IJCRR - 13(13), July, 2021
Pages: 159-161
Date of Publication: 05-Jul-2021
Print Article
Download XML Download PDF
A Successful Outcome in a Case of Ruptured Rudimentary Horn Pregnancy
Author: Anupama Bahadur, Rajlaxmi Mundhra, Latika Chawla, Juhi Mishra, Megha Ajmani, Jaya Chaturvedi
Category: Healthcare
Abstract:Introduction: Mullerian anomalies occur owing to developmental defect at various stages. They range from Mullerian agenesis to mild arcuate uterus. Lateral fusion defect results in the formation of the rudimentary horn of the uterus. Incidence of rudimentary horn pregnancy is known to occur in 1/100,000 and 1/140,000 pregnancy. Aims: To evaluate a case of the second trimester ruptured rudimentary horn pregnancy Methodology: A 23-year-old primigravida at 18 weeks 4 days gestation presented in shock with gross hemoperitoneum. Results: Prompt intervention with exploratory laparotomy with excision of the rudimentary horn with massive blood transfusion and ventilatory support was lifesaving. The patient conceived spontaneously 4 months of laparotomy and gave birth to a term male baby by caesarean section. Conclusion: Uterine anomalies though rare must be kept in differential diagnosis for any pregnant women presenting with shock and hemoperitoneum as early diagnosis and management can result in a better outcome.
Keywords: Mullerian anomaly, Ruptured rudimentary horn pregnancy, Hemoperitoneum, Maternal collapse, Massive blood transfusion
Full Text:
INTRODUCTION
Maldevelopment of Mullerian ducts occur at different stages like interruption during differentiation, migration, fusion, canalization of Mullerian ducts, and based on this, there can be a spectrum of anomalies.1 On one end remains Mullerian agenesis characterized by failure of development of ducts and at the other end lies arcuate uterus, which is a mild abnormality of canalization. Bicornuate uterus remains midway between these two extremes and is mainly a unification defect. Most patients remain asymptomatic but at times the rudimentary horn may contain a cavity with functional endometrium with the capacity to sustain a pregnancy. Rudimentary horn pregnancy is seen between 1/100,000 and 1/140,000 pregnancy.2
The fate of this atypical pregnancy is mainly rupturing of the pregnant horn during the first or second trimester, resulting in intractable heavy bleeding, with the diagnosis being made intraoperative for maternal rescue.3,4 Literature search has shown that such women have a poor pregnancy outcome in form of abortion, preterm delivery, low birth weight or operative and caesarean delivery.5 The ultrasound diagnosis of a pregnancy in a malformed uterus remains a difficult task. Hysteroscopy and laparoscopy are the gold standard for the diagnosis of uterine anomalies and help differentiate bicornuate from the septate uterus.
We herein present a case of a maternal near-miss survivor with a ruptured rudimentary horn pregnancy necessitating surgical management. She subsequently delivered a full-term healthy baby in her subsequent pregnancy.
CASE REPORT:
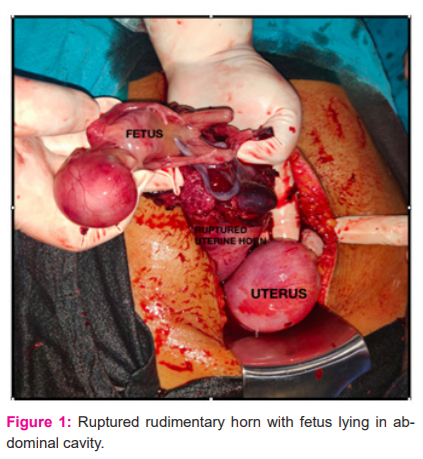
A 23-year-old primigravida at 18 weeks 4 days gestation with no previous antenatal check-ups presented with abdominal pain and distension. On general examination, she was severely anaemic (clinically 5-6 gm%), pulse rate of 110/minutes and blood pressure of 100/60 mm Hg. Bedside ultrasound revealed a live pregnancy corresponding to 13 weeks 1 day’s gestation with the gross intraabdominal collection. Because of suspicion of hemoperitoneum with declining general condition (blood pressure of 70/40 mmHg and tachycardia of 130/minutes), immediate laparotomy was done with blood at hand. Intraoperatively, a unicornuate uterus with a ruptured right rudimentary horn was seen with the fetus lying in the abdominal cavity (Figure1). Approximately 3.5 litres of hemoperitoneum was drained (ESHRE/ESGE class U4a). Right uterine horn excision was done. Three units packed red cell transfusion and 4 units of fresh frozen plasma were transfused intraoperatively. She was kept in the Intensive care unit postoperatively wherein she required ventilatory support and inotropes on her first postoperative day. She received massive blood transfusion (7 units PRBC’s, 4 RDPs and 9 cryoprecipitates) during the recovery period. Postoperatively, she developed lung consolidation with pleural effusion necessitating pleural tapping. She also underwent six serial hemodialyses for acute renal injury. With a multidisciplinary team approach, the patient recovered and was discharged in a stable condition on a post-operative day 30. She received psychological counselling and was advised to delay the next conception. Histopathology report of the specimen confirmed uterine horn within normal histological limits. The patient was lost to follow up. She conceived spontaneously 4 months after laparotomy. She underwent irregular antenatal care at a nearby health care centre. The antenatal period was uneventful. She delivered a healthy male child at 38 weeks gestation by caesarean section. On day 3 of caesarean delivery, she developed shortness of breath and anasarca. She was referred to our hospital in a state of shock and altered sensorium. Arterial blood gas analysis showed severe metabolic acidosis. Immediate intubation was done and started on ionotropic support. She was identified to have acute kidney injury and underwent hemodialysis. SARS CoV 19 test was negative. With serial hemodialysis and broad-spectrum antibiotics, she was finally discharged in stable condition.
DISCUSSION:
Mullerian anomalies are diagnosed in 6.3% and 3.8% of infertile & fertile women as compared to sterile (2.4%) ones.6
Unicornuate uterus accounts for 5–13% of Mullerian duct anomalies with the presence of a rudimentary horn in 74–90% of cases.7,8
Approximately 25% of these horns have a functional endometrium in their cavity and does not communicate with the main cavity of the contralateral Hemi-uterus (ESHRE/ESGE class U4 or ASRM class II b). The rudimentary horn is preferentially situated on right (62%).3
The risk of spontaneous rupture of anomalous uteri is seen in the first trimester but the cause remains unexplained. Literature search shows that there is an abnormal vascular network between these 2 Hemi-cavities of bicornuate uteri, at the level of the midline.9 Weakening of the uterine wall, particularly at the level of the fundus may be a possible hypothesis predisposing to spontaneous rupture.
Sonographic diagnosis of this malformation is a real challenge owing to the limited field of view as compared to other diagnostic imaging modalities and lateral deviation of the rudimentary horn.10 Many times, the diagnosis is made intraoperatively because of suspected hemoperitoneum in early pregnancy.4
Surgery remains the treatment of choice for ruptured rudimentary horn pregnancy. Prompt diagnosis and early surgical intervention is the mainstay of therapy. If fertility has to be preserved, excision of rudimentary horn with ipsilateral salpingectomy remains the recommended surgery. With advancements in minimally invasive surgery, laparoscopy is safe and effective, particularly in early unruptured cases. In the above case, because of a large gravid uterus and significant bleeding, the decision of exploratory laparotomy was made.
The subsequent obstetric prognosis seems reassuring. Diagnostic imaging of the reproductive system after this treatment has shown no negative effect of surgery on future fertility with no reported cases of the ruptured uterus during subsequent pregnancy in the remaining unicornuate uterus after rudimentary horn excision.11
To date, several studies have evaluated reproductive outcomes in women with congenital Mullerian duct anomalies. However, evidence from well-controlled studies is lacking on the risk of rupture uterus before or during labour after excision of the rudimentary horn. Though this risk is rare, obstetricians should always prognosticate their patients about maternal and fetal complications. It has been reviewed that unicornuate uterus has 2.7% ectopic pregnancy, 24.3% first-trimester abortion, 9.7% second-trimester abortion, 20.1% preterm birth, 3.8 % intrauterine fetal demise and 51.5% live birth.12
An association of birth defects in fetuses born to mother with congenital uterine malformations have been reported. These defects may due to reduced uterine volumes, which leads to insufficient space for a developing fetus to undergo proper growth, while mechanical pressure impacts the growing fetal structures. Martinez et al. demonstrated that birth defect(s) were 4 times higher among babies born to mothers with uterine defects than in women without such defect. The risk was found to be statistically significant for nasal hypoplasia, omphalocele, limb deficiencies, teratomas, and acardia-anencephaly.13 Zyla et al. in their study found that the most frequent defects were clubfoot and other defects of the limbs.5 No such defect was seen in our case.
CONCLUSION:
Uterine anomalies though rare must always be considered in early pregnant lady presenting with hemoperitoneum. Timely diagnosis and proper management not only save the patient in the current pregnancy but also increases the chance of a successful future pregnancy.
Acknowledgement: Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors/editors/publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
Conflict of interest: No conflict of interest exists for this article.
Source of Funding: No funding was required for this article.
Author contributions:
Anupama Bahadur & Rajlaxmi Mundhra: Main surgeons, Concept, design, analysis, interpretation, literature search and writing
Latika Chawla: Check draft, analysis
Juhi Mishra. Megha Ajmani: literature search, writing the first draft
Jaya Chaturvedi: Draft check and analysis
References:
-
-
Rechberger T, Kulik-Rechberger B. Congenital anomalies of the female reproductive tract –Diagnosis and management. Ginekol Pol. 2011;82:137–45.
-
Jain R, Gami N, Puri M, Trivedi SS. A rare case of intact rudimentary horn pregnancy presenting as hemoperitoneum. J Hum Reprod Sci. 2010;3:113–5.
-
Nahum GG. Rudimentary uterine horn pregnancy: the 20th-century worldwide experience of 588 cases. J Reprod Med. 2002; 47:151–163.
-
-
Ahmed Y, Shahzadi M & Abdelbaset M.Tale of rudimentary horn pregnancy: case reports and literature review. J Maternal-Fet Neona Med.2019; 32:4, 671-676,
-
-
?y?a MM, Wilczy?ski J, Nowakowska-G??b A, Maniecka-Bry?a I, Nowakowska D. Pregnancy and Delivery in Women with Uterine Malformations. Adv Clin Exp Med. 2015;24(5):873?879. doi:10.17219/acem/23171
-
Raga F, Bauset C, Remohi J, Bonilla-Musoles F, Simon C, Pellicer A. Reproductive impact of congenital Mullerian anomalies. Hum. Reprod. 1997;12:2277–2281
-
Grimbizis GF, Gordts S, Di Spiezio SA, Brucker S, De Angelis C. The ESHRE/ESGE consensus on the classification of female genital tract congenital anomalies. Hum Reprod. 2013 Aug;28(8):2032-44.
-
Bruand M, Thubert T, Winer N, Gueudry P, Dochez V. Rupture of Non-communicating Rudimentary Horn of Uterus at 12 Weeks' Gestation. Cureus. 2020;12(3):e7191. Published 2020 Mar 6. doi:10.7759/cureus.7191
-
Nazzaro G, Locci M, Marilena M, Salzano E, Palmieri T, De Placido G. Differentiating between septate and bicornuate uterus: bi-dimensional and 3-dimensional power Doppler findings. J Minim Invasive Gynecol. 2014;21(5):870?876. doi:10.1016/j.jmig.2014.03.023
-
Sonographic findings of early pregnancy in the rudimentary horn of a unicornuate uterus: a two-case report. Dove CK, Harvey SM, Spalluto LB. Clin Imaging. 2018;47:25–29.
-
Pados G, Tsolakidis D, Athanatos D, Almaloglou K, Nikolaidis N, Tarlatzis B. Reproductive and obstetric outcome after laparoscopic excision of functional, non-communicating broadly attached rudimentary horn: a case series. Eur J Obstet Gynecol Reprod Biol. 2014;182:33?37. doi:10.1016/j.ejogrb.2014.08.023
-
Reichman D, Laufer MR, Robinson B. Pregnancy outcomes in unicornuate uteri: a review. Fertil Steril. 2009;91:1886–94.
-
Martinez-Frías ML, Bermejo E, Rodríguez-Pinilla E, Frías JL. Congenital anomalies in the offspring of mothers with a bicornuate uterus. Pediatrics. 1998;101(4):E10. doi:10.1542/peds.101.4.e10
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License