INTRODUCTION
Natural products are a significant source of synthetic and traditional herbal medicine and are the primary source of the health care system. The traditional medicinal methods, especially the utilization of medicinal plants play a vital role in covering the basic health requirements in developing countries.1 Plants have been utilized in form of medicines since immemorial time. In Europe, henna was popular among females connected to the aesthetic movement and the Pre-Raphaelite artists of England in the 1800s. Henna is known as an essential ancient dye, evidence being the Egyptian mummies found in the tombs that had their nails dyed with henna. Consequently, the relics from the excavation at Mohanjodaro and Harappa (Indus Valley Civilization), Ajanta Caves Painting and Mughal dyeing, printing, and painting, show the use of natural dyes such as Madder, Indigo, and Henna. Henna leaves have been extensively utilized.
India has rich heritage of utilizing medicinal plants in traditional medicines such as Ayurveda, Siddha, and Unani besides folklore practices.2 A diverse range of plants may be incorporated in herbal preparations, and many of them can have serious toxic side effects. The utilization of Ephedra has documented or its effect on cardiovascular health, including death, which’s why prohibited to sale in the United States. Some herbal preparations cause dangerous drug interactions, primarily by altering the expression of liver enzymes. Alternative medicines and supplements have also been linked with hepatotoxicity, nephrotoxicity, neurotoxicity, carcinogenicity, and allergic reaction.3 Herbal drugs or medicinal plants, their extracts, and their isolated compound have demonstrated a spectrum of biological activities.4
Similarly, Lawsonia inermis linn. is a well-known plant usually grown in houses.5 Lawsonia inermis Linn. is commonly known as henna, which is recognized in the traditional system of medicine.6 As a cosmetic for staining hands, palms, hairs, and other body parts during religious festivals and marriages, and so on.7 Henna has been utilized as a cosmetic hair dye for 6,000 years.8 The plant of Lawsonia Inermis linn is shown below in figure no.1,
LAWSONIA INERMIS LINN
Lawsonia inermis Linn. (Lythraceae), henna is a biennial dicotyledonous herbaceous shrub.5,6 Lawsonia inermis Linn. is a perennial plant that belongs to Lythraceae, also known as the loosestrife family.7,8 It is also known as Alcanna spinosa, Casearia multiflora, Lawsonia alba, Lawsonia speciosa, Lawsonia spinosa, Lawsonia, and Rotantha combretoides. It has its local names e.g. Arabic: henna; Bengali: mendi, mehedi; English: Camphire, Egyptian-privet, henna, Jamaica-mignonette, mignonette-tree; French: henné; German: Hennastrauch; Hindi: mehndi; Sanskrit: Mendika, Telugu: Goranti, Malayalam: Mailanchi, Indonesian: inai, pakar kuku; Portuguese: hésia, hena, alfeneiro; Spanish: alcana, alheña; Swedish: henna; Vietnamese: nhuôm móng taylâ mòn.9,10,11
PRODUCTION OF LAWSONIA INERMIS LINN
Henna requires less water than traditional crops and is sustainable for agriculture in semi-arid regions.12 Lawsonia inermis frequently cultivated in India, Persia, and along the African coast of the Mediterranean Sea, widely cultivated as an ornamental hedge and dye plant.13,14 It was distributed in Africa: Egypt, Ethiopia, Somalia, Sudan, Zaire, Niger, Benin, Burkina Faso, Cote D'Ivoire, Gambia, Ghana, Guinea, Guinea-Bissau, Liberia, Mali, Nigeria, Senegal, Sierra Leone, Togo, South Africa, Comoros, Seychelles; Asia: India, Pakistan, Sri Lanka. It is widely cultivated in tropical regions of the world, the Southern areas of the Middle East, the Arabian Peninsula, North, and East Africa, and South Asia.
CHEMICAL CONSTITUENTS
-
Leaves: 2-Hydroxy-1,4-napthoquinone, 1,4dihydroxynaphthalene, 1,4-naphthoquinone, 1,2-dihydroxy-glucoyloxynaphthalene, luteolins, apigenin, and their glycosides, esculetin, fraxetin, scopletin, β-sitosterol, tannin, gallic acid, glucose, mannitol, fat, resin and mucilage.
-
Barks napthoquinone, isoplumbagin, triterpenoids-Hennadiol, aliphatics (3-methylnonacosan-1-ol)
-
Flowers essential oil (0.02 %) rich in ionones (90 %), β-ionones.
-
Roots 24β-ethylcholest-4-en-3β-ol
-
Seeds Linoleic acid, Arachidic acid, Stearic acid, Palmitic acid
-
Whole plant Laxanthone I, Laxanthone II, Laxanthone III, n-Triacontanol.15-18 The henna plant is shown below in figure no.2;
A new sterol, namely lawsaritol has been isolated from the roots of Lawsonia inermis. Its structure has been elucidated as 24β-ethylcholest-4-en-3β-ol based on spectral analysis and chemical reaction.20,21
These compounds exhibit in form of antimicrobial, anti-sickling, macrophage-stimulating, hepatoprotective, Analgesic, Anti-inflammatory, antipyretic, anticomplementary, cytotoxic, antioxidant, protein glycation inhibitory, Antituberculostatic, Antidiabetic, Antiulcer, Antiarthritic, Memory enhancing, Antiurolithiatic, Nematicidal effect, Antiparacidal, Antitrypanosomal, Molluscicidal, Antifertility, Ovicidal, Antidermatophytic activity, Anticonvulsant, Antisickling, and immunomodulatory property.22
CLASSIFICATION
There are three different types of henna, Neutral henna, Red henna, and Black henna.
-
Neutral henna: A green powder that scents similar to freshly cut grass cannot be henna /neutral. It is identified as Cassia obovata, contains anthraquinones, specifically chrysophanic acid, an identified antifungal, antimicrobial, and antibacterial compound. Cassia obovata does not color hair.
-
Red henna, a green powder that scents like hay, is Lawsonia inermis, commonly named henna. Henna will stain hair red-orange, but this stain is translucent and will combine with natural colour. The leaves of the henna plant have a red-orange dye molecule that is Lawsone, a naphthoquinone compound.19-22
-
Black henna: A green powder that scents like frozen peas, is neither henna nor black. It is indigo, Indigofera tinctorial.23
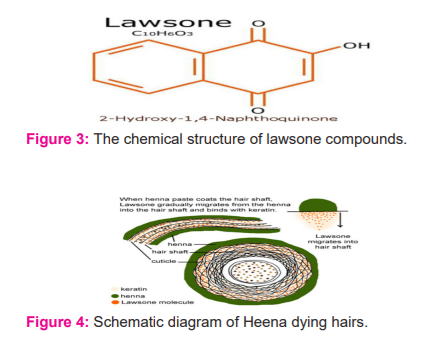
Lawsonia inermis Linn contains a red-orange pigment known as Lawsone, the molecule of which is also called hennotannic acid.24 Lawsone is the main constituent responsible for the dying properties of the plant.25 When henna leaves are smushed in an acidic medium and applied to the skin, the lawsone molecules migrate from the henna paste, the cuticle, traverse the outermost layer of the hair, and stain the hair. Prolonged applications of henna result in diffusion of the pigment deeply into the hair,26 a burgundy organic compound that has an affinity for bonding with protein.30 The dried and powdered leaves are mixed with warm water to form a mud-like paste, which is placed on the hair for 30–40 min to dye it. The colouring action is due to, which is naturally present as a glucoside and as the aglycone in the plant leaves.27 The chemical structure of lawsone compounds and schematic diagram of Heena dying hairs are given below in figure no.3 & figure no.4;
SIDE-EFFECTS OF RED HENNA
Contact allergy
Red henna is generally considered safe. Yet a few reports of contact allergic reactions, despite its extensive use exits. For instance, it has been assessed that at least half of the population of India has been presented to henna at some time in life, so it can be assumed that its sensitizing potential must be negligible. It is typically expected that the allergen in henna is Lawsone. However, this compound has been tested in only a few studies. In this manner, in most cases, the actual allergen stayed unknown, and some cases of contact allergy may have been caused by other ingredients of the plant or substances included later, for instance, essential oils.
Immediate reactions
Immediate-type hypersensitivity to henna has been reported rarely. It is an occupational hazard for hairdressers in the form of presumably IgE-mediated reactions, with symptoms like running nose sneezing, conjunctivitis, dry cough, dyspnoea, swelling of the face, or generalized urticaria. The main event for sensitization is the inhalation of a henna powder dispersed in the air.
MISCELLANEOUS SIDE-EFFECTS
Extravagant floral henna tattoo patterns on both forearms and hands may cause issues with peripheral venous cannulation—a metabolite of naphthalene and a powerful oxidant of G6PD –deficient cells. The topical application of henna may, therefore, cause life-threatening haemolysis in children with glucose-6-phosphate dehydrogenase deficiency. Signs and symptoms may include pallor, vomiting, jaundice, anaemia, lethargy, tachycardia, poor peripheral perfusion, shock, and even death.
PPD (PARA-PHENYLENEDIAMINE)
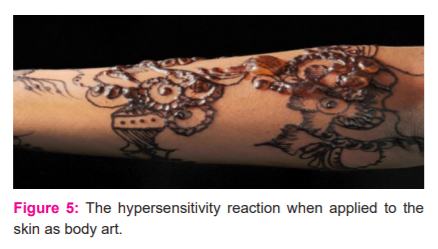
The hypersensitivity reaction to PPD sold as ‘black henna’ and applied to the skin as body art is given in figure no. 5. The above image of a woman’s arm blistering from an application of ‘black henna,’ a paste with little or no henna, but a high content of para-phenylenediamine. ‘Black Heena’ temporary tattoos are created with a paste containing 12.5% to 80% PPD. Para-phenylenediamine has been conflated with henna as ‘black henna’ since the 1970s and has popularized around the world for celebratory and festival skin adornment. Estimated that 150,000,000 individuals had been sensitized to PPD, and a much larger number had been sensitized through cultural use. A sensitization test in Manchester, UK, found the sensitization rate among children had risen from 3% in the 1990s to 8% in 2005 to 16% in 2014.
It was reported that allergic reactions are mostly caused by some ingredients added by the so-called “artists.” The ingredients are generally colouring agents such as diaminotoluenes and diaminobenzenes. Para-phenylenediamine (PPD) is a typical diaminobenzene and is one of the most popular ingredients. The allergic reactions caused by PPD include acute inflammatory reactions, eczematous hypersensitivity reactions, photo aggravated reactions, granulomatous reactions, lichenoid reactions, and pseudolymphomatous reactions. It was accounted that the long duration of skin contact, the high concentrations of sensitizing materials, and the absence of a neutralizing agent dramatically increases the risk of skin sensitization. Therefore, the Food and Drug Administration (FDA) approves henna only for use as a hair dye, not for direct application to the skin. The unapproved use of a color additive makes these products adulterated and, therefore, illegal.
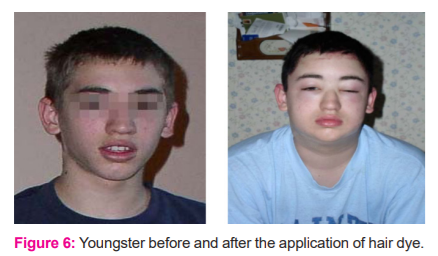
Therefore, It can be assumed that natural henna is a feeble skin allergen. PPD (p-phenylenediamine) is an aromatic amine compound; its chemical formula is C6H8N2, and its molecular weight is 108.15 g/mol. It can be easily observed in figure number 6 of a youngster before and after the application of hair dye.
It is a white to light purple powder that darkens on exposure to air. It is primarily utilized as an element of oxidative hair colouring products at a maximal concentration of 4.0%; still, after mixing in a 1:1 ratio with hydrogen peroxide before use, this concentration will be 2% at the time of application to the hair. It oxidizes, turning first red, then browns, then finally black.
Black henna contains p-phenylenediamine (PPD), an aromatic amine that reacts with components containing at least one aromatic ring in their structures. A black and long-lasting stain is created in minutes, rather than hours, when PPD mixed with henna is applied in decorative patterns to the skin. The utilization of PPD is the leading cause of allergic contact dermatitis or severe allergic reactions from henna tattoo mixtures. Allergic reactions may present as itching, blistering, depigmented skin patches, and even permanent scarring, which are treated with antibiotics and corticosteroids.
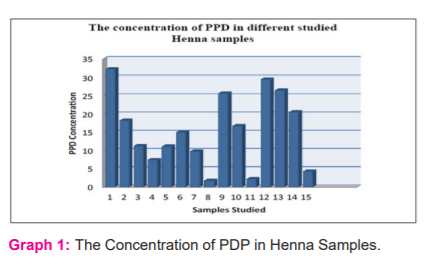
Notwithstanding hair dyes, PPD may also be found in fur or textile dyes. para-Phenylenediamine is also utilized as a developing photographic agent as well as an antioxidant in rubber compounds. People may be occupationally exposed to PPD during its manufacture or use, and the exposure may occur through inhalation, skin or eye contact, and ingestion. Short-term exposure to high levels of PPD may cause extreme dermatitis, eye irritation and tear, gastritis, asthma, tremors, renal failure, vertigo, convulsions, and coma in humans. The Concentration of PDP in Henna Samples are given below in graph number 1;
Apart from the use of PPD, many other chemicals, including p-methylaminophenol, p-aminobenzene, p-toluene diamine, benzene, petrol, butane, hydroquinoneandisobutyl p-aminobenzoate are added to natural henna and have been associated with contact dermatitis38&41.
COMPLICATIONS OF HENNA
Although most of the complications of henna come from topical applications for traditional events or temporary tattoo. Somewhere, other complications have occurred after the oral ingestion of henna e.g. Allergic contact dermatitis, Immediate-type hypersensitivity with urticarial, Erythema multiforme, Post-inflammatory hypo-or hyperpigmentation, Hypertrichosis Keloids, Hemolysis, Vasculitis and renal impairment, Teratogenicity etc.27-30
Most pregnant women believe that natural treatments are not dangerous and do not have any side effects for either the mother or the fetus, and due to such questionable beliefs may attempt to self-medicate with herbal medicines or other such preparations. The potential effects of Lawsonia inermis extract on the gestation of mice embryos in pregnant mice. The results indicated that the use of Lawsonia inermis during pregnancy might cause abortion, and therefore, the researchers of the study highly suggest that Lawsonia should be utilized with great caution or else considered to be counter-indicated for pregnant individuals.
HENNA AND G6PD DEFICIENCY
People along with homozygous G6PD deficiency are called Favism. Who is suggested not to use henna to dye their hairs? It is a genetically inherited anomaly on the X chromosome and henna can cause hemolytic anaemia. Such people who have this deficiency because of the G6PD enzyme results in leaving the blood cells vulnerable to oxidative hemolysis. A doctor can diagnose G6PD deficiency with a blood test and can advise on these risks. If an individual has G6PD deficiency, physicians advise an individual to avoid any food items. The homozygous condition of G6PD deficiency is often common in human being. Males of a certain age of ten years; are the most vulnerable to oxidative hemolysis from it. 22
Though the appearance of green colour urine after dyeing hair with henna is harmless, the appearance of blood in one’s urine is potentially dangerous and should be brought to the attention of a physician to see whether the individual might have homozygous G6PD deficiency. A simple blood test will confirm whether have G6PD Deficiency, or whether there is blood in urine from some other condition.28 The health risks involved in the pre-mixed paste, not the natural henna; therefore, consumers are advised to avoid henna with synthetic additives. Otherwise, some pastes have been noted to contained synthetic: disperse orange dye, silver nitrate, pyrogallol, carmine, and chromium. These have been observed to be a cause of allergic reactions, chronic inflammatory reactions/ late-onset allergic reactions to hair-dressing materials and textile dyes. For this situation, one has to be careful while buying henna from the market.
In a case, a 15-year old girl died of laryngeal oedema and pulmonary congestion, consistent with anaphylaxis, following conscious ingestion of an unknown amount of henna in a suicide. Acute haemolysis can take place in G6PD-deficient individuals after applying henna dye to the skin. Observed symptoms are anaemia, reticulocytosis, and indirect hyperbilirubinemia. At postmortem physical examination, no traumatic conditions were found. The only pathologic autopsy findings were laryngeal oedema and pulmonary congestion. It was also determined that the stomach contained henna staining. Autopsy findings were consistent with anaphylaxis47. Henna may cause haemolysis in patients with G6PD (glucose-6-phosphate dehydrogenase) enzyme deficiency in regions where it is commonly utilized. In another case of acute kidney injury was recorded in a 34-year-old man with G6PD deficiency from Yangon, Myanmar, after ingesting a herbal remedy of boiled henna leaves. He developed hemoglobinuria, and he underwent five sessions of hemodialysis. His condition improved within seven with full recovery.13
Two siblings, an 11-year-old male, and a 7-year-old girl were admitted to our hospital with a history of vomiting, paleness, dark and low amount of urine, and jaundice without fever, which had begun six hours ago. The patients were told to have ichthyosis Vulgaris disease. Although they were taken to paediatricians many times and were administered various medications for this disease, their skin lesion had persisted. It was observed that henna mixed with water was applied to the whole-body skin lesions by their mother six hours ago. The patients had no complaints, except skin lesions (ichthyosis Vulgaris) until six hours after henna was applied from throat to soles. Six hours after the topical henna mixture application, vomiting and paleness developed. As soon as these complaints developed, their mother washed their whole body covered with the henna mixture. They were the second and third children of a consanguineous marriage with no family history of similar conditions, and they had six healthy siblings. The other siblings had no history of henna application. On physical examination of the 11-year-old male patient, anthropometric measurements were normal; the axillary temperature was 36.6 °C, blood pressure was 110/65mmHg, and heart rate was 142/min. His general appearance was exhausted, very icteric, and pale. Skin from his throat to soles had been dyed red-brown. His liver was 3.5 cm palpable, and his spleen was unpalpable.
Laboratory evaluation showed haemoglobin 6.7 g/dl, Hct 18.8%, WBC 15 200/mm3 and platelets 340000/mm3. In peripheral smear, of leucocytes, 42% were PMNL, 58% were lymphocytes. Eighteen per cent of cells were normoblasts; platelets were adequate and clustered. Anisocytosis and fragmented erythrocytes were present. There was no spherocytosis or elliptocytosis. Reticulocytosis was detected (10%). The osmotic fragility test and sickling test were negative. G6PD screening revealed a deficiency. The direct Coombs test was negative. Urea, creatinine, blood glucose, CK, and electrolytes (NA, K, Ca) were normal, total bilirubin: 8 mg/dl, direct bilirubin: 2.2 mg/dl. After a blood transfusion, haematocrit increased to 22.4%. Subsequently, Hb became stabilized, transaminases, direct, and indirect bilirubin levels fell gradually, and the patient was discharged after four days.29,30
CONCLUSION
Body craftsmanship and decoration is a desideratum present in ancient and modern civilizations, due to different motivations and perceptions. Since the last few years, the use of tattoo and piercing increased, mainly in adolescents and young people, as a popular form of self-expression, evidencing the need for identification and body control against modern alienation. People favour temporary and natural tattoos because they are considered safer than synthetic and long-lasting ones. However, reports on allergic and chronic inflammatory reactions are increasing that ask for higher quality controls. The case of henna shows that also the cosmetic sector requires adequate controls to avoid adulteration, usually considered safe, and polluting with toxic substances to enhance activity. Thus it is essential to verify the state, origin, and identity of the utilized raw material as well as of the marketed products.
Continuous use of such contaminated cosmetics could increase some metal levels in the human body beyond acceptable limits, as well as induction of severe allergic dermatitis in susceptible personnel due to unsafe constituents that were not mentioned on the constituent list of the black henna package. Putting henna on the dermal of these infants can cause their red blood cells to burst. For pregnancy or breastfeeding: It is unsafe to take henna by mouth if a woman is pregnant. There is little evidence that it may cause a miscarriage. It is also unsafe to take henna if a woman is breastfeeding.
ACKNOWLEDGEMENT: Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors/editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
CONFLICT OF INTEREST: NA
SOURCE OF FUNDING: NA






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License