IJCRR - 13(13), July, 2021
Pages: 24-27
Date of Publication: 05-Jul-2021
Print Article
Download XML Download PDF
Platelet-Rich Plasma in the Treatment of Dorsal Wrist Ganglion
Author: Prakasam N, Vasudevan A, Guru Prasad R, Prabakar M. S., Senguttuvan K, Palani V
Category: Healthcare
Abstract:Introduction: Ganglions are one of the commonest soft tissue lesions that arise from a joint capsule or tendon sheath. The gold standard treatment for this is excision biopsy. The other options are intra-lesional hyaluronidase injection or triamcinolone injection after aspiration. These techniques have drawbacks. Surgery has a formation of scar which sometimes has a chance of becoming an unsightly hypertrophic scar. Aim: To check the effectiveness of Platelet Rich Plasma (PRP) in dorsal wrist ganglion. Materials and Methods: A case-control study in adherence with the principles of the Declaration of Helsinki was conducted on 60 patients. 20 patients were given intra-lesional hyaluronidase injection after aspiration and 20 patients were given intralesional PRP injection after aspiration and another 20 patients were given triamcinolone injection after aspiration. Results: PRP group had lower recurrence rates compared to the other two groups. The Hyaluronidase group had recurrences and required a repeat injection, it was also noted that the capsule thickened after the treatment in these patients. Triamcinolone group had lower recurrence rates at 1 month follow up but this eventually increased over a 6 monthly follow up, they also required a second injection Conclusion: PRP is easy to obtain, safe and cost-effective in the management of dorsal wrist ganglion. More studies to be conducted in the future in a larger population with a larger observational period to confirm this.
Keywords: Protein-rich Plasma, Platelet Rich Plasma (PRP), Ganglion, Hyaluronidase, Triamcinolone
Full Text:
INTRODUCTION:
Ganglion cysts are cystic lesions arising from the soft tissues adjacent to joint capsules or tendon sheaths. These are most commonly seen in the wrists, hands and feet, but they do occur within muscles, menisci and tendons also. These are classified based on their site of origin: the tendon sheath, joint, bone or soft tissue. Of these, the most commonly occurring is the one arising from the tendon sheaths followed by the intratendinous ganglion cyst. Most of these arise from the extensor tendons of the wrist and hand.1
The intraneural ganglions are mostly benign and contain the mucinous substance. These are formed within the nerve sheath of the peripheral nerves. The symptoms of these include peripheral neuropathy. Their pathogenesis is unclear. There are different treatments but all of these have been disappointing and the recurrence rates are high.2
The aetiology of intratendinous ganglion cysts is controversial. One such aetiology is that recurrent injury to the tendon with subsequent cystic degeneration. And this theory holds good because tenosynovitis or associated tendon tears are present in the area adjacent to the ganglion cyst. 1 There are three possible explanations for these cysts so far. One is that they are formed from a capsular defect of a nearby joint, this allows joint fluid to egress and track along the epineurium of an innervating articular branch. The second is that the fluid follows the path of least resistance; and the third being that the cyst takes form due to pressure changes.2,3,4
Similarly, the aetiology of intraneural ganglion cysts has also been unclear. We have observed this from the very first known report (1809) described by Beauchêne till the newer ones. Although materials from these studies support evidence of an elbow joint connection2.
Intraneural recurrences are now becoming commonly recognized. This is probably because of increasing awareness, use of MRI’s and better follow-up by patients 5 with increasing imaging technologies, the joint connections are identified initially and/or postoperatively. 6,7 it is also observed that the intraneural recurrences decrease when the diagnosis is made early and treatments target the articular branch connection. 2
A surgical approach is still the gold standard and has a significantly lower recurrence rate when compared with aspiration and intra-lesional injections.4,8 Arthroscopic excision has limited data but has so far given good outcomes amongst patients and is not considered superior. 9 It was stated by Crijns et al. in 2019 that patients who have undergone hand surgeries have more tendencies toward depression and chronic pain along with an unsightly hypertrophic scar. 10
We wanted a scarless procedure for our patients and we also wanted a low recurrence rate. Hence, the aim of this study was directed to identify the effectiveness of PRP in patients with dorsal wrist ganglion.
METHODOLOGY:
In adherence to the principles of the Declaration of Helsinki, written informed consent was obtained from participants of this study. Permission from the Institutional Review Board was obtained (ACS-MCH/20/JAN/18/09). This was a case-control study conducted at ACS Medical College from 2018 to 2020. 60 patients were chosen for this study, of which, 20 were given PRP treatment, 20 were given the routine hyaluronidase injections and 20 other patients were given triamcinolone injection. An ultrasound was done before the study for all patients.11
Inclusion criteria:
-
Above 18 years
-
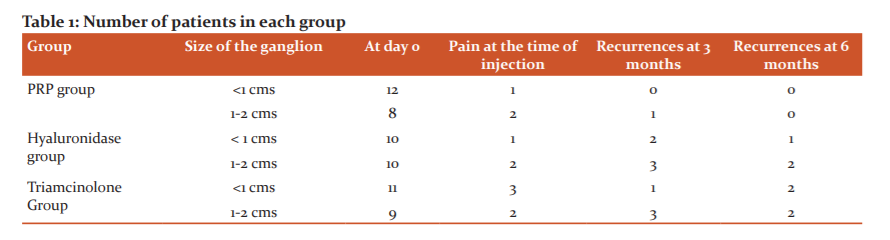
Patients with Dorsal wrist ganglion from all departments– single, size up to 2 cms
-
No comorbidities
-
No bone or joint pathologies
-
Consenting for the study
Exclusion Criteria:
-
Below 18 years of age
-
Multiple ganglia
-
Osteoporosis of the joint
-
Comorbidities like Diabetes mellitus, generalised osteoporosis, blood disorders, bleeding or clotting disorders
-
Patients with HIV, Hepatitis or any other infections
-
Patients on any long-term medications
-
Patients not consenting to the study
Group A patients received Intra lesional PRP injections after aspiration. Review after one week as a routine. Group B patients received intra-lesional hyaluronidase after aspiration. Group C patients were given intra-lesional triamcinolone after aspiration. An 18-gauge needle was used to aspirate the contents. The amount injected into the lesion was always equal to the amount withdrawn from the ganglion.
Following this, patients were asked to rest with a compression bandage or a crepe bandage which was removed after a day.
These patients were then followed up for one year. All three groups were asked to review at 15 days, then at one month, 3 months than at 6 months and then at one year. There was a total of 5 visits to the hospital including the first visit.
Parameters like pain, mobility, size of the swelling were noted during every visit.
PRP PREPARATION:12
PRP was prepared from the patient’s blood. About 5-10 ml of blood was withdrawn from the patient. This was then transferred to a container with an anticoagulant. An initial soft spin of the whole blood (3000 RPM for 5 min at 23°C). This separated the blood into two layers. The topmost layer was pipetted out and subjected to a hard spin (4500 RPM for 10 mins) (Figure 1 and 2). The lower one-third portion constitutes the PRP. This was aspirated in a syringe with an 18-Gauge needle and injected as per the above-mentioned protocol.13
RESULTS:
There were 40 patients, of which 20 were cases and 20 were controls. All the patients were 20-40 years of age. 30 patients were females and 10 were males. 36 of these patients were involved with activities involving fine hand movements.
Parameters compared:
The pain was slightly higher with the PRP group. The cost involved in the treatment was slightly higher with controls. Patients were able to do their routine activities by the second day in both groups. (Table 1)
The following observations were made:
-
There was only one recurrence in the PRP group for the entire period of the study. The patient was given a repeat PRP injection and had no complaints in the follow-up.
-
The hyaluronidase group had 5 recurrences at three-month follow-up and three recurrences at 6-month follow-up.
-
The triamcinolone group had 4 recurrences at three-month follow-up and 4 recurrences at six-month follow-up.
-
All the patients with recurrences were administered with a second dose of PRP / Hyaluronidase/triamcinolone injections depending on the group they were in.
-
On follow-up, the hyaluronidase group had a thickening of the capsule and this mimicked a recurrence in some cases. Similarly, the triamcinolone group had slight hypopigmentation of the overlying skin. But this discolouration slowly vanished with time. This discolouration was probably due to the seepage of the injected steroid.
-
A pain score of more than 3 was considered significant. These patients were managed with paracetamol.
-
Long-term patient satisfaction was higher in the PRP group.
DISCUSSION:
Platelet-rich plasma also called PRP promotes physiological and pathological healing. PRP therapy is nowadays used in surgeries. It is also a treatment of choice for osteoarthritis (OA) and tendinopathies. 14
PRP therapies are used for disorders that have tissue regeneration. PRP Injections are used to treat tendinopathy and they have shown some clinical benefits with pain management.15 it is also known that PRP can reduce inflammatory and angiogenic status. 14
PRP, as we know is biological. Hence it can be used in both physiological and pathological conditions. But to know its importance is a necessity. 16 From chronic tendinopathy to acute traumatic rupture it is observed that multiple cytokines take part.14
PRP as the name suggests is known to contain large amounts of platelets. These are activated to form Prostaglandins (PG) and in turn release Platelet Growth Factor (PGF), this is of significant importance in therapy.12
As stated by Guo et al. exosomes that are released by PRP may lead to angiogenesis through activation of Erk and Akt signalling pathways. This suggests that PRP-induced re-epithelialization may be triggered by activation of Yes-Activated Protein (YAP). 17
The main advantages of PRP are that it is prepared from the patient’s blood and it does not need a high-tech lab for this purpose. The more important advantage being, PRP is autologous and hence there are no reactions to this treatment when compared to the commonly used cortico-hyaluronidases. 18,19,20 on the other hand, there are no pieces of evidence to regulate the formulation and composition of PRP and hence make it difficult for us to know the exact dosage that is to be given. 16-20
As stated by Prakasam et al. in the year 2018 and 2020, PRP is easy to obtain, can be cost-effective, safe and has a lot of healing properties. This can be used to heal ulcers of any origin. 13,21
Although the limitations of this study are its small size and a small follow up period, we conclude by saying that PRP can be used for dorsal wrist ganglion as it is safer, pain-free in the long term and has very minimal recurrences.
CONCLUSION:
PRP is easy to obtain, safe and cost-effective in the management of dorsal wrist ganglion. PRP also fares better in terms of recurrence and pain when compared to the regular Hyalase Injection and Triamcinolone injection. More studies to be conducted in the future in a larger population with a larger observational period to confirm this.
ACKNOWLEDGEMENTS:
We would like to acknowledge and thank our institute for allowing and encouraging us to conduct and write about this study. We would also like to take this opportunity to thank our staff and other members of our department who have helped us in crossing all the obstacles to make this article a successful one.
CONFLICT OF INTEREST:
None
SOURCE OF FUNDING:
None
AUTHOR CONTRIBUTIONS:
Dr. M. S. Prabakar, Dr. K. Senguttuvan, Dr. V. Palani – conceptualisation of the study, overview of the study, review of manuscript and results
Dr. Prakasam N, Dr. Vasudevan A, Dr. Guru Prasad R – Review of literature, conduction of the study, data analysis, manuscript writing,
References:
1. Kim SK, Park JM. intratendinous ganglion cyst of the semimembranosus tendon. Br J Radiol. 2010;83(April):e79–82.
2. Desy NM, Frcs C, Wang H, Ahmed M, Elshiekh I, Tanaka S, et al. Intraneural ganglion cysts: a systematic review and reinterpretation of the world’s literature. J Neurosurg. 2016;125(9):615–630.
3. Lu H, Chen L, Jiang S, Shen H. A rapidly progressive foot drop caused by the posttraumatic Intraneural ganglion cyst of the deep peroneal nerve. BMC Musculoskelet Disord. 2018;19(298):1–5.
4. Harsch I. Para-Articular Cysts in a 64-Year-Old Man. Dtsch Arztebl Int. 2018;115(249b).
5. Mathoulin C, Gras M. Arthroscopic Management of Dorsal and Volar Wrist Ganglion Dorsal ganglion Volar ganglion Wrist arthroscopy Treatment. Hand Clin. 2017;33:769–777.
6. Kodaira S, Nakajima T, Takahashi R, Moriya S, Nakagawa T. A case of intra-articular ganglion cysts of the knee joint?: correlation between arthroscopic and magnetic resonance imaging. BMC Med Imaging [Internet]. 2016;16(36):8–11. Available from: http://dx.doi.org/10.1186/s12880-016-0138-8
7. Mao Y, Dong Q, Wang Y. Ganglion cysts of the cruciate ligaments?: a series of 31 cases and review of the literature. BMC Musculoskelet Disord [Internet]. 2012;13(137):1–4. Available from: BMC Musculoskeletal Disorders
8. Miralles JR, Cisneros LN, Escolà A, Fallone JC, Cots M, Espiga X. Type A ganglion cysts of the radiocapitellar joint may involve compression of the superficial radial nerve. Orthop Traumatol Surg Res [Internet]. 2016;102(6):791–794. Available from: http://dx.doi.org/10.1016/j.otsr.2016.05.014
9. Head L, Gencarelli JR, Allen M, Boyd KU. Wrist Ganglion Treatment: Systematic Review and Meta-Analysis. J Hand Surg Am [Internet]. 2015;40(3):546-553.e8. Available from: http://dx.doi.org/10.1016/j.jhsa.2014.12.014
10. Crijns TJ, Bernstein DN, Ring D, Gonzalez RM, Wilbur DM, Hammert WC. Depression and Pain Interference Correlate With Physical Function in Patients Recovering From Hand Surgery. hand. 2019;14(6):830–835.
11. Ting W, Ke W, Chang V, Özçakar L. Ultrasound facilitates the diagnosis of tarsal tunnel syndrome?: intraneural ganglion cyst of the tibial nerve. J Ultrasound [Internet]. 2019;22(1):95–98. Available from: https://doi.org/10.1007/s40477-018-0314-5
12. Everts PAM, Knape JTA, Weibrich G, Schönberger JPAM, Hoffmann J, Overdevest EP, et al. Platelet-Rich Plasma and Platelet Gel?: A Review. J Am Soc Extra-Corporeal Technol. 2006;38:174–187.
13. Prakasam N, Prabakar MS, Reshma S, Loganathan K, Senguttuvan K. A clinical study of platelet-rich plasma versus conventional dressing in the management of diabetic foot ulcers. Int Surg J. 2018;5(10):3210–3216.
14. Andia I, Rubio-azpeitia E. Platelet-rich Plasma Modulates the Secretion of Inflammatory / Angiogenic Proteins by Inflamed Tenocytes. Clin Relat Res. 2015;473:1624–1634.
15. Lacci KM, Dardik A. Platelet-Rich Plasma?: Support for Its Use in wound healing. YALE J Biol Med. 2010;83:1–9.
16. Everts P, Onishi K, Jayaram P, Mautner K. Platelet-Rich Plasma?: New Performance Understandings and Therapeutic Considerations in 2020. Int J Mol Sci. 2020;21(7794):1–36.
17. Guo S, Tao S, Yin W, Qi X, Yuan T, Zhang C. Exosomes derived from platelet-rich plasma promote the re-epithelization of chronic cutaneous wounds via activation of YAP in a diabetic rat model. Theranostics. 2017;7(1):81–96.
18. Ma N. Blood-Derived Products for Tissue Repair / Regeneration. Int J Mol Sci. 2019;20(4581):3–5.
19. Mariani E. Platelet Concentrates in Musculoskeletal Medicine. Int J Mol Sci. 2020;21(1328):1–43.
20. Noh K, Liu XN, Zhuan Z, Yang C. Leukocyte-Poor Platelet-Rich Plasma-Derived Growth Factors Enhance Human Fibroblast Proliferation In Vitro. Orig Artic Clin Orthop Surg. 2018;10(2):240–247.
21. Prakasam N, Vasudevan A, Prasad G, Bala V. New Age Treatment For An Age-Old Problem – PRP For Post - Surgery Non - Healing Venous Ulcers. Eur J Mol Clin Med ISSN. 2020;07(05):185–192.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License