IJCRR - 13(12), June, 2021
Pages: 133-138
Date of Publication: 22-Jun-2021
Print Article
Download XML Download PDF
Prevalence, Risk Factors and Quality of Floaters Among Medical Students, A Questionnaire-Based Study
Author: Nivetha U, M Dheepak Sundar
Category: Healthcare
Abstract:Objective: To assess the prevalence, risk factors and quality of floaters among medical students and to evaluate the association of floaters with related variables. Methodology: A cross-sectional descriptive study was carried out among 331 students belonging to the medical stream. A semi-structured google form questionnaire was used as the study tool. It was designed to assess the factors associated with the prevalence of floaters. The obtained responses were inspected using appropriate statistical tests. Results: Among 331 medical students, 37.76%(n=125) reported visualizing floaters. The presence of floaters was significantly associated with frequent rubbing of eyes (p< 0.05, odds ratio:5.23), myopia (p< 0.05, odds ratio: 1.87), and emmetropia (p< 0.05, odds ratio: 0.47). Factors like age, gender, playing sports and going to the gym were not significantly associated with the presence of floaters. 80%(n=100) of the students reported seeing floaters during the daytime. About 8%(n=10) of the study population were willing to be treated for floaters whereas 83.2%(n=104) were not interested in getting treated. Conclusion: The presence of floaters is quite common among medical students. Myopia and frequent rubbing of the eyes are possible risk factors. Most of the students who had floaters were not interested in getting any form of treatment.
Keywords: Floaters, Myopia, Rubbing of eyes, Flashes, Emmetropia
Full Text:
Introduction:
Floaters or Muscae volitantes are mobile and scattered structures that float in the visual field. 1,2 They are mostly idiopathic or age-related, commonly associated with synchysis and syneresis.1 Though the presence of floaters is a common complaint among the elderly age group, it is nowadays found to be equally prevalent in the younger age group also.3 4 Floaters are frequently associated with refractive errors especially high myopia and they might be an important clue in early detection of Posterior Vitreous Detachment (PVD)especially with a positive history. 5, 6 Floaters do not need any treatment on a large scale. However, when they hinder the quality of the vision, surgical interventions like Nd: YAG Vitreolysis and Pars plana Vitrectomy might be required.10
The study was conducted to assess the prevalence, risk factors and quality of floaters in the student population as hardly a few similar prototype studies have been conducted in the past.
Methodology:
A questionnaire-based cross-sectional study was conducted among the medical students studying in Saveetha Medical College And Hospital, Thandalam, Tamil Nadu in South India. Based on the study conducted by Webb et al. 14, the sample size was calculated as 331 with the formula 4pq/d2. Institutional Ethics Committee approval was obtained and the study was conducted according to the tenets of the declaration of Helsinki.
A semi-structured google form was designed to assess the prevalence of floaters and the risk factors that increase its prevalence among the study population. The questionnaire was designed to assess the possible risk factors of floaters like refractive error, rubbing of eyes, gym and sports activity. The quality of the floaters was assessed by the duration, number, frequency, severity and progression.7-10The association between the floaters and the various parameters were analyzed using Chi-square test and odds ratio. A P-value less than 0.05 was considered significant.
Result:
About 331 medical students studying at Saveetha Medical College And Hospital were provided with the questionnaire of study.
Demographic details:
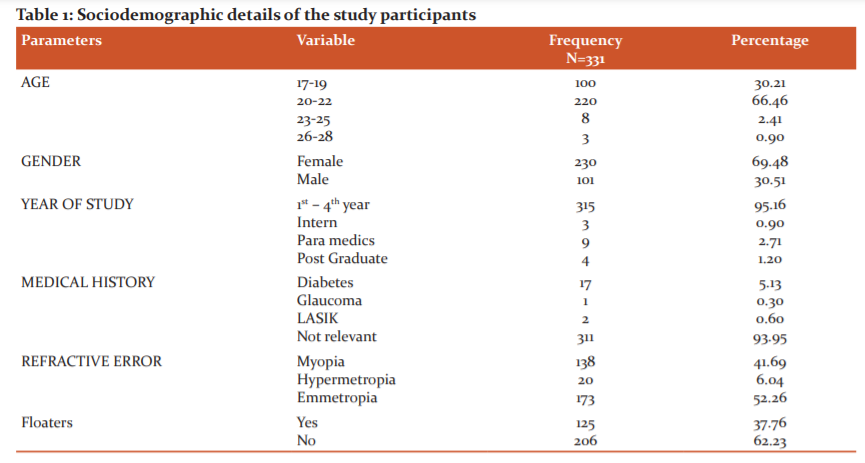
The majority of the students 66.46%(n=220) were in the age group o 20-22 years and most of them were females 69.48%(n=230). About 5.13%(n=17) of
students had a positive history of diabetes. 41.69%(n=138) of the study population had myopia, 6.04%(n=20) had hypermetropia and 52.26%(n=173) had normal vision ( Table 1).
Prevalence of the floaters in the study population:
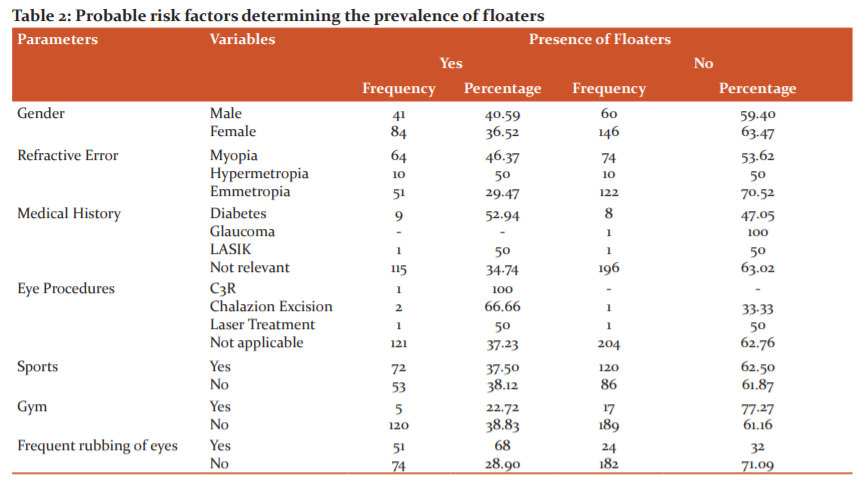
Table No:2 represents the prevalence of floaters and its relative variables among the study population. Overall,37.76%(n=125) of the students reported experiencing floaters. About 40.59%(n=41) among the males responded positively to the floaters and about 36.52%(n=84) among the females reported seeing floaters. 46.37 %(n=64) among the myopes, 50%(n=10) among the hyperopes 29.47%(n=115) among the students with normal vision reported visualizing floaters.
It was also found that about 52.94%(n=9) among the diabetics reported floaters. About 68%(n=24) of the students who rub eyes frequently reported an increase in the number of floaters. 37.5%(n=72) of the study population who played sports and 22.72%(n=5) of the students who went to the gym reported visualizing floaters (Table 3).
Association between floaters and related variables among the study population:
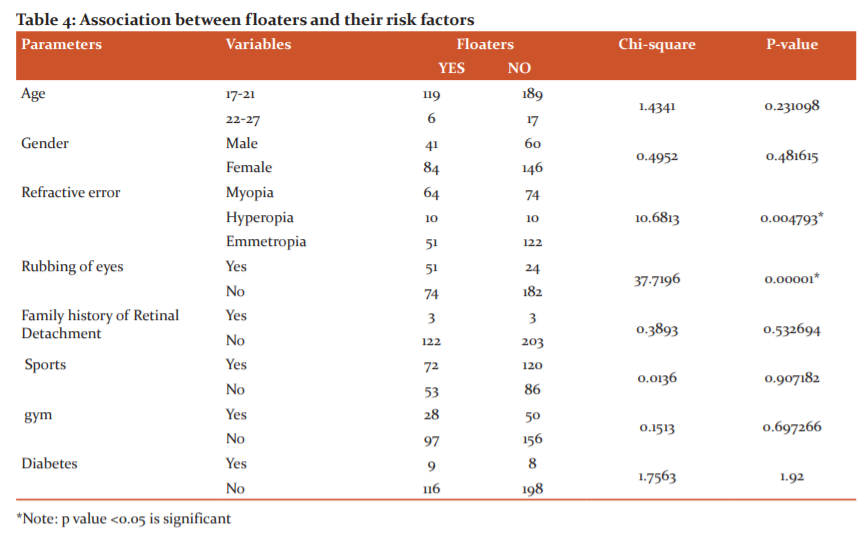
Table No:4 represents the probable risk factors that affect the prevalence of floaters.
Factors like age[p=0.231098], gender[p=0.481615], family history[p=0.532694], playing sports[p=0.907182], going to gym[p=0.697266] or diabetes[p=1.92] didn’t affect the prevalence of floaters. Whereas a statistical significance was established between refractive error [p=0.004793] and prevalence of floaters. There was also a significant increase in the prevalence of floaters among the population who rubbed their eyes frequently [p=0.00001].
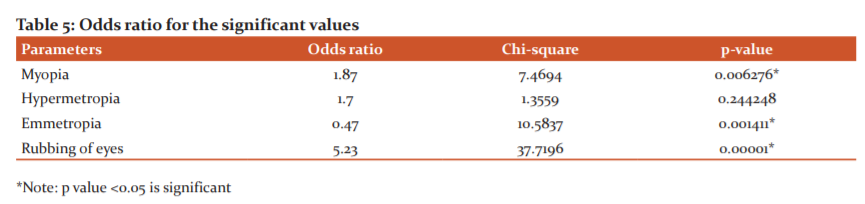
The odds ratio for the significant risk factors:
Table No:5 represents the odds ratio for the significant factors. It was found that there was about a 1.87 times increase in the risk of developing floaters in the myopic population. Whereas frequent rubbing of eyes increased the risk of developing floaters by 5.23 times. The emmetropic population were 0.47 times likely in developing floaters.
Assessment of the quality of floaters:
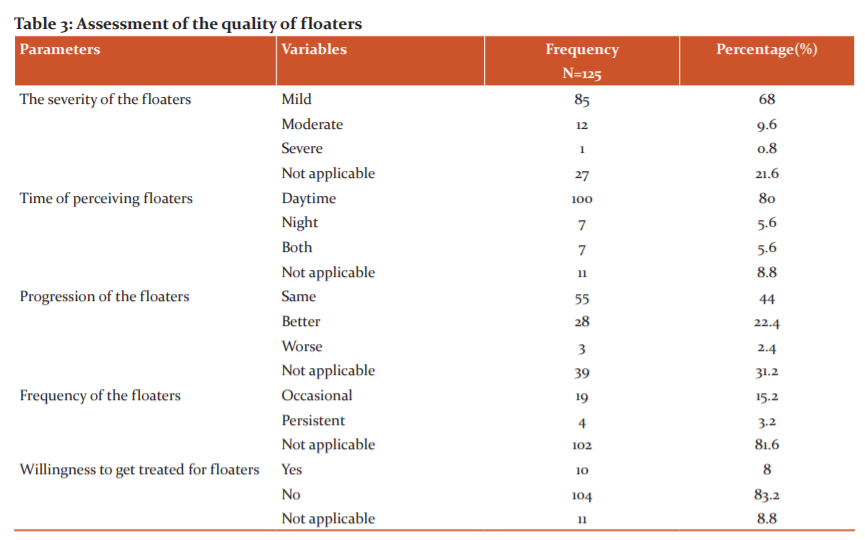
Table no :3 represents the quality of floaters such as frequency, progression, severity, time of visualizing floaters and willingness to get treated for the same as reported by the study population. About 68%(n=85) among the students who reported visualizing floaters graded the severity in visual disturbance as mild and 9.6%(n=12) graded it as moderate and 0.8%(n=1) graded it as severe. 80%(n=100) of the students reported seeing floaters during the daytime. 5.6%(n=7) reported visualizing floaters during the night time and the same percentage (5.6%) of students reported visualizing it both times. When asked about the progression of the floaters. 44%(n=55) of the study population reported no change in progression whereas 22.4% reported it getting better and 2.4% reported it as worsening. When asked about the frequency of visualizing floaters, 15.2%(n=19) reported it seeing occasionally and 3.2%(n=4) reported visualizing persistently. About 8%(n=10) of the study population were willing to be treated for floaters whereas 83.2%(n=104) were not interested in getting treated.
Discussion:
Floaters are lines or dark dots that are visualized clearly against a bright background. They are mostly age-related and idiopathic. However, there is an increased reporting of floaters even among the young population.11-14 Our study was primarily conducted to evaluate the various parameters affecting the prevalence of floaters in the youngpopulation. In our study sample, the prevalence of floaters was about 37.76% whereas , in the study conducted by Blake F. Webb et al, 76% reported seeing floaters.15,16 The increased prevalence in the previous study might be due to the various age groups (18 and above) that was included. While our study was primarily conducted in the younger (17-27) age group. This signifies the fact that the prevalence of floaters tends to rise with increasing age. with the increase in age, vitreous liquefication also increases which is the most important cause of floaters. 17 Floaters are also reported commonly in retinal detachment.18,19
The vitreous body is a homogenous transparent gel composed of collagen and fibrils. Usually, the gel liquefies with age which results in posterior vitreous detachment. However, in the young population, early vitreous liquefaction and anomalous PVD occurs in myopia as a result of myopic vitreopathy. 19,20,21 Thus, myopes tend to have an increase in the number of floaters due to visualization of the shadows caused by clumped degenerated vitreous fibrils or the Weiss ring associated with PVD. Various studies show that most of the clinical population approaching help for floaters included a high proportion of myopes. 15, 21 Similarly, our study revealed a significant association between myopia and floaters.
Almost 50% of the hyperopes also complained of floaters, but the total number of hyperopes (20) in our study was too minimal to elucidate a cause-effect relationship, There was also a statistical significance established between the prevalence of floaters and emmetropia in our study. The significance might be probably due to the unchecked low degree refractive errors which appear to be more common. 20
Our study revealed that frequent rubbing of eyes likely resulted from a 5.23 times increase in the prevalence of floaters. This seems to be a novel finding from our study. Constant and hard rubbing can result in disturbances in the vitreous causing posterior vitreous detachment or vitreous degenerations and thus leading to floaters. 21,22
Full-body workouts and heavy weight lifting may be accompanied b floaters and flashes as PVD is common during their exertion.10. However, our study revealed no significance between workouts and the prevalence of floaters. Only, 5.13% of our total study population were diabetic out of which 52.94% of the students reported visualizing floaters. The number of diabetics in our study were too less to establish a statistical association between diabetes and prevalence floaters.
In our study, only 3.2% of the population reported persistent floaters and 0.8% of the population reported it to be severe. Previous studies suggest that severe and persistent floaters can affect the quality of life. 20 Surgical interventions might be required in such cases of floaters. 3 However, to determine the severity of floaters to support the patient’s complaints objective clinical measures like quantitative ultrasonography and CS and Straylight measures might be carried out. 20,21,22
CONCLUSION:
Our study has many limitations. Restricted age group and a relatively smaller study population were the major ones. The study found that there is an about a 5-fold increase in the prevalence of floaters in the population with frequent rubbing of eyes. Myopia and emmetropia were also the major risk factors. To determine the significance of diabetes on the prevalence of floaters, studies should be directed exclusively in youth with a positive history. Thus, more studies should be conducted in a relatively young population to analyze all major risk factors and treat the cause before it becomes an ocular emergency.
ACKNOWLEDGEMENT: We hereby acknowledge our heartfelt respect and gratitude to all the scholars cited in our article.
SOURCE OF FUNDING: None
CONFLICT OF INTEREST: None
References:
-
Tauzin F. In-depth observations on eye floaters–a challenge to ophthalmology. Mystic Living Today, August 2011a. http://www. Mysticliving today. com/view_page. PHP. 2011.
-
Scotti R, Mascellani SC, Forniti F. The in vitro colour stability of acrylic resins for provisional restorations. Int J Prosthodont. 1997;10:164-8.
3.National Eye Institute. Floaters. https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/floaters [ Accessed 09 August 2020]
4.Laibovitz RA. The vitreous and vitreous floaters: Understanding a common visual complaint. Postgrad Med. 1984 Apr 1;75(5):64-7.
5.Akiba J. Prevalence of posterior vitreous detachment in high myopia. Ophthalmol. 1993 Sep 1;100(9):1384-8.
6.Wilkes SR, Beard CM, Kurland LT, Robertson DM, O'Fallon WM. The incidence of retinal detachment in Rochester, Minnesota, 1970—1978. Ame J Ophthalm. 1982 Nov 1;94(5):670-3.
7.American Academy Of Ophthalmology. Flashes of Light. https://www.aao.org/eye-health/symptoms/flashes-of-light [ Accessed on 09 August 2020]
8.Sowka JW, Kabat AG. How to Make Sense of Flashes and Floaters. Rev Optomet. 2000 Jun 15;137(6):67-.
9.Maggiano J, Yu MC, Chen S, You T, Rathod R. Retinal tear formation after whole-body vibration training exercise. BMC ophthalm. 2020 Dec 1;20(1):37
10.Delaney YM, Oyinloye A, Benjamin L. Nd: YAG vitreolysis and pars plana vitrectomy: surgical treatment for vitreous floaters. Eye. 2002 Jan;16(1):21-6.
11.Webb BF, Webb JR, Schroeder MC, North CS. Prevalence of vitreous floaters in a community sample of smartphone users. Int J Ophthal. 2013;6(3):402.
12. Hidayah FK, Dewi NA, Refa S. Profile of Patients with Floaters in Saiful Anwar Hospital Malang. Inter J Ret. 2018 Aug 24;1(2).
13. Wagle AM, Lim WY, Yap TP, Neelam K, Long KG. Utility values associated with vitreous floaters. Am J Ophth. 2011 Jul 1;152(1):60-5.
14.The University of Illinois College of Medicine. Floaters and flashes. https://chicago.medicine.uic.edu/departments/academic-departments/ophthalmology-visual-sciences/our-department/media-center/eye-facts/floaters/ [Accessed on 09 August 2020]
15. Sebag J. Floaters and the quality of life. Am J Ophth. 2011 Jul 1;152(1):3-4?
16.Jobke S, Kasten E, Vorwerk C. The prevalence rates of refractive errors among children, adolescents, and adults in Germany. Clin Ophth. (Auckland, NZ). 2008 Sep;2(3):601.
17.Milston R, Madigan MC, Sebag J. Vitreous floaters: aetiology, diagnostics, and management. Surv Ophthalmic. 2016 Mar 1;61(2):211-27.
18.Yonemoto J, Ideta H, Sasaki K, Tanaka S, Hirose A, Oka C. The age of onset of posterior vitreous detachment. Clin Exp Ophth. 1994 Feb 1;232(2):67-70.
19.Shiferaw Alemu D, Desalegn Gudeta A, Tsega Ferede A, Worataw Alemu H. Prevalence and degrees of myopia and hyperopia at Gondar University Hospital Tertiary Eye Care and Training Center, Northwest Ethiopia. 2016 Nov;2016(8):85-91.
20.Ben-Eli H, Ernest N, Solomon A. Pathogenesis and complications of chronic eye rubbing in ocular allergy. Surv Ophthalm. 2019;19(5):526-534.
21.Rodge HY, Lokhande S. Refractive Error in Children. Int J Cur Res Rev. 2020; 2(20) Dec;12(23):185.
22.Narayanan NN, Kumar A, Sukumaran K. An Ayurvedic Protocol to Manage Rhegmatogenous Retinal Detachment and the Resultant Macular Hole-A Case Report. Int J Cur Res Rev. 2020 Jul;12(14):10.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License