermatol2004 ; 4 : 8.
-
Kroenke K, Spitzer RL, Williams JB, Validity of a Brief Depression Severity Measure. J GEN INTERN MED 2001;16:606-6
-
Iannuzzo RW, Jaeger J, Goldberg JF, Kafantaris V, Sublette ME. Development and reliability of the HAM-D/MADRS Interview: An integrated depression symptom rating scale. Psychiatry Research 145 (2006) 21–37.
-
Donker T, Straten A, Marks I, Cuijpers P. Quick and easy self-rating of Generalized Anxiety Disorder: Validity of the Dutch web-based GAD-7, GAD-2 and GAD-SI. Psychiatry Research 188 (2011) 58–64.
-
Kocalevent, RD., Hinz, A. & Brähler, E. Standardization of a screening instrument (PHQ-15) for somatization syndromes in the general population. BMC Psychiatry 13, 91 (2013).
-
Kosaraju SK et al. Psychological morbidity among dermatological patients in a rural setting. Indian J Dermatol 2015;60:635.
-
Kuruvilla M, Sridhar KS, Kumar P, Rao GS. Pattern of skin diseases in BantwalTaluq, Dakshina Kannada. Indian J DermatolVenereolLeprol 2000;66:247?8.
-
Kar C, Das S, Roy AK. Pattern of skin diseases in a tertiary institution in Kolkata. Indian J Dermatol 2014;59:209.
-
Symvoulakis E K, et al. Primary care and pattern of Skin diseases in a Mediteranean island. B M C Family Practice 2006,7:6.accessed online http:\\www.biomedcentral.com/1471- 2296/7/6.
-
Baur B, Sarkar J, Manna N, Bandyopadhyay L. The Pattern of Dermatological Disorders among Patients Attending the Skin O.P.D of A Tertiary Care Hospital in Kolkata, India. Volume 3, Issue 4 (Jan.- Feb. 2013), PP 04-09.
-
Dalgard F, Holm J, Svensson A, Kumar B, Sundby J. Self-reported skin morbidity and ethnicity: a population-based study in a western community. B M C Dermatology, June 2007,7:4
-
Das KK. Pattern of dermatological diseases in Gauhati Medical College & Hospital, Guwahati. IJDVL 2003;69(1):16-18.
-
Devi T, Zamzachin G. Pattern of skin diseases in Imphal. Indian J Dermatol 2006;51:149-50.
-
Yazici K, Baz K, Yezici AE. Disease specific quality of life is associated with anxiety and depression in patients with acne. J EurAcadDermatolVenereol 2004; 18: 435-9.
-
Picardi A et al. Recognition of depressive and anxiety disorders in dermatological outpatients. ActaDermVenereol 2004;84:213-7.
-
Picardi A et al. Psychosomatic assessment of skin diseases in clinical practice. PsychotherPsychosom 2005;74:315-22.
-
Koo JY, Smith LL. Psychologic aspects of acne. PediatrDermatol. 1991;8:185–8.
-
Bach M, Bach D. Psychiatric and psychometric issues in acne excoriee. PsychotherPsychosom. 1993;60:207–10.
-
Gupta MA, Gupta AK, Schork NJ. Psychosomatic study of self-excoriative behavior among male acne patients: Preliminary observations. Int J Dermatol. 1994;33:846-8.
-
Kim EK et al. Prevalence and risk factors of depression in geriatric patients with dermatological diseases. Ann Dermatol 2013;25:278?84.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License