Welcome to IJCRR
Indexed and Abstracted in: Crossref, CAS Abstracts, Publons, Google Scholar, Open J-Gate, ROAD, Indian Citation Index (ICI), ResearchGATE, Ulrich's Periodicals Directory, WorldCat (World's largest network of library content and services)
|
The test result variable(s): ALP has at least one tie between the positive actual state group and the negative actual state group. Statistics may be biased. |
|
a. Under the nonparametric assumptionNull hypothesis: true area = 0.5 |
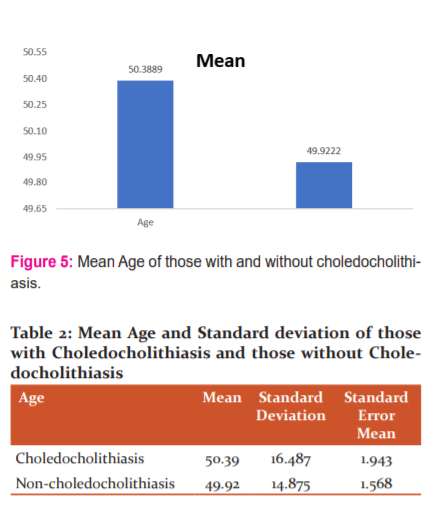
The mean age of those with choledocholithiasis was found to be 50.39 with SD ± 16.487. The mean age of those without choledocholithiasis was 49.92 with SD ± 14.875 (Figure 5 and Table 2). The Chi-square test performed revealed no significant relation with age.
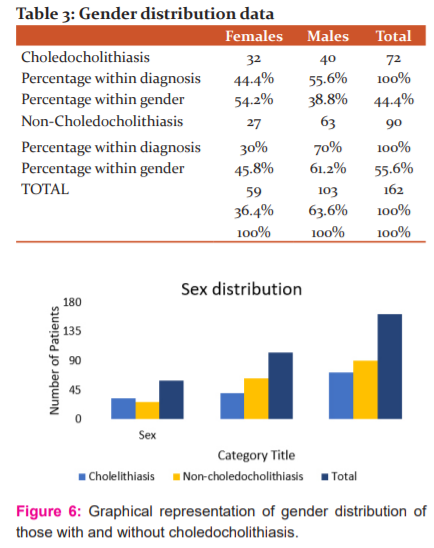
Gender distribution was as follows: The total number of females were 59 and males were 103. Amongst the 59 women, 32(54.7%) had choledocholithiasis and among the males, 40(38.8%) had choledocholithiasis (Table 3 and Figure 6).
Of the total 162 patients, 72 had choledocholithiasis. Out of the 72, 51 patients had raised ALP beyond 130 IU/L and 21 patients (30%) had a normal ALP value (<130IU/L). The sensitivity of ALP was calculated as 70.8% and Specificity was 55.7%. A Positive predictive value of 56.7% and a negative predictive value of 70% was observed. The percentage of false positives was 44.3% whereas the percentage of false negatives was 29.2% (Table 4).
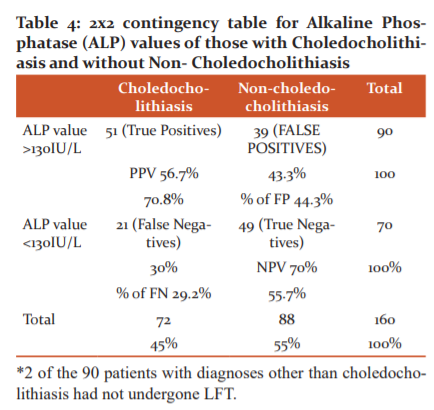
30% (21) of all patients with choledocholithiasis showed a normal ALP – a significant number of patients in whom the diagnosis can be missed if relying only on ALP to show evidence of biliary obstruction. Of the 21, 12 were male and 9 were female. The mean age was found to be 53.619. Concurrent Cholelithiasis was present in 13 of the cases. 4 had features of calculous cholecystitis. Adenomyomatosis of the gall bladder was present in 2 patients. Concurrent pancreatic calculus was present in 1 patient. An anatomical variant of the biliary tree with hepatomegaly was observed in 1 case. 2 cases showed MRI features of acute pancreatitis. Serum amylase was elevated more than 80u/l in 7 patients whereas 6 out of 21 had lipase elevated more than 60u/l. CBD and CHD Diameter was measured and matched with age-appropriate standard diameters as “Decade of age +1”. CBD was dilated in 17 out of the 21 patients. Total bilirubin was elevated as >1.20mg/dl in 9 out of 21. Clinically evident jaundice (>3mg/dl) was present only in 1 patient. SGOT and SGPT (normal <50u/l) were elevated only in 4 out of 21 patients. All 21 of them underwent ERCP with common bile duct stenting.
Discussion:
Liver function tests are the preliminary serum markers done in all patients with suspected hepato-biliary pathologies. Alkaline phosphatase is thought to be specific for ductal pathologies as one of its main sources is the cells lining the biliary canaliculi. Although Gamma-glutamyl transpeptidase and 5’nucleotidase are also specific for cholestasis. Our study focussed only on routine LFT parameters as GGT is not routinely done. The observed pattern in obstruction is increased in serum bilirubin, alkaline phosphatase and elevated ALT, AST with a cholestatic pattern.
Anciaux et al.2 demonstrated that serum ALP and γ-GT were elevated within the 1st 3 days in 100% of patients with biliary obstruction, whereas aminotransferase levels were elevated in up to 88% of patients, with a mean of 102 to 150 IU/L for AST and ALT;
“In our experience, the absence of any biological abnormality during the three days following the onset of symptoms made the diagnosis of choledocholithiasis quite improbable.”
In a study carried out by H C van Santvoort et al.3, to determine which radiological or serological parameters best predicted CBD stones, they reported that “raised ALP (OR: 3.16, p=0.006) on admission blood tests was a superior indicator to ALT (OR: 2.30, p=0.187) and bilirubin (OR: 0.89, p=0.637) for CBD stones although all had low sensitivity”; “In univariate analysis, the only parameters significantly associated with CBD stones were GGT and alkaline phosphatase.”
The positive predictive value of elevated liver tests is poor because deranged liver function can indicate a variety of other pathologies as well. Hence it was understood so far that, normal levels help in excluding choledocholithiasis. The need for further imaging is assessed based on clinical progression, which subjectively varies from each patient to the other and biochemical indicators of cholestasis such as raised bilirubin, ALP or GGT.
In our study, 21 out of 72 patients with MRCP detected choledocholithiasis had a normal alkaline phosphatase. This accounts for 30% of patients who would have had a missed diagnosis is reliant on the above criteria. The percentage of false negatives was 29.2% with a positive predictive value of 56.7% and a negative predictive value of 70%. Our study highlights the percentage of patients who would be left with a missed diagnosis in the event of the use of selective MRCP based on ALP as the predictive parameter. The consequences of a missed diagnosis are wide-ranging such as the conversion of laparoscopic procedure to open, the need for further post-operative re-intervention such as ERCP or second surgery, postcholecystectomy syndrome, increased morbidity, prolonged hospital stay and increased financial burden.
Hence, it is imperative to identify the presence or absence of common bile duct stones as it dictates the line of management for the surgeon. Common bile duct stones can be easily missed on routine ultrasonography.4,8 and hence require further imaging studies. This depends on the choice of the surgeon: some prefer MRCP, others utilise EUS and some go ahead with an intra-operative cholangiogram. ERCP has been the preferred modality as it can be therapeutic as well as diagnostic of choledocholithiasis for many decades; although MRCP is non-invasive, whereas EUS is less invasive than ERCP.5,6 The choice of investigation and further management is dictated by the individual clinical settings. The availability of endoscopic services, feasibility, and cost-effectiveness also determine the role of ERCP and EUS.
EUS is thought to be the choice to identify biliary sludge, smaller stones (<6mm) and in those with a nondilated common bile duct and it is an option for patients for whom MRCP is contraindicated (e.g. pacemaker, claustrophobia, gadolinium allergy).7,8 However, the limiting factors may be the lack of availability of endoscopic services, skilled endoscopists and operator dependency producing subjective results.
MRCP, although non-invasive, has not been standardised as the investigation of choice due to high cost, reliability on patient co-operation for optimal results. We are trying to highlight the need for standardised use of MRCP as the diagnostic modality for all patients of clinically suspected choledocholithiasis to reduce the consequences of a missed diagnosis.
Conclusion:
Alkaline phosphatase, a biochemical indicator of cholestasis, is poorly reliable in predicting common bile duct pathologies. According to our results, the sensitivity (70.8%) and specificity are both low (55.7%) with the area under the Receiver Operating Curve was plotted with ALP levels of all patients as 0.641 (<0.70- insignificant). A normal Alkaline Phosphatase value in a patient with suspected choledocholithiasis does not rule out the presence of a common bile duct stone.
The lack of non-universal practice of biliary ductal imaging modalities highlights the increased likelihood of missed diagnosis and morbid complications. All patients with suspected CBD stones should be subjected to a pre-operative MRCP to identify the presence of CBD stones. Alkaline phosphatase should not be the sole biochemical indicator to dictate the selective use of MRCP.
Declarations:
Ethics approval: Sri Ramachandra Institute of Higher Education and Research, Institutional Ethics Committee Clearance: REF: CSP-MED/20/0CT/62/114
Consent for Publication: Not applicable
Competing Interests: The authors declare that they have no competing interests.
Availability of data and materials: References provided, not applicable otherwise.
Funding: Not applicable
Author’s contributions:
DS was responsible for data collection. KBS was in charge of reviewing the manuscript. TM conceived the idea of the study and reviewed the manuscript.TM and NN were responsible for multiple revisions of the drafted manuscripts.
All authors have approved the final submitted version and have agreed with both to be personally accountable for the author's contributions and to ensure that questions related to the accuracy or integrity of any part of the work, are appropriately investigated, resolved, and the resolution documented in the literature.
The manuscript is in concordance with STARD 2015 Guidelines.
Acknowledgements:
Department of General Surgery,
Sri Ramachandra Institute of Higher Education and Research, Chennai – 600116
Department of Medical Gastroenterology,
Sri Ramachandra Institute of Higher Education and Research, Chennai – 600116
Department of Radiology and Imaging Sciences,
Sri Ramachandra Institute of Higher Education and Research, Chennai – 600116
Abbreviations
ALP- Alkaline phosphatase
ALT – Alanine amino-transferase
AST- Aspartate amino-transferase
CBD- Common Bile duct
CHD- Common hepatic duct
ERCP- Endoscopic retrograde cholangio-pancreatogram
MRCP – Magnetic resonance cholangiopancreatogram
NPV- Negative predictive value
PPV- Positive predictive value
ROC- Receiver operating characteristic curve
References:
1. Barlow AD, Haqq J, McCormack D, Metcalfe MS, Dennison AR, Garcea G. The role of magnetic resonance cholangiopancreatography in the management of acute gallstone pancreatitis. Ann R Coll Surg Engl. 2013 Oct;95(7):503–6.
2. Anciaux ML, Pelletier G, Attali P, Meduri B, Liguory C, Etienne JP. Prospective study of clinical and biochemical features of symptomatic choledocholithiasis. Dig Dis Sci. 1986 May 1;31(5):449–53.
3. Van Santvoort HC, Bakker OJ, Besselink MG, Bollen TL, Fischer K, Nieuwenhuijs VB, et al. Prediction of common bile duct stones in the earliest stages of acute biliary pancreatitis. Endoscopy. 2011 Jan;43(1):8–13.
4. Qiu Y, Yang Z, Li Z, Zhang W, Xue D. Is preoperative MRCP necessary for patients with gallstones? An analysis of the factors related to the missed diagnosis of choledocholithiasis by preoperative ultrasound. BMC Gastroenterol. 2015 Nov 14;15:158.
5. Isherwood J, Garcea G, Williams R, Metcalfe M, Dennison AR. Serology and ultrasound for the diagnosis of choledocholithiasis. Ann R Coll Surg Engl. 2014 Apr;96(3):224–8.
6. Zare M, Kargar S, Akhondi M, Mirshamsi MH. Role of liver function enzymes in the diagnosis of choledocholithiasis in biliary colic patients. Acta Med Iran. 2011;49(10):663–6.
7. Zidi S, Prat F, Le Guen O, Rondeau Y, Rocher L, Fritsch J, et al. Use of magnetic resonance cholangiography in the diagnosis of choledocholithiasis: prospective comparison with a reference imaging method. Gut. 1999 Jan;44(1):118–22.
8. Karakan T, Cindoruk M, Alagozlu H, Ergun M, Dumlu S, Unal S. EUS versus endoscopic retrograde cholangiography for patients with intermediate probability of bile duct stones: a prospective randomized trial. Gastrointest Endosc. 2009 Feb 1;69(2):244–52.
Indexed and Abstracted in






Antiplagiarism Policy: IJCRR strongly condemn and discourage practice of plagiarism. All received manuscripts have to pass through "Plagiarism Detection Software" test before forwarding for peer review. We consider "Plagiarism is a crime"
IJCRR Code of Conduct: To achieve a high standard of publication, we adopt Good Publishing Practices (updated in 2022) which are inspired by guidelines provided by Committee on Publication Ethics (COPE), Open Access Scholarly Publishers Association (OASPA) and International Committee of Medical Journal Editors (ICMJE)
Disclaimer: International Journal of Current Research and Review (IJCRR) provides platform for researchers to publish and discuss their original research and review work. IJCRR can not be held responsible for views, opinions and written statements of researchers published in this journal.
International Journal of Current Research and Review (IJCRR) provides platform for researchers to publish and discuss their original research and review work. IJCRR can not be held responsible for views, opinions and written statements of researchers published in this journal
148, IMSR Building, Ayurvedic Layout,
Near NIT Complex, Sakkardara,
Nagpur-24, Maharashtra State, India
editor@ijcrr.com
editor.ijcrr@gmail.com
 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
Copyright © 2026 IJCRR. Specialized online journals by ubijournal