IJCRR - 7(22), November, 2015
Pages: 52-56
Date of Publication: 21-Nov-2015
Print Article
Download XML Download PDF
STUDY ON ANALYSIS OF FUNCTIONAL OUTCOME OF FENESTRATION TECHNIQUE IN SINGLE LEVEL LUMBAR INTERVERTEBRAL DISC PROLAPSE
Author: Imran B.M., Pisudde P.M., Aravind Kumar
Category: Healthcare
Abstract:Objective: Aim of this study was to assess functional and neurological outcome by fenestration technique, since standard laminectomy and discectomy carries a risk of spine instability, it is preferable to perform discectomy through fenestration. Methods: Out of the 51 patients who were operated for single level lumbar disc herniation by fenestration discectomy between 2009 to April 2011, only 48 patients were available for follow up. Patients were followed up for a period of 1 year. The post operative outcome was analysed using the JOA score. The outcome was analysed with motor deficit, sensory deficit and bladder function as variables. Results: Back pain improved immediately in almost all 48(100%) patients. The outcome was excellent in 35.4%% patients good in 56.3% and fair in 8.3%. Conclusion: Fenestration technique with minimal disc removal is an effective technique for treating properly selected patients.
Keywords: Laminectomy, Discectomy, Herniation, Fenestration technique
Full Text:
INTRODUCTION
Disc prolapse is most common cause of the Low Backache. Disc prolapse commonly occurs in males with a male to female ratio of 2:1, highest prevalence is found to be in the age group of 30- 50 years.1 In India Prasad et al found that in their hospital 65.6% were male and 34.4% were female most common age of presentation was 31-40 years, they also found that disc prolapse is more common in moderate workers (59.4%) in rural India population2 . It is the responsibility of the orthopaedic surgeon to diagnose and treat this disease, since disc prolapse is the most common cause of low back pain. Disc prolapse is more common at the L4-L5 and L5-S1 levels followed by L3-L4 and L3-L2 levels.3 Lumbar discectomy is very commonly performed to treat disc prolapse if conservative management fails. Pain is the common indication to do fenestration, but neurological status is also to be taken inconsideration, other factors are far less of functional importance because they appear to be more of objective than pain related signs.4 Even with the advent of newer techniques like percutaneous endoscopic lumbar discectomy and use of Nd: YAG Laser, fenestration and microdiscectomy, technique still remains a good tool for treating patients of Low back pain with disc related pain.5,6Fenestration though relieves pain in almost all patients, it is important to select the patients carefully to get a good result. Fenestration is less time consuming, with lower blood loss and lesser postoperative complications and maintains the stability of the spine better than procedures like laminectomy and discectomy.3, 7 To assess objectively, the results of lumbar disc surgery, there are no specific criteria. Interestingly, the results of lumbar disc disease present a challenge to surgeons. Dissimilarity among the population undergoing surgery compared the problems of wide variability in analyzing results. This subjective and objective obser vation and purposed implication from data assembled tends to confuse rather than illuminate. Clearly there is a need for simple systematic protocol for analyzing results of lumbar disc disease. There are very few literatures which emphasize on improvement about the various parameters after different disc surgery and also fenestration surgery. So the present study was undertaken to analyze the improvement of various parameters after fenestration for example gait, activities of daily living etc. Aim of this study was to access functional and neurological outcome by fenestration technique, since standard laminectomy and discectomy carries a risk of spine instability, it is preferable to perform discectomy through fenestration.
MATERIALS AND METHODS
Present cross sectional study which was prospective in nature was carried out between the period of February 2011 to April 2013. Patients visiting to orthopaedics Out Patient Department(OPD) in hospital were included in study. A detailed history and thorough clinical examination was done in all patients. Magnetic Resonance Imaging(MRI) was done followed by routine pre op investigations. All details were recorded in a proforma. The study subjects having Single level disc disease, low back pain and radicular pain, sensory, motor deficit and bladder symptoms were included in study. Study subjects showing significant evidence of disc prolapse in MRI were carefully selected and included in study. Study subjects those who were excluded were those who underwent surgical treatment for disc prolapse, suffering from other associated disease of spine, not undergone conservative management and suffering from only back pain and no associated signs or symptoms. Pre op and post op assessment was done using the Japanese Orthopaedic Association scoring (JOA score)system.8 For uniformity all surgeries were done by single surgeon, all patients underwent fenestration and intra-op complications were noted. Follow up was done at 14 days, 1 month, 3 months and 6 months and 1 year was done. Neurological status and signs for radicular pain and LBA were checked.Operative technique of fenestration: Patient is positioned in the prone knee-chest position, care being taken to see the abdomen is free so as to prevent undue engorgement of the epidural veins and thus decrease the extent of intra operative blood loss. A vertical mid-line incision is made after localizing the level of the disc. The para-spinal muscles are retracted and the interlaminar space is exposed. Only the ligementum flavum is excised removing only small part of the lamina. The thecal sac is retracted the disc herniation identified and discectomy carried out using disc removing forceps. The disc at that level is removed partially. The thecal sac and the roots are confirmed to be decompressed and lying freely in their respective canals. The wound is closed in layers and dressing done. After treatment: IV Antibiotics were given routinely for 2 days; the suction drain was removed within 48 hrs and the patient was mobilized with a lumbo sacral corsette on the second post operative day. Suture removal done on 10th post operative day. Patient was explained the different methods of taking care of the back and advised against doing any strenous activity for the first six weeks after which patient was gradually encouraged to get back to his previous level of activity. It is proved that limited disc excision is sufficient, rather than entire disc removal which can cause collapse of disc space and degeneration of apophyseal joints at a later date. 9, 10,11
RESULTS
A total number of 53 patients were selected for fenestration and operated during the period of February 2011 to April 2013. 48 patients were available for follow up of one year. Most of them had central paracentral PIVD more commonly and less commonly lateral and far lateral PIVD. Distribution of the study subjects were as follows mentioned in table 1
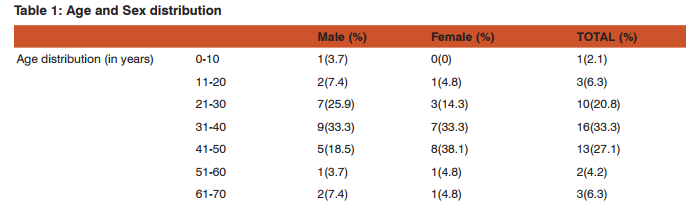
Above table 1 shows that majority of study subjects were males (56.3%) and female (43.7%). Table also shows that males were more in age group of 31-40 years and females were more in 41-50 years. Majority of the study subject were indulge in doing light work 56.3% followed by 43.8% performing heavy work. Majority of study subject had gradual onset of the symptoms ie 89.6% and only 10.4% had sudden onset of symptoms.75% of study subjects witnessed dull aching pain followed by catching pain in 22.9% study subject and 2.1% witnessed severe type of pain.
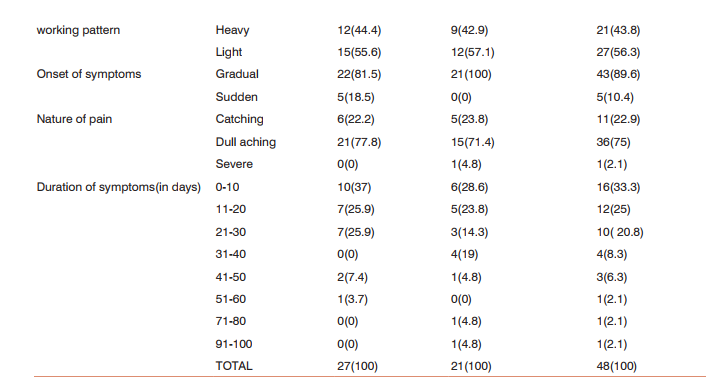
Above table 2 shows that there is improvement in all the parameters after fenestration operation majorly in low back pain with 66.7%, motor disturbances (65), followed by leg pain (63.3), and followed by gait (60%). Activity of daily living improved by 43.6% followed by SLR (passive)
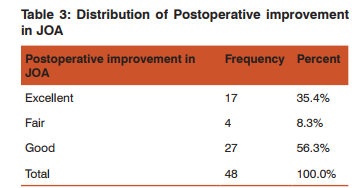
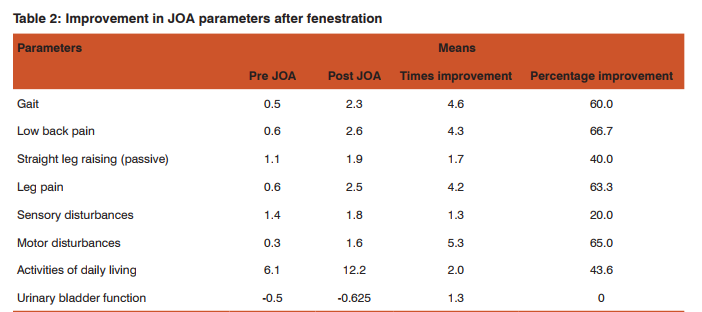
Above table 3 shows that maximum study subjects had good JOA score falling in the good outcome with 56.3%, followed by 35.4% having excellent outcome and only 4% were having 8.3% outcome
DISCUSSION
Lumbar laminectomy is the most common operation for a herniated lumbar disc. But laminectomy has its inherent draw backs of a prolonged surgical time, more blood loss and a delayed convalescence period as compared to fenestration7. The post-operative complication (e.g., Arachnoiditis and adhesions) are found to be more when laminectomy is used as a procedure. To add this it is also found to Jeopardize the mechanical stability of the Spine.7 In such a situation a surgical procedure which is less damaging to the stability of the spine, has a shorter surgical time, less blood loss, lesser incidence of post-operative complications and ultimately has a shorter convalescence period would be more beneficial. Excision of a herniated disc for relief of sciatica provides rapid relief of sciatica and low back pain.12 The best result is achieved if the patient was operated on before two months of onset of symptoms of disabling sciatica.13In the younger patients it is important to aim toward an early return to duty via surgical treatment.14 Discectomy by fenestration method is kind of a surgical procedure wherein only the inter laminar space is utilized with removal of minimal part of the superior lamina, the cord is exposed, retracted and the discectomy carried out. The present study analysis the results of this surgical technique on the basis of the functional outcome of the patient, it shows an improvement in activities of daily living, gait, back pain, leg pain, sensory, motor and bowel bladder symptoms. The change in improvement in all above parameters and outcome after surgery indicate JOA to be a useful tool in evaluation. Present study stated that there is near about 50% improvement in the patient’s condition when JOA Score was taken into consideration, and in some parameters there were upto 65% improvements. Other studies stated that there was not more significant difference in the surgical procedure used, and they found fenestration was complicated process and not much useful. Similar results were found with the fenestration surgery which was equivalent to the results of study done by Sharma et al.15 In the present study similar type of prognostic factors were used and the results were also similar with studies of Smith M et al and Spangfort et al study which showed that lumbosacral discectomy appear favorable as evaluated in this study. Preoperative factors useful as predictors of short-term outcome are much less reliable when considering the longterm results. These factors were number of previous hospitalization, duration of leg pain, straight leg-raise examination, and presence of osteophytes, disc bulge, and duration of surgery. 9,16, In the present study duration of symptoms in study subjects was associated with surgical outcome of fenestration technique similar was found in other studies.17In the present study it was found that the clinical outcome was better after the fenestration surgery similar was found in study conducted in Rohtak.3
CONCLUSION
Form the following study it can be concluded that Interlaminar technique of fenestration is a safe and reliable method for treating patients of lumbar disc prolapse which shows improvement in all the aspects of the criteria which was taken into consideration in JOA score, but patients has to be closely scrutinized for surgery. The outcome was excellent in 35.4%% patients good in 56.3% and fair in 8.3% this satisfactory outcome is only because of carefully selecting patients. Change in the outcome score preoperatively compared to post operative shows that JOA score is a useful tool for evaluation of fenestration technique. Good neurological recovery has been noted following fenestration.
ACKNOWLEDGEMENT
Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
1. F. Postacchini, G.cinnotti, lubar disc herniation, Etiopathogenesis inFranco postacchini in Lumbar disc herniation, Thompson press, newDelhi, springerwein 1999: 151-152.
2. R.Prasad, M.F. Hoda, M.M. Dhakal, K. Singh, et al: Epidemiological Characteristics of Lumbar Disc Prolapse in a Tertiary Care Hospital. The Internet Journal of Neurosurgery. 2006 Volume 3 Number 1.
3. SS Sangwan, ZS Kundu, Raj Singh, P Kamboj, RC Siwach, et al:Lumbar disc excision through fenestration, Indian journal ofOrthopaedics, [2006], 40[2]:86-9.
4. Bo Johnson 1996 “Neurological signs of lumbar disc herniations” acta Otho scand 67[5]:466-69.
5. Sasani M, Ozer AF, Oktenoglu T, Canbulat N, Sarioglu AC. Percutaneous endoscopic discectomy for far lateral lumbar disc. Herniations, Minim Invasive Neurosurg. 2007 Apr; 50[2]:91-7.
6. Savitz MH, Doughty H, Burns P. Percutaneous lumbar discectomy with a working endoscope and laser assistance. Neurosurg Focus.Cited 1998 Feb 15; 4[2]:e9.Available from: http://www. ncbi.nlm.nih.Gov/pubmed/17206772.
7. Nagi, O.M. ‘Early results of discectomy by Fenestration technique’ Indian Journal of Orthopaedics, 1985;19[1]: 15-9
8. Japanese Orthopaedic Association (JOA). Japanese Orthopaedic Association Assessment Criteria Guidelines Manual. 1996. p-46-9.
9. Spangfort EV. The Lumbar disc herniation – a computer aided analysis of 2504 operation. Acta Orthop. Scand suppl 142:3-95, 1972.
10. Astrand, 2000 “Pain and orthopaedic and neurologic signs after lumbar discectomy”. Clinical Orthopaedics and related reserch, 379: 154–160.
11. Loupasis, George A, Stamos, Konstadinos, Katonis, et.al Sevento 20-Year Outcome of Lumbar Discectomy, Spine, 1999 November, 24[22]:2313.
12. Toyone, T., Tanaka, T., Kato, D. and Kaneyama, R. Low-back pain Following surgery for lumbar disc herniation. A prospective study. J.Bone Joint Surg (Am). 2004; 5: 86-A (5): 893-896.
13. Deyo, R. A. Non-operative treatment of low back disorders: differentiating useful from useless therapy. In: Frymoyer J.W., editor. The adult spine: principles and practice. New York: Raven Press. 1991; 1559–1560.
14. Ishihara, H., Matsui, H., Hirano, N. and Tsuji, H. Lumbar intervertebral disc herniation in children less than
16 years of age. Long-term follow-up study of surgically managed cases. Spine. 1997; 22 (17): 2044-2049.
15. Sharma, 1980 “A clinical profile of prolapsed intervertebral disc and Its management”. Indian Journal of Orthopaedics, 14(2): 204–212. 16. Smith M, Gallagher J, Memanus F. Surgery in lumbar disc protrusion. A long term follows up. In Med J 76:25-26, 1983.
17. D. Olsen, D. McCord and M. Law. Laparoscopic discectomy with Anterior interbody fusion of L5-S1, surgical endoscopy, 1996. December; 10[12]:1158-63.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License