IJCRR - 13(12), June, 2021
Pages: 34-38
Date of Publication: 22-Jun-2021
Print Article
Download XML Download PDF
Colloid Preloading Vs Co-loading During Tourniquet Deflation: An Assessment of Haemodynamic Stability in Total Knee Replacement
Author: Akhya Kumar Kar, Abinash Patro, Monu Yadav, Gopinath Ramachandran
Category: Healthcare
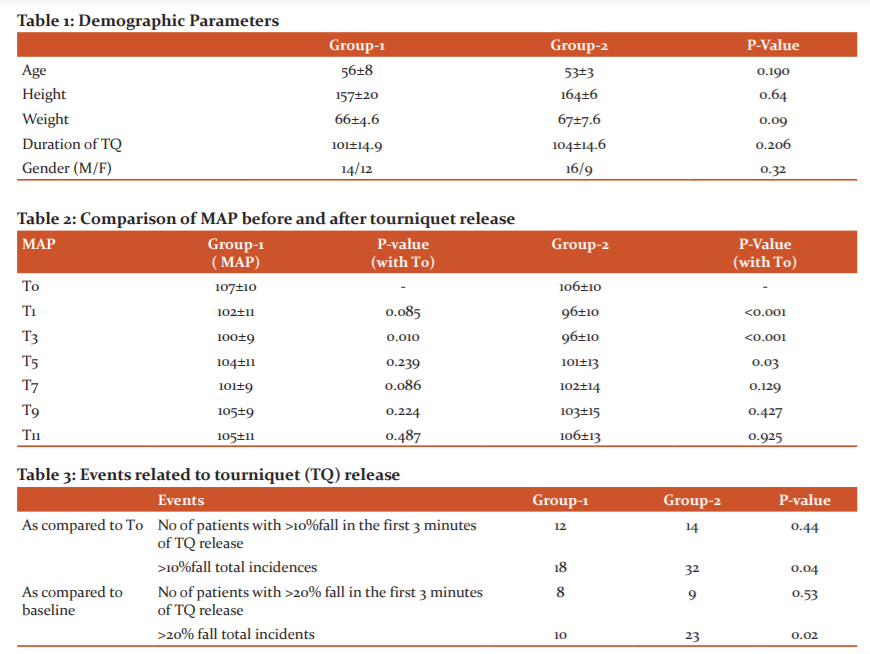
Abstract:Introduction: Tourniquet is an essential part of orthopaedic limb surgeries to limit blood loss and achieve a bloodless field during surgery. Some case reports of life-threatening events at the time of deflating tourniquet prompted us to study the impact of tourniquet release on haemodynamics during knee arthroplasty surgery. This study intended to determine the effect of preloading with 6% HES (130/0.4) on the haemodynamic parameters during tourniquet deflation. Methods: This prospective randomized clinical investigation was undertaken at a tertiary care centre after obtaining written informed consent from ASA I&II patients scheduled for elective total knee arthroplasty under spinal anaesthesia, belonging to the age group of 18 and 60 years. The participants were randomized to two groups (group-1 and 2) of 30 each. In group-1 HES given at 5 ml/kg over 30 minutes before tourniquet deflation and in group-2 colloid infusion done based on haemodynamics after tourniquet release. Baseline vitals and tourniquet pre-release value(T0) compared with 1 minute (T1) to 11 minutes (T11) of post-release vitals. Results: Post-deflation of the tourniquet, in group-1 there was a significant increase in heart rate for 3 minutes(P=0.023), while in group-2 it was high throughout the observation period up to T11(P=0.004). Incidences of 20% fall in MAP as compared to baseline (P=0.02) and 10% fall compared to T0(P=0.04) was significantly higher in group-2. The average MAP was significantly low at T3 in group-1 while it was significantly low through T1 to T5 in group-2, compared to T0. Conclusions: Tourniquet release induced hypotension need attention. Preloading with colloids reduces overall hypotensive episodes.
Keywords: Tourniquet deflation, Hypotension, Total knee arthroplasty, Tourniquets, Spinal anaesthesia, Vasopressors
Full Text:
INTRODUCTION:
A Pneumatic tourniquet is an essential part of orthopaedic limb surgeries; it reduces blood loss and provides a bloodless field during surgery.1 During inflation and deflation of tourniquet, hemodynamic changes occur, which needs attention—many case reports of adverse outcomes published during tourniquet deflation.2,3 Most adverse effects during the deflation period are related to a sudden increase in the volume of distribution, bleeding from the surgical site, circulation of toxic products originated due to prolonged limb ischemia, and release of cementing particles in knee arthroplasty, and associated comorbidities. The adverse events leading to cardiac arrest in literature were attributed to reperfusion syndrome,4pulmonary artery embolization,5,6 and coronary artery vasospasm.7Only a few works of literature available where the impact of tourniquet release on haemodynamics is studied,8 where the mean arterial pressure (MAP) is seen to fall to the extent of 20% as compared to baseline. Fluid management is the key to counter the haemodynamic alteration; however, it is mostly individualized during tourniquet release in the absence of much literature guidance. Preloading is used to reduce hemodynamic variation during spinal anaesthesia; however, there are conflicting views regarding its effectiveness.9Analyzing the effect of preloading before tourniquet release can add to the literature the usefulness of such methods. This study contemplated the primary objective of assessing the impact of preloading of 6% HES (starch,130/0.4) on hemodynamic parameters during tourniquet release. The secondary purpose was to study the effect of tourniquet release on immediate hemodynamic stability and compare preloading and co-loading at the time of tourniquet deflation.
MATERIAL AND METHODS:
This prospective randomized clinical investigation was undertaken at a tertiary care centre from February 2019 to August 2019. This study has the approval of the institutional ethics committee (EC/NIMS/2208/2018) and prospectively registered with the clinical trial registry of India (http://ctri.nic.in/Clinicaltrials, CTRI/2019/01/016838). After obtaining written informed consent, sixty American Society of Anesthesiologist Physical Status ? and ?? (ASAPS-I and II) patients scheduled for elective total knee arthroplasty belonging to both the gender aged between 18 and 60 years were recruited for the study. Patients with hypertension, long-standing diabetes mellitus or on insulin, deranged renal parameters, antiplatelet drugs, altered coagulation profile, and heart rate control drugs like beta-blockers, alpha agonists, calcium channel blockers were excluded from the study. Instances where activation of epidural anaesthesia was required before tourniquet release was also planned to exclude after inclusion.
The recruited patients were randomly assigned to two groups (group-1 and group-2) of 30 patients each according to a computer-generated random number sequence and closed envelope method. Spinal anaesthesia is given with an adequate dose of bupivacaine heavy after epidural catheterization. After spinal anaesthesia, 15ml/kg Ringer lactate infused intravenous route (IV) over 30 minutes and 2 ml/kg/per hour as maintenance fluid. Mean arterial pressure (MAP) fall of more than 30% treated with a bolus of Mephenteramine 6mg IV, the total no of doses required were noted. Vitals before tourniquet release, 2, and 5 minutes after tourniquet inflation was recorded in both the groups. A test dosing of 10 ml HES given to exclude any possibility of an allergic reaction. At the end of the surgery, group-1 patients preloading done before tourniquet release and in group-2, co-loaded with 5ml/kg of HES over 30 minutes. Vitals noted before tourniquet release (T0), 1 min post-tourniquet release (T1), and every 2 minutes after that from 3rd minute to 11th minute in both the groups and named as per the minutes after the tourniquet release time as T3, T5, T7, T9, T11 respectively. Recordings with more than 20% fall in MAP compared to the baseline were treated with 1ml/kg of HES as slow intravenous infusion. If the fall in MAP was more than 30% compared to baseline, then mephenteramine 6mg IV was given to maintain the MAP in a safe range. At the end of the study, the patients were shifted to the postoperative ward for observation and further management. For postoperative analgesia, continuous infusion of 0.125% of bupivacaine administered after activation of epidural space.
Statistical analysis was done using the Statistical Package for Social Science (SPSS17.0 Evaluation version). Qualitative data were compared with the chi-square test, and quantitative data were compared within the group against baseline values using the paired t-test. The results were expressed as mean ± standard deviation, P <0.05 as significant and highly significant if <0.001. The maximum fall in MAP in the co-loading group was 20% as per the literature data with a MAP of 80mmHg where no preloading was done,8 and we assumed preloading group MAP fall would be restricted to 5%. Considering a difference of 15%, post-deflation MAP in preloading to be 92mmHg and standard deviation of 15, G*power (3.1.9.4) software was used for sample size calculation. With an alpha error of 5% and power of 80%, a sample size of 26 was required in each group. Hence we recruited 30 in each group to account for possible exclusions.
RESULTS:
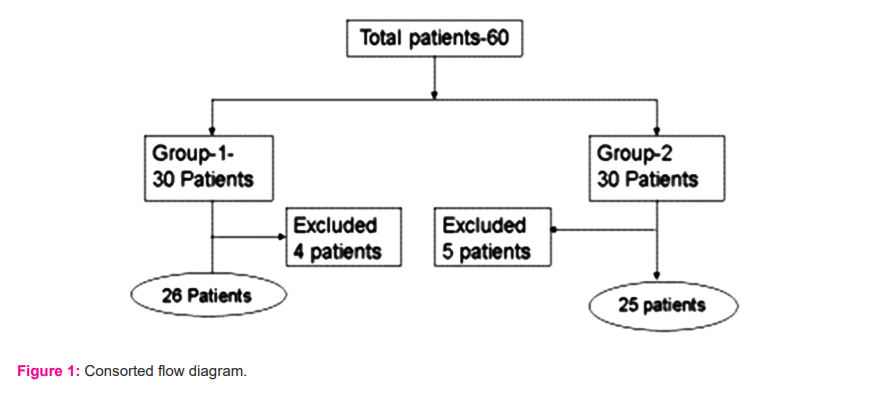
We studied 30 patients in each group. Nine patients were excluded (4 Group1 and 5 Group2) from the study as epidural space activated during surgery (Figure-1). Both groups were comparable about demographic parameters (Table-1). Tourniquet (TQ) inflation did not produce any significant change in HR (P=0.082) or MAP (0.906) after 5 minutes of inflation. Post-deflation of the tourniquet, increase in heart rate compared to T0 was at a statistically significant level for 3 minutes (P=0.023) in group-1 while in group-2 it was high throughout the observation period to T11 (P= 0.004). The MAP was comparable in both groups throughout the observation period. The average maximum fall of MAP was found at T3 was 12% in group-1 whereas it was 17% in group-2 compared to baseline. A significant relationship was found between the groups when the number of events of 20%fall in MAP compared to baseline or 10% fall compared to T0 was noted (Table-2). The average MAP was significantly low at T3 in group-1 while it was significantly low through T1 to T5 in group-2 when compared to T0 (Table-3). There were no incidences with a 30% fall of MAP, and no significant difference between or within the groups at 30 minutes of tourniquet release.
DISCUSSION:
Our study outcome has shown that tourniquet deflation alters haemodynamic parameters which need attention. Our study assumption of maximum fall in MAP to the range of 20% was based on similar literature that further observed that the MAP almost reaches to T0 value at around 12 minutes of tourniquet release; hence we planned to monitor the vitals to 11 minutes.8The watched maximum fall of MAP was found at T3 in both groups were less as compared to the literature data,8 probably ongoing colloid resuscitations partially helped to maintain stable vitals. The maximum fall in MAP was more (12%) than our assumption of 5% in the preloading group; however, the fall was transient and recovered faster. The combined effect of redistribution and bleeding into the joints is the primary reason for this fall. Studies have proven that the low blood pH and low base excess found at 1,3 and 1,3, 5minute post tourniquet release respectively. The malondialdehyde (MDA) level,10 a marker of oxidative stress injury is high in 5 min post tourniquet release,11which almost correlates severity of the fall of MAP in both the groups.
Preloading helped to attenuate the haemodynamic instability related to tourniquet release with an overall decrease in hypotensive episodes during the observation period (Table-3). During the early phase of 3 minutes of tourniquet release, the preloading group fared better with limited immediate fall (T1) and initial stabilization of MAP compared to the co-loading group. (Table-2) As compared to T0, the maximum fall in MAP was almost 10% in group-2 while it was within the 5% range in group-1. Though MAP at T0 can be used as a guide to predict the probability of adverse outcome during tourniquet release however it is crucial to observe the relation to baseline values as a 10% fall from T0 after tourniquet release may not always be within the acceptable range.
Older age group and patients with comorbidities are a vulnerable group of patients where deflation of tourniquet may cause significant alteration of haemodynamic parameters. One of the reasons for limited fall in MAP in our study participants may be the exclusion of this sub-group of patients, however observing the magnitude of the impact of tourniquet deflation and benefit of fluid resuscitation, maintaining euvolemia and safe vitals before tourniquet release by judicious use of intravenous fluids will prevent any untoward incident at the time of tourniquet deflation.
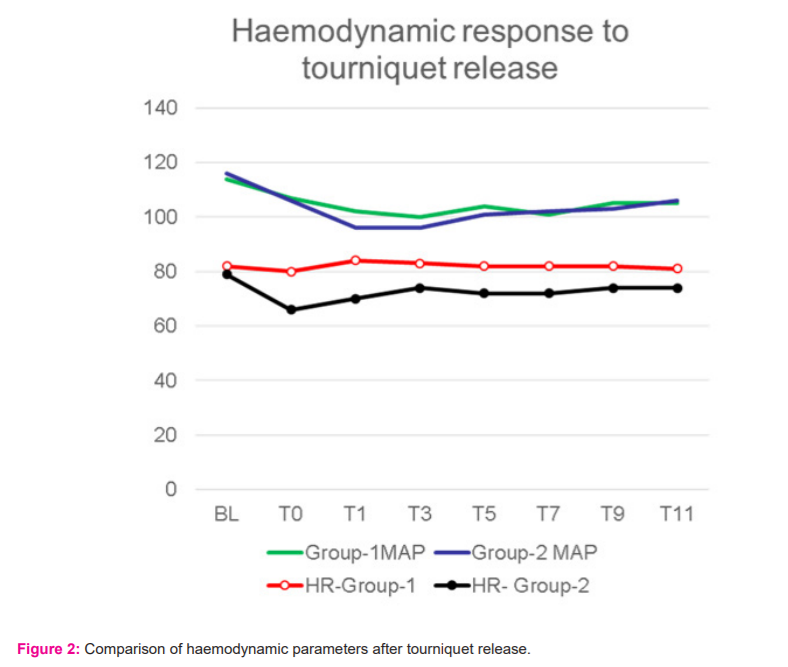
We observed the maximum increase in heart rate in group-1 and group-2 was in the range of 5% and 12% respectively compared to baseline, which was clinically insignificant. The mean values of vital parameters in both groups related to tourniquet release were clinically insignificant (Figure-2), which denote fluid therapy adequacy. The selection of colloid was always debatable for adverse effects on kidneys. However, studies have proven that in patients with normal renal parameters, the newer generation starch solutions are safe to use, 12,13 our selection of HES was part of institutional protocol and availability.
Inflation of tourniquet was done after exsanguination by elastic wrap followed by elevating the limb as an institutional protocol to minimize blood loss during the procedure. Usually, bilateral inflation of tourniquet in lower limbs expected to increase the circulating blood volume by 15%,14,15 however in our study group inflation of the tourniquet did not have any significant impact when compared with pre-inflation values. This substantiates the application of tourniquet in one limb in patients with adequate volume status has minimal impact on hemodynamic parameters. The duration of tourniquet inflation usually affects the hemodynamic stability during release, but in our study group, the course was uniform across the study group, leaving less evaluation scope.
Our study's limitation was that immediate blood loss post-tourniquet release was not taken into consideration, which could have affected the vitals, to add the haemodynamic change was not correlated with blood pH and postoperative hematocrit which could have given an added assessment.
CONCLUSION: Tourniquet release induced hypotension needs attention. Preloading with colloids before tourniquet release reduces overall hypotensive episodes. Pre-loading partially attenuates immediate haemodynamic instability after tourniquet release.
Conflict of Interest: NONE
Sources of support: There are no financial support or sponsorship.
Acknowledgement: Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors/editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
-
Tetro AM, Rudan JF. The effects of a pneumatic tourniquet on blood loss in total knee arthroplasty. Can J Surg. 2011; 44:33-8.
-
Pradeep Govil, P.N. Kakar, Atul Kishore Kapoor, Ankit Sharma, Deepak Govil, Deep Arora. Refractory Hypotension after Tourniquet Deflation in a Patient on Chronic Clomipramine Therapy. Indian J Anaesth. 2008; 52 (4):443-7.
-
Kewal Krishan Gupta, Amanjot Singh. Cardiac arrest following tourniquet release: Needs attention. Saudi J Anaesth. 2015 Oct-Dec; 9(4): 489–90.
-
Houng WR, Lee CL, Chiou HM, Wei YS. Cardiac arrest after tourniquet deflation in tibial plateau fracture surgery in a healthy man – a case report. Formosan J Musculoskel Disord. 2012; 3: 34-8.
-
Bharti N, Mahajan S. Massive pulmonary embolism leading to cardiac arrest after tourniquet deflation following lower limb surgery. Anaesth Intensive Care. 2009;37(5): 867-8.
-
Cohen JD, Keslin JS, Nili M, Yosipovitch Z, Gassner S. Massive pulmonary embolism and tourniquet deflation- a case report. Anesth Analg 1994;79: 583-5.
-
Satoh J, Arakawa J, Ohmori H, Takahashi H, Yamakage M, Namiki A. Intraoperative cardiac arrest due to coronary vasospasm after tourniquet release--a case report. Masui. 2006;55(4):460-3.
-
Inkyung Song, Dong Yeon Kim, Youn Jin Kim. The effect of tourniquet deflation on hemodynamics and regional cerebral oxygen saturation in aged patients undergoing total knee replacement surgery. Korean J Anesthesiol. 2012; 63(5): 425-30.
-
Mueen Ullah Khan, Abdul Saboor Memon, Mohammad Ishaq and Mansoor Aqil. Preload Versus Co-load and Vasopressor Requirement for the Prevention of Spinal Anesthesia Induced Hypotension in Non-Obstetric Patients. J Coll Physicians Surg Pak. 2015; 25(12): 851-5.
-
Iwama H, Kaneko T, Ohmizo H, Furuta H, Ohmori S, Watanabe K.Circulatory, respiratory and metabolic changes after thigh tourniquet release in combined epidural-propofol anaesthesia with preservation of spontaneous respiration. Anaesthes. 2002: 57: 584–605.
-
Karaca Omera, Gogus Nerminb, Ahiskalioglu Ali, Aksoy Mehmet, Dogus Unal, Kumas Solak Sezen et al. Tourniquet-induced ischaemia-reperfusion injury: the comparison of antioxidative effects of small-dose propofol and ketamine. Braz J Anesthesiol. 2017; 67(3):246-50.
-
Westphal M, James MF, Kozek-Langenecker S, Stocker R, Guidet B, Van Aken H. Hydroxyethyl starches. Different products – different effects. Anesthes. 2009; 111: 187-202.
-
James MFM. The role of tetrastarches for volume replacement in the perioperative setting. Curr Opin Anaesthesiol. 2008; 21: 674-8.
-
Estebe JP, Davies JM, Richebe P. The pneumatic tourniquet: Mechanical, ischaemia-reperfusion and systemic effects. Eur J Anaesthesiol. 2011;28:404-11.
-
Zaman SM, Islam MM, Chowdhury KK et al. Haemodynamic and end tidal CO2 changes state after inflation and deflation of pneumatic tourniquet on extremities. Mymensingh Med J. 2010;19:524-8.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License