IJCRR - 13(12), June, 2021
Pages: 123-127
Date of Publication: 22-Jun-2021
Print Article
Download XML Download PDF
A Study of Insulin Resistance and Glucose Tolerance Test in Patients with Essential Hypertension
Author: Rao B Deepak, Chakrapani
Category: Healthcare
Abstract:Background: The number of hypertensive cases has been slowly rising in the world. Many studies have been pointing out the fact that arterial hypertension is an insulin-resistant condition that has been associated with an increased incidence in diabetes. This study puts in a sincere effort to find if there is any relation. This study is intended to be of great help to the community by throwing up some light on this matter. This study is also intended to be of great help to the practising physicians and also academicians. Aims and Objectives: To study insulin resistance and glucose tolerance test in patients with essential hypertension. Materials and Methods: The present study was conducted over a year, 50 patients of which 30 were cases and 20 controlled who was admitted to KMC Attavarand other hospitals under Kasturba medical college. Results: Insulin resistance was about 16 % in cases, with a mean of 1.33 and std deviation of 1.4. No controls had insulin resistance. Conclusion: There was an increased incidence of impaired fasting glucose among hypertensive which was statistically significant.
Keywords: Insulin, Resistance, Glucose Tolerance, Essential Hypertension
Full Text:
INTRODUCTION
The prevalence of hypertension is rising rapidly worldwide and the impact is particularly being felt in developing countries.1 This is due to the epidemiological transition taking place in developing countries leading to alarming increases in non-communicable diseases, especially diabetes and hypertension.2,3 India now has the largest number of diabetic patients in any given country in the world. Hypertension is also likely to follow suit. Risk factors for hypertension may vary between developed and developing nations due to changes in genetic and environmental factors.4,5Thus, studies looking at the relationship between insulin resistance and hypertension in developing countries like India are of great interest. It is still unclear whether hypertension is related to insulin resistance per se or the insulin resistance cluster. Arterial hypertension is an insulin-resistant condition that has been associated with an increased incidence of diabetes. Diabetes mellitus and insulin resistance have been shown to increase future cardiovascular morbidity and mortality. Thus in hypertensive patients, early diagnosis and treatment of abnormal glucose metabolism may be important to reduce cardiovascular mortality.6,7
AIM
To study insulin resistance and glucose tolerance test in patients with essential hypertension.
METHODS AND MATERIALS
The present study was conducted over a year, 50 patients of which 30 were cases and 20 controlled who was admitted to KMC Attavarand other hospitals under Kasturba medical college.
INCLUSION CRITERIA:
-
Patients of over 30 yrs of age of either sex are
-
30 patients with essential hypertension without diabetes are cases, 20 without diabetes or hypertension are controls.
Exclusion criteria:
-
Patients who are diagnosed to have diabetes.
-
Cases of secondary hypertension.
-
All patients or controls below 30 yrs of age.
-
Pregnant, lactating mothers
All cases and controls are subjected to:
-
Detailed history and clinical examination. Anthropometric measure - waist circumference was done.
-
Routine investigations including fasting lipid profile, renal function tests.
-
A glucose tolerance test is performed using 75g of glucose, a fasting glucose sample and a 2 hr postprandial sample are obtained.
-
A fasting insulin venous sample is obtained and insulin resistance is calculated as follows : (HOMA )
-
Insulin resistance = fasting glucose in mmol x fasting insulin sample in, micro lu /d1 22.5
-
Value IR > 2.5 is defined as insulin resistance.
-
A microalbuminuria test is done using the urine dipstick method. A value > 30mg is significant
Results:
Graph 1: Age Distribution:
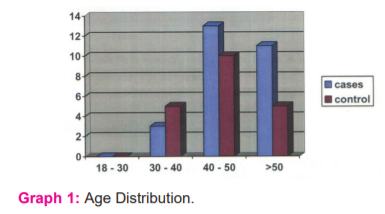
Out of 30 cases 40% between 40 to 50 yrs with a mean of 49.4 and
standard deviation of 9.2.Out 20 controls 50% were between 40 and 50 yrs with a mean of 39.5 and standard deviation of 7.4. (Graph 1)
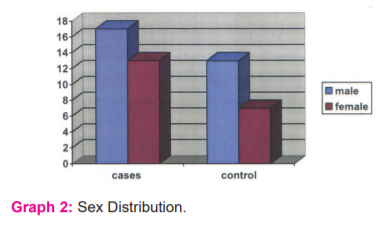
Out of 30 cases, 56 % were male and 44 % were female, in the control group55 % were male and 45 % were female. (Graph 2)
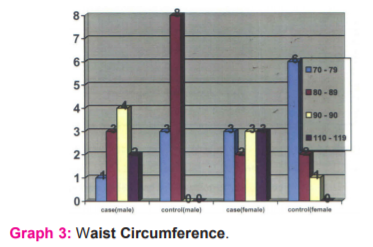
The %of male patients who had a waist circumference of more than90 ems in cases were 76 % while compared to 61 % in the control group with a mean of 96.5 and 83.5, the standard deviation of 12.5 and 3.5, with p value<0.05. Among females, 76 % had more than 80 ems waist circumferences compared to 33 % in the control group with a mean of 95.38 and 79.55.STD deviation of 14.8 and 4.4 with p-value <0.05. The two showed a significant statistical. (Graph 3)
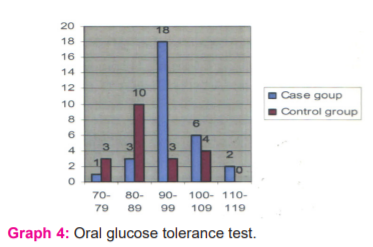
Nearly 26.6 % Of the cases were found to have impaired fasting glucose with (mean of 96.16, std deviation of 8.6) as compared to 20 % of controls (mean of 88.3 and std deviation of 9.5) p-value <0.05. (Graph 4)
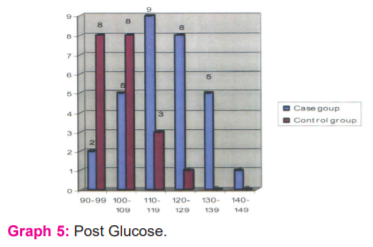
3.3 % of cases had impaired postprandial glucose tolerance test with no controls having impaired postprandial glucose tolerance test (mean of117.7 and 103.3, STD deviation of 12.2 and 18) p-value <0.05. (Graph 5)
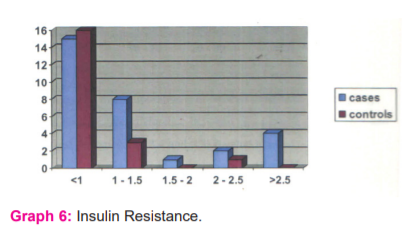
Insulin resistance was about 16 % in cases, with a mean of 1.33 and std deviation of 1.4. No controls had insulin resistance. (P< 0.05) (Graph 6)
A value greater than 2.5 were considered significant (47)
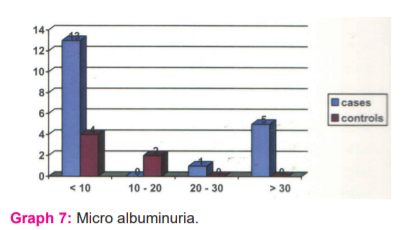
10 % of cases had microalbuminuria compared to none in the control group. There was no statistical difference between the two groups. (Mean 16.5 and 17.4 standard deviations of 18.4 and 9.3).p-value >0.05 (Graph 7)
DISCUSSION:
The number of patients studied was 50 out of which 30 were cases and 20 controls. All the cases studied were diagnosed with hypertension and were on treatment for the same. Most were males in the age group of 40 to 50yrs. Every case and control underwent an oral glucose tolerance test and insulin resistance was calculated using HOMA.
Blood pressure was recorded in the sitting position in the right arm to the nearest 2 mmHg with a mercury sphygmomanometer. Two readings were taken 5 minutes apart and the mean of the two was taken as the blood pressure.
The present study showed a there was an increased incidence of insulin resistance and impaired glucose tolerance among cases with a p-value < 0.05.
The association of HOMA with hypertension• is independent of age, sex, smoking habit and alcohol use. Many patients with hypertension were also found to have impaired glucose tolerance as defined by ADA guidelines. Another factor is the prevalence of obesity which increases the risk factor for insulin resistance and hypertension.
Hoorn Study data, showed men with high insulin predicted a 1.5-fold increase in CVD, increased waist circumference predicted a doubling, and hypertension predicted a two- to threefold increase in risk of CVD.8
It has also been suggested that the insulin resistance syndrome is characterized by the linking of a metabolic entity (insulin resistance, dyslipidemia and obesity) to a homodynamic factor namely hypertension.9
Although earlier studies suggested an association of hypertension with insulin resistance, the question that remains unanswered is
whether hypertension was associated with insulin resistance per se or with the insulin resistance cluster. ( Table 1)
Waist circumference:
The %of male patients who had a waist circumference of more than90 cms in cases were 76 % while compared to 61 % in the control group(p<0.05). Among females, 76 % had > 80 cms waist circumference as compared to 33 % in the control group (p<0.05)
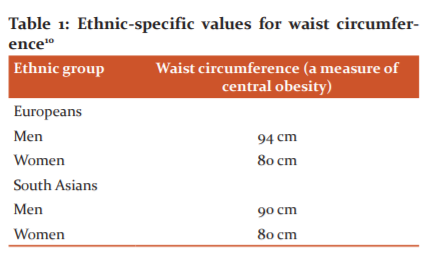
Central obesity is an essential element in this definition, with different waist circumference thresholds set for different race/ethnicity groups:
Oral glucose tolerance test:
Out of the 30 patients studied 8 of the 30 cases had impaired fasting glucose one out of 30 cases had impaired postprandial tolerance. That is 26.6 % Of the cases were found to have impaired fasting glucose as compared to 20 % of controls ( p<0.05). And 3.3 % of cases had impaired postprandial glucose tolerance test with no controls having impaired postprandial glucose tolerance test (p<0.05). None of the cases or controls had overt diabetes.11 Earlier studies showed a high incidence of impaired fasting glucose as high 68.5% of the patients recruited for the study.
Insulin resistance:
The number of patients diagnosed to have insulin resistance was about 16 % in cases as compared to none in the control group (p<0.05)The Chennai Urban Population Study (CUPS) was an epidemiological study involving two residential areas in Chennai in southern India. 1262participated in this study.9
The mean HOMA IR value in hypertensives was 1.046, significantly higher than that observed in normotensives, e.g. 0.81 (p=0.001).9
The study showed that the components of IRS, e.g. insulin resistance (HOMA IR), obesity, hyperglycemia and hypertriglyceridemia, clustered in the native
Indian population and this Insulin Resistance factor are associated with hypertension. It has been suggested that the insulin resistance syndrome is characterized by the linking of a metabolic entity (insulin resistance, dyslipidemia and obesity) to a homodynamic factor namely hypertension. The present study shows that clustering of IRS factors is associated with hypertension in native Indians, who are already known to have high prevalence rates of diabetes and CAD. Hypertension is known to be associated with insulin resistance and both could independently predispose to CAD. However, the underlying mechanisms are not clearly defined. Potential explanations for the frequency with which insulin resistance and hypertension are associated could be the coincidence of two common abnormalities, the causation of one by the other, or the existence of a common underlying factor. The first explanation appears unlikely, with a preponderance of evidence suggesting that the two conditions are related1. It also appears unlikely that hypertension causes insulin resistance, as glucose uptake is not affected in experimental renovascular hypertension and because lowering blood pressure in individuals with hypertension does not necessarily improve glucose uptake. There is, however, greater forearm vascular resistance in obese than in non-obese adolescents, with glucose uptake across this issue inversely related to vascular resistance, suggesting that vascular resistance may play a role in some aspects of insulin action.2 The converse, that insulin resistance may cause hypertension, appears more likely to be a factor. Fasting insulin levels correlate with systolic blood pressure, and the drop in blood pressure following weight loss is related to the improvement in insulin sensitivity. Interestingly, in hypertensive obese individuals, somatostatin decreases both the insulin level and blood pressure, suggesting an effect of hyperinsulinemia. Insulin can lead to sodium retention 3 and angiotensin II-mediated aldosterone production can change vascular structure and function, can altercation flux, and can activate the sympathetic nervous system. In both obese and non-obese individuals during water diuresis, however, sodium excretion decreases with a euglycemic-hyperinsulinemic clamp, so insulin resistance can not be certainly proposed as the cause of hypertension.
Microalbuminuria:
The total percentage of patients found to have microalbuminuria were 10 % in cases where none in the control group. However, a nonsignificant statistical difference was found between the two groups. Microalbuminuria is defined as the persistent elevation of albumin in the urine, of 30-300 mg/day (20-200 µg/min). These values are less than the values detected by routine urine dipstick testing, which does not become positive until protein excretion exceeds 300-500 mg/day Although the
24-hour urine collection was previously the gold standard for the detection of microalbuminuria, it has been suggested that screening can be more simply achieved by a timed urine collection or an early morning specimen to minimize changes in urine volume that occur during the day.
Microalbuminuria is unlikely if the albumin excretion rate is below 20µg/min in a timed collection or if the urine albumin concentration is less than 20 to 30 mg/L in a random specimen. Higher values (particularly those just above this range) may represent false-positive results and should be confirmed by repeated measurements. 12
Conclusion:
-
The study showed that there was a higher incidence of obesity (waist circumference) among hypertensive.
-
There was an increased incidence of impaired fasting glucose among hypertensive which was statistically significant.
-
There was a statistically significant higher incidence of insulin resistance in cases group.
-
The study did not show any significant increase in incidence in microalbuminuria between two groups.
CONFLICT OF INTEREST: Nil
SOURCE OF FUNDING: Self-funded
AUTHOR CONTRIBUTION:
-
Dr Rao B Deepak: Chief investigator
-
Dr Chakrapani: Guide
References:
-
Reaven GM, Role of insulin resistance in human disease (syndrome X): an expanded definition. Annu Rev Med; 1993; 44 (1) :121-131
-
Haffner SM, Epidemiology of insulin resistance and its relation to coronary artery disease. Am J Cardiol. 1999; 84 (1) :11-14
-
Kannel WB. Risk stratification in hypertension: new insights from the Framingham Study. Am J Hypertens. 2000; 13 (1): 3S-10S
-
Miccoli R, Ceraudo AM, Manfredi SG, Odoguardi L, Navalesi R Atherogenic dyslipidemia, metabolic syndrome andcardiovascular risk. Cardiologia . 1999; 44 (1) :885-899.
-
Chen W, Srinivasan SR, Elkasabany A, Berenson GS Cardiovascular risk factors clustering features of insulin resistance syndrome (Syndrome X) in a biracial (Black-White) population of children, adolescents, and young adults: the Bogalusa Heart Study. Am J Epidemiol. 1990; 150 (1) :667-674
-
Ferri C, Bellini C, Desideri G, Valenti M, De Mattia G, Santucci A. Relationship between insulin resistance and non-modulating hypertension. Linkage of metabolic abnormalities and cardiovascular risk. Diabetes. 1999; 48 (1) :1623-1630
-
Ferrannini E, Buzzigoli G, Bonadonna R, Giorico MA, OlegginiM, Graziadei L Insulin resistance in essential hypertension. N Engl J Med. 1987; 317:350-357
-
Lehto S, Ronnemaa T, Pyorala K, Laakso M Cardiovascular risk factors clustering with endogenous hyperinsulinemia predict  death from coronary heart disease in patients with type II diabetes. Diabetologia. 2000; 43 (1) :148-155
death from coronary heart disease in patients with type II diabetes. Diabetologia. 2000; 43 (1) :148-155
-
Shanthi Rani CS, Rema M, Deepa R, Premalatha G, Ravikumar R, Anjana Mohan, Sastry NG, Ramu M, SarojaR, Kayalvizhi G, Mohan V. The Chennai Urban Population Study (CUPS). Methodological Details (CUPS Paper No. 1). Int J Diabetes Dev Countries. 1999; 19 :149-157
-
Alberti KG; Zimmet I, Shaw J. The metabolic syndrome-a new worldwide definition. Diabetologia. 2005; 24-30;366:1059-62.
-
Pollard T, Lithell H, Berne. Insulin resistance is a characteristic feature of primary hypertension independent of obesity. Metabolism. 1990; 39: 167-174.
-
Mogensen, CE, Vestbo, E, Poulsen, PL, et al. Microalbuminuriaand potential confounders. A review and some observations on the variability of urinary albumin excretion. Diabetes Care 1995; 18:572.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License