IJCRR - 13(16), August, 2021
Pages: 58-62
Date of Publication: 30-Aug-2021
Print Article
Download XML Download PDF
Comparison between Device Closure and Surgical Method of Closure in Atrial Septal Defects in a Tertiary Health Care Setup
Author: Manoj Kumar, Navneet K Srivastva, Dharmendra K Srivastava, Subhash S Rajput, Sudharshan Vijay
Category: Healthcare
Abstract:Background: Atrial septal defect (ASD) comprise 7-10% of the congenital heart diseases in adults. For decades surgical repair has been the treatment of choice with excellent survival in long term follow up. However, like every cardiac surgery, there are complications related to cardiopulmonary bypass, residual scars and mental agony. Less invasive methods such as percutaneous transcatheter device closure have been developed. Aim: To compare surgical repair and device closure methods for management of ASD in terms of efficacy, intraoperative, post-operative complications and length of hospital stay. Materials and Methods: The present study was done in a tertiary health centre in northern India and comprised of 80 patients with a proven isolated ASD who had undergone surgical repair (n=50) and device closure (n=30). They were reviewed and analysed for comparison among the two methods. Results: The successful closure rate was 100% in the surgical group and 93.3% in device closure. There was a significant difference in operative time between the surgical group and the device groups. The length of stay in the intensive care unit and postoperatively in the hospital was shorter in the device group than in the surgical group. In terms of complications, arrhythmia was seen in 16% of surgical patients and 20% device group. Wound infection/ groin hematoma was in 12% patients of surgical and in 13.3% patients of device. Conclusion: It can be summarised that surgical closure of ASD is comparable to transcatheter device closure with some limitations in either group. Procedural success is more in the surgical group with no chance of device migration and embolisation which is a fatal complication of device closure. However, the surgical group has its limitations in terms of post-operative pain and hospital stay.
Keywords: Atrial septal defect, Comparison, Congenital heart disease, Device closure, Surgery
Full Text:
Introduction: Atrial septal defect (ASD) accounts for 7-10% of congenital heart defects in adults. 1More recent epidemiological data suggest that ASD occur in 1.6 per 1000 live births. 2 This increase can be attributed to improvements in imaging technology. Advanced maternal age is also thought to be a risk factor for ASD. The gold standard in the treatment of ASD is direct surgical closure of the defect. It is associated with excellent survival in long-term follow; however, complications due to sternotomy, cardiopulmonary bypass, residual scars and mental agony do persist. Hence, in recent times ASD are being increasingly closed by transcatheter implantation of occluder devices.3The decision to manage ASD depends on technical factors. Small ASD with adequate septal rims are suitable for transcatheter closure, whereas surgical closure should have opted when the defect is too close to the atrioventricular valves, the coronary sinus, or the vena cavae.
Methods: [1]
Subjects: The study cohort comprised of 80 patients with isolated ASD during a period of twelve months August 2018 to July 2019. The inclusion criteria were an ostium secondum ASD without any associated cardiac anomaly. The patients were divided into two groups according to their treatment options. There were 50 patients in group A (surgical repair) and 30 patients in group B (Transcatheter device closure). Medical records were reviewed for demographic features like height, weight, age and their baseline characteristics like size, type of ASD and pulmonary hypertension were recorded.
Operative technique :
Surgical repair (Group A): ASD was approached by either of the three incisions- median sternotomy, right anterolateral thoracotomy and or vertical infra-axillary thoracotomy as per the patient’s height, weight and sex. A pericardial patch was used in all cases. All patients required cardiopulmonary bypass (CPB) in this group.
Transcatheter device closure (Group B): Femoral vein was used for catheterization and the defect was closed with a guidewire. Transthoracic echocardiography (TEE) and or angiography was used to assess the diameter of ASD and a corresponding occluder was placed across the defect.
Successful ASD closure was defined if they had no (<1mm colour jet width) or small (1-2mm colour jet width) on transthoracic echocardiography immediately after procedure (for device closure) and at 24-hours after the surgical repair. Operative and postoperative outcomes like duration of the procedure, CPB time/fluoroscopy time, aortic cross-clamp time, length of hospital stay, residual ASDs, total procedural success, decrease in right cardiac load (right ventricular end-diastolic diameter, tricuspid annular diameter) were noted. Complications like wound infection, pneumonia, pericardial/pleural effusion, device embolization, device endocarditis, reopening, arrhythmias, readmission were noted.
Statistical analysis was done using SPSS 16.0 version to represent the data in percentage and mean ± SD. The Chi-square test was used to compare categorical variables. The Unpaired t-test was used to compare continuous variables between the groups. The p-value<0.05 was considered significant.
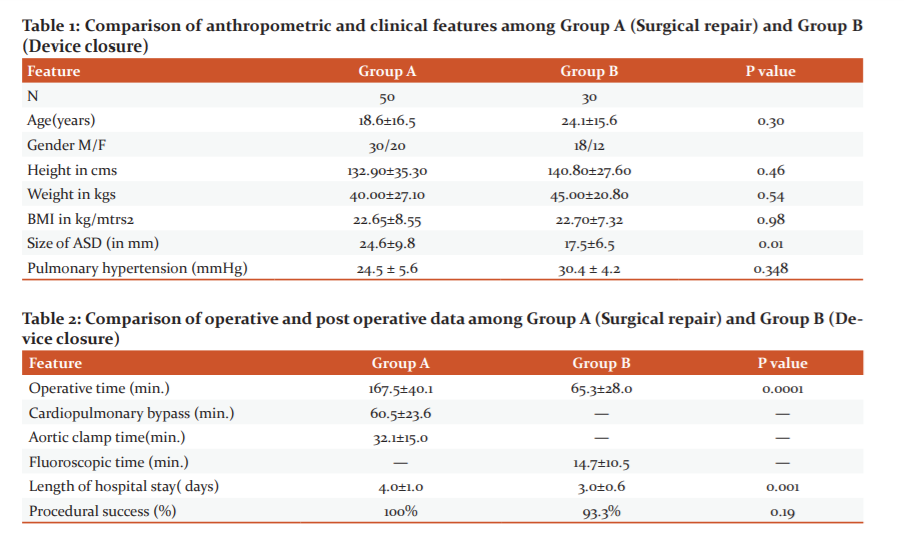
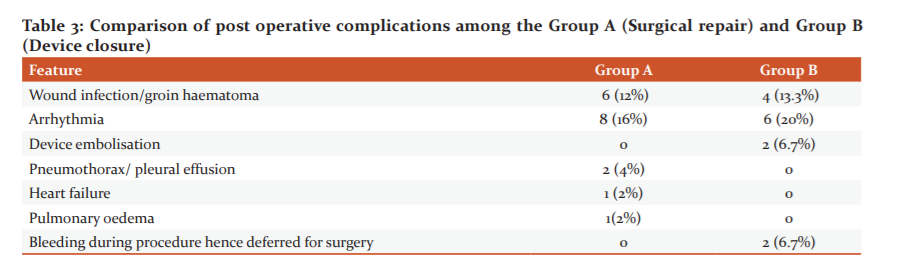
Results:[2] A total of 80 patients were evaluated in this study out of which 50 underwent surgical repair and 30 device closure. Table 1 shows the baseline clinical and demographic data. In the present study, the mean age of patients of surgical and device closure was 18.6±16.5 and 24.1±15.6 years respectively (p value - 0.3). There was no significant difference in age, anthropometric parameters and pulmonary hypertension between the groups [Table 1] [3] . The size of ASD was significantly (P=0.01) higher in surgical patients (24.6±9.8) compared to device patients (17.5±6.5) [Table 1] In the present study, the duration of surgery was significantly (P=0.0001) higher in surgical patients (167.5±40.1 minutes) compared to device patients (65.3±28.0 minutes). [Table 2]
The rate of successful ASD closure was 100% in surgical repair and 93.3% of Device patients. CPB/fluoroscopy was significantly (P=0.0001) higher in Surgical patients (60.5±23.6 minutes) compared to Device patients (14.7±10.5 minutes) [Table 2] .
Regarding the postoperative length of hospital stay, it was significantly (P=0.001) higher in surgical patients (4.0±1.0 days) compared to device patients (3.0±0.6 days). Arrhythmia, wound infection/ groin hematoma and device embolization was more common in group b (20%, 13.3% and 6.7% respectively) compared to group A (16%, 12%, 0% respectively). [Table 3] All patients were followed up for 12 months with complete physical examination and echocardiography follow-up period was 12 months. All patients underwent a complete physical examination and electrocardiography. None of them suffered any major complications such as sudden death, cerebral embolism or endocarditis.
Discussion: Since decades the standard treatment of choice for ASD has been surgical repair via the median sternotomy approach.4,5 Right anterolateral thoracotomy and right axillary thoracotomy can also be used for better cosmetic results.6,7 Like every surgery there are complications due to scar formation, blood transfusions and postoperative pain. With advancements in technology interventional transcatheter device closure for ASD has now gained popularity.8,9However the decision to treat ASD is based on a number of factors. ASD defect closer to the atrioventricular valves, coronary sinus, or the venae cavae require surgery whereas a small ASD with adequate septal rims is suitable for device closure. The success rate for transcatheter closure is reported to be 96% to 98%. 10
In the present study, the mean age of patients of group A and group B was 18.6±16.5 and 24.1±15.6 years respectively. Both groups had no significant difference in age (P =0.30). Ozdemiret al found the mean age of patients of transcatheter ASD closure was 36.5±14.7 years and 33.2±13.8 of surgical closure with insignificant difference.11 There was no significant (P=0.98) difference in anthropometric parameters between the groups in this study however in a study by Kotowycz et al older patients had transcatheter closure.In this study, pulmonary hypertension was present in 48% patients of surgical and in 33.3% patients of device. There was no significant (P=0.348) difference in pulmonary hypertension between the groups similar to the study by Kotowycz et al.12
The size of ASD was significantly (P=0.01) higher in surgical patients (24.6±9.8) compared to device patients (17.5±6.5) in the present study comparable to a study by Rudzitis et al where they found that ASD size in the device and surgical groups was 14.2 ± 5.6 mm and 28.7 ± 10.0 mm, respectively (p < 0.001). 13
Above findings strongly support the point that larger defects definitely require surgery. However, Vida et al. have reported that the transcatheter closure group had larger ASD than that of the surgical closure group. 14
In the present study, the duration of surgery was significantly (P=0.0001) higher in surgical patients (167.5±40.1 minutes) compared to device patients (65.3±28.0 minutes). In this study, the CPB/fluoroscopy time was significantly (P=0.0001) higher in surgical patients (60.5±23.6 minutes) compared to device patients (14.7±10.5 minutes). Aortic Cross clamp time and Mean minimum temperature was 32.1±15.0 minutes and 32.4±0.5 minutes respectively among surgical patients in the present study.
In a study by Berger F. and his co-workers, it has been reported that the complication rates are similar however the hospital stay is shorter with less morbidity in the device group.15Decreased cost is another added advantage of transcatheter ASD closure. In the present study, the length of hospital stay was significantly (P=0.001) higher in surgical patients (4.0±1.0 days) compared to device patients (3.0±0.6 days) comparable with the study by Ozdemir et al in which the surgical closure group had longer hospital stay (11.8 ± 3.8 days vs.2.8 ± 1.6 days, P < 0.001).11
In this study, the procedural success was in all surgical patients (100%) and in 93.3% of device patients. There was no significant (P=0.19) difference in procedural success between the groups. Ozdemir et al also found similar finding in which the procedural success rate was similar between the percutaneous closure and surgical closure groups (95% vs. 99%, P = 0.139). 11 Rudzitis et al compared results of transcatheter and surgical ASD closure in adults and found that there was no differences in procedure success rates: 99.2% in the device group and 100% in the surgical group (P=0.451). 13
No technique is a full proof success. Transcatheter device closure may fail due to many factors such as instability of the device. In these situations patient need to be taken up for surgical repair on an emergency basis. Sometimes the patients may require urgent intervention due to device embolization, cardiac perforation, erosion or rupture.13
The present study found that arrhythmia was in 16% of surgical patients and 20% of device patients. Transient cardiac arrhythmia was found to be the most common complication in device closure group in a study by Chen et al. 14Wound infection/ groin hematoma was seen in 12% surgical patients and in 13.3% patients of device closure. Device embolisation was in 6.7% patients of device group. Ozdemir et al found that device embolisation was observed in 1.4% patients.11
Conclusion[4]: In summary, both methods of device closure have their own benefits and limitations. Many studies have reported that transcatheter ASD closure is as effective as surgical ASD closure.16Transcatheter procedure is effective with a closure rate similar to that of surgery, the standard therapy. Furthermore, the complication rate is lower and the length of hospital stay is shorter for transcatheter patients compare to those of surgical patients. Surgery should be preferred in patients who reject foreign implants, have insufficient rims and associated with other congenital cardiac anomalies. Communication with the guardians is also of utmost importance. Individualized treatment options should be well discussed and the decision should be in the best of the patient. Appropriate patient selection is an important factor for successful ASD closure. All said and done surgery will always remain a final stopover.
A limitation of this study was the retrospective design and selection bias. We had to gather information from the medical record which were incomplete- Xray and electrocardiogram findings. Still extended follow ups are required to know about the long term benefits of the new interventional technology[5]
Ethics approval and consent to participate: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institution (IEC No 85/17) This article does not contain any studies with animals performed by any of the authors
Conflict of Interest: The authors declare that they have no conflict of interest.
Funding: Not applicable
Authors' contributions: Navneet Kumar Srivastva and Manoj Kumar contribute to draft the manuscript, Navneet Kumar Srivastava Subhash Rajput, Dharmendra Kumar Srivastava and Sudharshan Vijay revised it critically for important intellectual content and gave the final approval of the version to be submitted. All the authors reviewed and contributed the final version conflict of interest,:
Acknowledgment: Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors/editors/publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed."
References:
-
Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol.2002;39(12):1890-900.
-
Chelu RG, Horowitz M, Sucha D, Kardys I, Ingremeau D et al. Evaluation of atrial septal defects with 4D flow MRI-multilevel and inter-reader reproducibility for quantification of shunt severity. MAGMA. 2019;32(2):269-279.
-
Tsuda, T., Davies, R.R., Radtke, W. et al. Early Surgical Closure of Atrial Septal Defect Improves Clinical Status of Symptomatic Young Children with Underlying Pulmonary Abnormalities. Pediatr Cardiol. 2020; 41:1115–1124.
-
Siddiqui WT, Parveen S, Siddiqui MT, Amanullah MM. Clinical outcomes of surgically corrected atrial septal defects. J Pak Med Assoc. 2013;63(5):662-665.
-
Ak K, Aybek T, Wimmer-Greinecker G, Ozaslan F, Bakhtiary F, Moritz A, Dogan S. Evolution of surgical techniques for atrial septal defect repair in adults: a 10-year single-institution experience. J Thorac Cardiovasc Surg. 2007;134(3):757-764.
-
Naik MJ, Chua YL. Minimally invasive repair of atrial septal defects--a case series. Ann Acad Med Singap. 2000;29(6):735-749.
-
Vida VL, Tessari C, Fabozzi A, Padalino MA, et al The evolution of the right anterolateral thoracotomy technique for correction of atrial septal defects: cosmetic and functional results in prepubescent patients. Ann Thorac Surg. 2013;95(1):242–24
-
Grohmann, J., Höhn, R., Fleck, T., Schnoor, C. and Stiller, B. Transcatheter closure of atrial septal defects in children and adolescents: A single-center experience with the GORE® septal occluder. Cathet. Cardiovasc. Intervent. 2014;84: E51-E57.
-
Kim, Michael S, Andrew, John Carroll. Transcatheter closure of intracardiac defects in adults. Jof intervent cardiol. 2007;6:524-45.
-
Du, Zhong-Dong, Oi Ling, Jonathan Rhodes, Mary, Ziyad Choice of device size and results of transcatheter closure of atrial septal defect using the amp later septal occluder.J of interventcardiol. 2002;15(4 ): 287-92.
-
Özdemir E, Varis? E, Kiris? T, Emren SV, Nazli C, Tokaç M. In-Hospital cost comparison of transcatheter closure versus surgical closure of Secundum atrial septal defect. Int J Cardiovasc Acad. 2018;4:28-31.
-
KotowyczMark, Judith Therrien, Raluca, Colum, Louise Long-term outcomes after surgical versus transcatheter closure of atrial septal defects in adults.JACC. Cardiovascular interventions 2013; 6(5): 497-503..
-
Ooi YK, Kelleman M, Ehrlich A, Glanville M, Porter A, et al. Transcatheter Versus Surgical Closure of Atrial Septal Defects in Children: A Value Comparison. JACC Cardiovasc Interv. 2016; 119(1):79-86.
-
Chen, Q., Cao, H., Zhang, GC, Liang WC, Fan XU et al Midterm follow-up of transthoracic device closure of an atrial septal defect using the very large domestic occluder (44–48 mm), a single Chinese cardiac center experience. J Cardiothorac Surg. 2017;12, 74
-
Berger F, Vogel M, Alexi-Meskishvili V, Lange PE. Comparison of results and complications of surgical and Amplatzer device closure of atrial septal defects. J Thorac Cardiovasc Surg 1999;118:674-680.
-
DiBardino DJ, McElhinney DB, Kaza AK, Mayer JE Jr. Analysis of the US Food and Drug Administration Manufacturer and User Facility Device Experience database for adverse events involving Amplatzer septal occluder devices and comparison with the Society of Thoracic Surgery congenital cardiac surgery database. J Thorac Cardiovasc Surg. 2009;137(6):1334-1341.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License