IJCRR - 13(13), July, 2021
Pages: 28-32
Date of Publication: 05-Jul-2021
Print Article
Download XML Download PDF
A Comparative Analysis of Scoring Systems in Upper Gastrointestinal Bleed to Predict Mortality and Rebleed among Patients from South India
Author: Aradya H V, Deepak Suvarna, Anurag Lavekar, Nandeesh HP, Vijay Kumar T R, Anupama C
Category: Healthcare
Abstract:Introduction: One of the major gastroenterological emergencies encountered is Upper Gastrointestinal bleeding. The major factors which influence the bleeding are the age of the patients, Comorbid conditions, Haemoglobin, ulcer size, shock, and need for repeated blood transfusion. The increased mortality rate among patients with upper gastrointestinal bleeding is due to rebleeding. Objective: To compare the Sensitivity, Specificity of the various scoring system in predicting the outcome of upper gastrointes�tinal bleeding. Methodology: A Prospective study was conducted at JSS Hospital, Mysore, India inMarch 2018. to September 2018. Compari�son of different scoring systems (Rockall, Blatchford, AIMS 65, T score, and PNED score) was done using the ROC curve in predicting the risk of rebleed and mortality. Results: The area under the curve was more for the PNED Score, followed by Rockall Score. It was least for the T Scoring Technique when compared with Mortality Scoring Pattern with the risk scoring. All the scoring systems were found to be statisti�cally Significant for the Mortality risk factor except for Blatchford Score. The different risk scoring for rebleeding was found to be statistically significant for all Scores except for the PNED Score which was significant. Conclusion: Rockall score, PNED, Blatchford Glasgow score and AIMS 65 has very good sensitivity, specificity, and negative predictive value for rebleed and mortality. However, their positive predictive value for rebleed and mortality is a limiting factor.
Keywords: GI Bleed Scoring, Rebleed, Duodenal Ulcer, Mortality
Full Text:
Introduction:
One of the major gastroenterological emergencies encountered is Upper Gastrointestinal bleeding. It is considered to be one of the most challenging and life-threatening problems which require immediate hospitalization and surgical intervention for the better outcome of the patient.
The overall mortality of upper gastrointestinal bleeding ranges from 10 % to 40% among the patients who are more prone to bleeding disorders and with other comorbid illnesses.1
The causes of upper gastrointestinal bleeding range from Mallory Weiss tear to large variceal bleeding. The major factors which influence the bleeding are the age of the patients, Comorbid conditions, Haemoglobin, ulcer size, shock, and need for repeated blood transfusion. The increased mortality rate among patients with upper gastrointestinal bleeding is due to rebleeding.2
All the patients suffering from Upper gastrointestinal bleed are hospitalized and subjected to endoscopic examination irrespective of type (variceal or nonvariceal), quantity and severity of the bleeding. The endoscopic examination and the treatment of upper gastrointestinal bleeding within 24 hours can reduce mortality significantly.
To assess the risk of mortality and other complications related to upper gastrointestinal bleeding various scoring methods have been developed. Few of the scoring system requires the usage of endoscopy findings to conclude the risk and few of the scoring systems doesn’t require an endoscopy to arrive at the risk assessment of upper gastrointestinal bleeding.
One of the most common risk assessment scores used is Rockall Score3 and Progetto Nazionale Emorragia Digestiva (PNED) 4 which require the findings of endoscopy before calculating the risk score. There are still many scoring systems that are used to assess the risk score using endoscopy, but they are inferior to the Rockall Score and PNED score. The scoring system using endoscopy can cause a delay in arriving or calculating the risk score due to delay in the performing endoscopy in our health care setting .5
Hence other scoring systems were developed which don’t require the findings of the endoscopy and determine the risk by the pre-endoscopic scores for upper GI Bleeding were ‘admission’ Rockall Score, Glasgow Blatchford score, and the AIMS65 score. These scoring systems use clinical, hemodynamic, and quickly available laboratory values for Glasgow Blatchford and AIMS65 Scoring. Few studies suggested that these scores could be used to identify patients at very low risk which can be managed in the outpatients. 6,7
In our study, we have tried to compare the different scoring methods used in risk assessment of Upper gastrointestinal bleeding.
Objective:
To compare the Sensitivity, Specificity of the various scoring system in predicting the outcome of upper gastrointestinal bleeding.
Materials and Methods:
A Prospective study was conducted at JSS Hospital, Mysore, India inMarch 2018. to September 2018. All the patients who were admitted to the department of medical gastroenterology with a history of hematemesis and melena during the study period were included in the study. Patients in whom Upper Gastroendoscopy was not possible were excluded from the study. A detailed history and clinical examination were done. Complete hemogram, Liver Function Test, Renal Function Test, Upper Gastroendoscopy was done for included patients. Statistical analysis was done using SPS 17. Comparison of different scoring systems (Rockall, Blatchford, AIMS 65, T score, and PNED score) was done using a ROC curve in predicting the risk of rebleed and mortality. A correlation test was used to check the association between Mortality and rebleed with Hemoglobin, creatinine, and Total Leucocyte Count. The Ethical Clearance from the University was obtained.
Results:
A total of 198 Patients who were included in the study were analyzed. The overall mortality rate was 12.6 % (25/198). The rebleed rate was 16.1 % (32 / 198). The mortality rate in patients with rebleed was 40.6 % (13/32).
The most common causes of upper Gastro-Intestinal bleeding were ulcers in the duodenum and oesophagus, 39 each (19.6 %). Oesophagal varices were seen in 16.6% of the cases. Gastric Varices (10.6%), Gastric Ulcer (9.5%), Portal Gastropathy (9%), Mallory Weis Tear (4.5%), GRED (4%) were the other common etiologies responsible for the bleeding in the upper gastrointestinal Bleeding ( Table 1).

Rebleed and mortality were correlated with the levels of Hemoglobin, Levels of Creatinine, and Total Leucocyte Count.
The Hemoglobin and total Leucocyte count was found to be Positively Correlated with both Rebleeding and Mortality among the cases. The Creatinine level was found to be negatively Correlated with mortality among the cases and positively correlated with Rebleed ( Table 2 and 3).
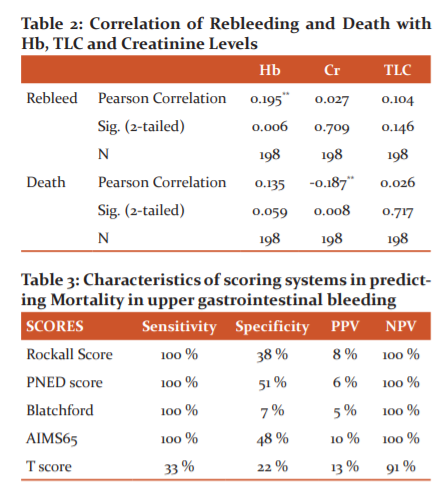
The sensitivity was found to be 100 % for Rockall Score, Blatchford Score, AIMS65 Score and PNED Score. T Scoring technique was found to have a lease sensitivity of 33% when compared to other scoring techniques. The specificity was found to be high for the PNED Scoring technique at 51 %, Followed by AIMS65 Scoring at 48 %. The Blatchford Score had a specificity of only 0.7%. The negative Predictive value was 91% for T Score and 100 % for all the remaining scoring Systems. Positive Predictive value was highest for T Score and least for Blatchford Scores (Graph 1).
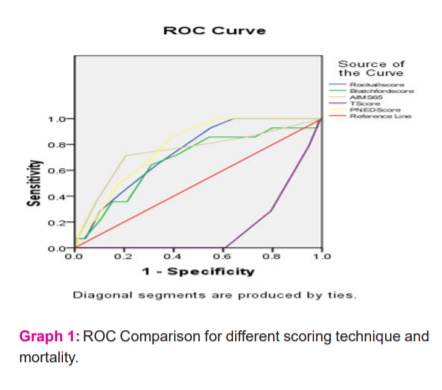
The area under the curve was more for the PNED Score, followed by Rockall Score. It was least for the T Scoring Technique when compared with Mortality Scoring Pattern with the risk scoring. All the scoring systems were found to be statistically Significant for the Mortality risk factor except for Blatchford Score ( Table 4).
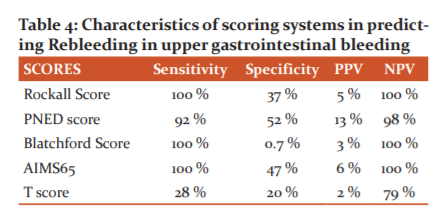
The sensitivity was found to be 100 % for Rockall Score, Blatchford Score, AIMS65 Score. It was 92% for PNED Score and 28% for the T Scoring technique. The specificity was found to be high for the PNED Scoring technique at 52 %, Followed by AIMS65 Scoring at 47 %. The Blatchford Score had a specificity of only 0.7%. The negative Predictive value was 98% for T Score and 79 % for the T score. The remaining score had a 100% Negative Predictive Value. Positive Predictive value was highest for PNED Score (13%) and AIMS65 Score (6%) (Graph 2).
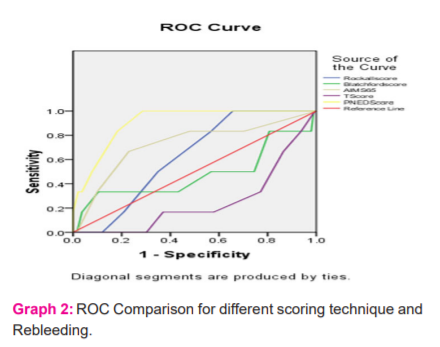
The different risk scoring for rebleeding was found to better with the PNED Score covering more area followed by AIMS65 Score. T score showed the least covered area under the curve. All the Scoring was found to be statistically insignificant except for the PNED Score which was significant.
Discussion:
Out of the total 198 cases which were analyzed, the common causes of Upper Gastrointestinal Bleeding seen in our study was similar to various studies .8,9
In our study, we tried to evaluate a total of 5 different scoring systems that can predict the outcome of upper gastrointestinal bleeding in terms of mortality and rebleeding among the patients. The scoring techniques like AIMS65, Glasgow Blatchford score, and T Score were the scores that didn’t require emergency endoscopy to determine the outcome. Rockall and PNED Risk scoring required the findings of the endoscopy to arrive at any conclusion.
Of all these scoring systems it is the AIMS65 Score that can determine the outcomes of the Patients without considering the comorbid conditions which are suffered by the patients. Few of the researcher evaluated the GBS scoring without considering the endoscopic findings or the comorbid conditions and its termed as Clinical Rockall Score .3,4,7,8
In our study, we could conclude that the usage of Blatchford Score and AIMS 65 both were equally useful (Sensitivity 100%) in determining the mortality than T Scoring System among those patients in whom it was not able to perform endoscopy within 24 hours. in the studies done by various authors .10,11,12. The limitation of the AIMS65 Scoring was the low Positive Predictive value (10%) which means a significant number of low-risk patients with upper GI Bleeding will be missed.
Many of the research studies reported that Rockall Score, Blatchford, AIMS 65 Score, and PNED Score were found similar to the predicting mortality which was comparable to other studies .13,14,15
In the study done by Tammaro L et al.16, the T-score was found to use in the triage patients who are likely to have high-risk endoscopic stigmata and therefore need intervention. The conditions like rebleeding, to predict the high-risk endoscopic stigmata and mortality was found to be similar to GBS. The findings of our study were contradictory to our study findings where T score was found to have the least sensitivity among all the scores in predicting mortality.
According to Tammaro and collaborators,17 a T-score of ≤ 6 was able to predict the presence of high-risk endoscopic stigmata. The Specificity was 96% and the Positive Predictive value was 74.5% in predicting the need for an early endoscopy. He also recommended the use of non-endoscopic scoring Rockall and GBS score in acute GI Bleeding.
The major aspect of the risk scoring assessment for the upper gastrointestinal is the timing of the endoscopy. The timing of the endoscopy determines which risk scoring assessment is better in predicting the outcome of mortality or rebleeding among the patients.
Bhakurun suggested that endoscopy is always beneficial in reducing mortality and improving the outcome is performed within 24 hours from the admission. Though Endoscopy is not associated with the reduction of mortality or rebleeding it will help increase the efficiency of the care of high-risk patients and reducing the duration of hospital stay. These benefits of performing endoscopy give an added advantage of the risk scores which uses endoscopy when compared to risk score without endoscopy.18
Conclusion:
Duodenal and oesophageal ulcers are the most common causes of Upper GI bleed in this study. Rockall score, PNED, Blatchford Glasgow score, and AIMS 65 have very good sensitivity, specificity, and negative predictive value for rebleed and mortality. However, their positive predictive value for rebleed and mortality is a limiting factor.
Acknowledgment: Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors/editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
Conflict of Intrest: Nil
Source of Funding: Nil
Authors contribution:
Aradia H V: Planning and Data Collection of the study, Analysis of the results, Manuscript Writing and Literature Review
Deepak Suvarna: Manuscript Writing and Literature Review
Anurag Lavekar: Data Collection of the study
Nandeesh HP : Review of the Article and Manuscript Writing
Vijay Kumar T R: Analysis of the study, Data Collection of the study
Anupama C: Analysis of the study, Literature Review
References:
-
Walls R, Hockberger R, Gausche M. Rosen’s Emergency. Medicine-Concepts and Clinical Practice: Elsevier Health Sciences;9 th edition: May 2017.
-
Bogoch A, Gastrointestinal bleeding, Chap-6, Vol 1, Bockus. Gastroenterology, 4th Std. 1985; 1: 65-110.
-
Rockall TA, Logan RFA, Devlin HB, Northfield TC. Risk assessment after acute upper gastrointestinal haemorrhage. Gut .1996;38(3): 316-21.
-
Marmo R, Koch M, Cipolletta L, Italian registry on upper gastrointestinal bleeding (Progetto Nazionale Emorragie Digestive-- PNED 2). Predicting mortality in non-variceal upper gastrointestinal bleeders: validation of the Italian PNED Score and Prospective Comparison with the Rockall Score. Am J Gastroenterol. 2010; 105(6):1284-91.
-
Hearnshaw SA, Logan RFA, Lowe D, Travis SPL, Murphy MF, Palmer KR. Use of endoscopy for management of acute upper gastrointestinal bleeding in the UK: results of a nationwide audit. Gut . 2010; 59(8):1022- 9.
-
Blatchford O, Murray WR, Blatchford M. A risk score to predict the need for treatment for upper gastrointestinal haemorrhage. Lancet. 2000; 356(9238):1318-21.
-
Saltzman JR, Tabak YP, Hyett BH, Sun X, Travis AC, Johannes RS. A simple risk score accurately predicts in-hospital mortality, length of stay, and cost in acute upper GI bleeding. Gastroin Endosc. 2011; 74(6):1215-24.
-
Chan J C H, Ayaru L.Analysis of risk scoring for the outpatient management of acute upper gastrointestinal bleeding. Frontl Gastroent .2011; 2(1):19–25.
-
Subramanian V, Hawkey CJ. Assessing bleeds clinically: what’s the score? Lancet. 2009; 373(9657):5–7.
-
Stanley AJ, Ashley D, Dalton HR, Mowat C, Gaya DR, Thompson E, et al. Outpatient management of patients with low-risk upper-gastrointestinal haemorrhage: multicentre validation and prospective evaluation. Lancet. 2009;373(9657):42-7.
-
Stephens JR, Hare NC, Warshow U, Hamad N, Fellows HJ, Pritchard C, et al. Management of minor upper gastrointestinal haemorrhage in the community using the Glasgow Blatchford Score. Eur J Gastroenterol Hepatol. 2009;21(12):1340-6
-
Palmer K, Nairn M; Guideline Development Group. Management of acute gastrointestinal blood loss: summary of SIGN guidelines. Bri Med J .2008;337: 1832.
-
Yaka E, Y?lmaz S, Do?an NÖ, Pekdemir M. Comparison of the Glasgow-Blatchford and AIMS65 scoring systems for risk stratification in upper gastrointestinal bleeding in the emergency department. Acad Emerg Med. 2015; 22(1):22-30.
-
Hyett BH, Abougergi MS, Charpentier JP. The AIMS65 score compared with the Glasgow-Blatchford score in predicting outcomes in upper GI bleeding. Gastrointest Endosc. 2013; 77(4):551-7.
-
Abougergi MS, Charpentier JP, Bethea E, A prospective multicenter study of the AIMS65 score compared with the Glasgow Blatchford score in predicting upper gastrointestinal haemorrhage outcomes. J Clin Gastroenterol. 2016; 50(6):464-9.
-
Tammaro L, Di Paolo MC, Zullo A, Hassan C, Morini S, Caliendo S, Pallotta L. Endoscopic findings in patients with upper gastrointestinal bleeding clinically classified into three risk groups before endoscopy. World J Gastroenterol. 2008; 14(32): 5046-5050.
-
Tammaro L, Buda A, Di Paolo MC, Zullo A, Hassan C, Riccio E, Vassallo R, Caserta L, Anderloni A, Natali A. A simplified clinical risk score predicts the need for early endoscopy in non-variceal upper gastrointestinal bleeding. Dig Liver Dis. 2014; 46(9): 783-787.
-
Barkun AN, Bardou M, Kuipers EJ, Sung J, Hunt RH, Martel M, Sinclair P. International consensus recommendations on the management of patients with non-variceal upper gastrointestinal bleeding. Ann Intern Med .2010; 152(2): 101-113 .
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License