IJCRR - 7(23), December, 2015
Pages: 08-13
Date of Publication: 10-Dec-2015
Print Article
Download XML Download PDF
CLINICAL STUDY ON THE PREVALANCE OFFUNGAL INFECTIONS IN DIABETIC FOOT ULCERS
Author: Abilash S., N.S. Kannan, K.V. Rajan, M. Pramodhini, M. Ramanathan
Category: Healthcare
Abstract:Introduction: Diabetic lower limb wounds account for one of the commonest forms of complications with diabetes. These ulcerated lesions are easily susceptible to infections. Several studies have concluded the presence of varied microbial flora associated with the wounds. The mycology of the lesion is not given equal importance when compared to its bacterial aspect. Recent studies have shown the presence of wide range of fungal strains present in an infected foot ulcer of a diabetic patient, with Candida species accounting for the most commonly isolated strain. Aim: This study was done in an attempt to study the prevalence and spectrum of fungal infection in diabetic foot ulcers and to compare our findings with those of previous studies. Methodology: This hospital based prospective study. A total number of 100 patients with diabetic foot ulcers were included in this study. Patients already treated with anti-fungal therapy, chemotherapy, immunosuppressant, radiotherapy and corticosteroids were excluded. Detailed history of all patients was taken. These patients were evaluated with reference to clinical symptomatology and biochemical profile for diabetes mellitus. Two tissue samples, which were taken from the bed of the diabetic foot ulcer from each patient, one for microscopic examination and the other for culture sensitivity both bacterial and fungal. The patients were treated with regular dressing and antifungal therapy in addition to appropriate antibiotics as per bacterial culture sensitivity. The results were compared with other studies in literature and discussed. Results: Out of the 100 patients, evaluated 18% had positive fungal cultures, among them most common fungal strain was C albicans and secondly was C tropicalis
Conclusion: Management of diabetic foot ulcers must include antifungal antibiotics as per fungal culture sensitivity report in addition to routine bacterial culture sensitivity and other modalities.
Keywords: Diabetic foot ulcer, Fungal infection, Culture and sensitivity, Antifungal antibiotics
Full Text:
INTRODUCTION
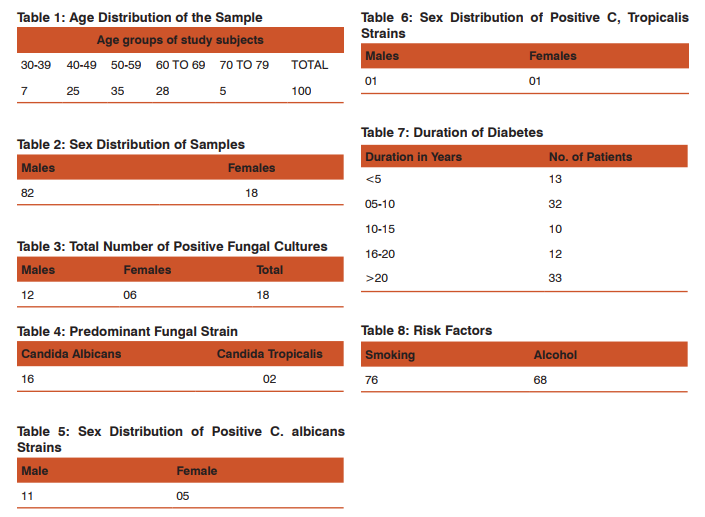
Diabetic lower limb wounds account for one of the commonest forms of complications with diabetes. These ulcerated lesions are easily susceptible to infections. Several studies have concluded the presence of varied microbial flora associated with the wounds. The microbiology associated with diabetic foot ulcers studied from samples taken from deep tissue bed is varied. In addition, several studied have shown the researched evidence of presence of both aerobic and anaerobic bacteria associated with the infections. Even though bacteriological infections associated with diabetic foot ulcers are given prime importance, the opportunistic fungal infections are ignored. The mycology of the lesion was not given equal importance in the past when compared to its bacterial aspect due to lack of literature. However, re cent studies have shown the presence of wide range of fungal strains in an infected foot ulcer of a diabetic patient, with Candida species accounting for the most commonly isolated strain. Ideal treatment of an infected diabetes foot ulcer should encompass all the possible microbiological causes, to provide efficient and specific treatment to the surgical patient. Aims and Objectives 1. To study the prevalence of fungal infection in diabetic foot ulcers. 2. To study the spectrum of fungal strains isolated from the wounds. 3. To compare our findings with those of previous studies. MATERIALS AND METHODS This hospital based prospective study was carried out in Mahatma Gandhi Medical College and Research institute, Pondicherry during the period February 2013 to June 2014. A total number of 100 cases were studied. The study was carried out after obtaining clearance from institutional human ethics committee. All patients with diabetic foot ulcers coming to our hospital were included in this study. Patients already treated with anti-fungal therapy, chemotherapy, immunosuppressants, radiotherapy and corticosteroids were excluded. After duly obtaining an informed consent, detailed history of all patients was taken. These patients were evaluated with reference to clinical symptomotology, biochemical profile for diabetes mellitus (FBS, PPBS and HbA1C) .Two tissue samples which were taken from the bed of the diabetic foot ulcer from each patient is put in a sterile container containing normal saline and is sent to the microbiology laboratory and Microscopic examination of collected tissues were done. One of the tissue bit is soaked in 10% KOH, the other tissue bit is used for fungal culture sensitivity with Sabourauds dextrose agar supplemented with chloramphenicol and cycloheximide, incubated at 30°C and 37°C for 4 weeks. The patients were treated with regular dressing, appropriate antibiotics according to bacterial culture sensitivity till the fungal culture reports. Antifungal therapy was started as per the culture sensitivity report. The data were tabulated in a master chart using MS EXCEL. The results were compared with other studies in literature and discussed. RESULTS Among the 100 patients, the youngest patient was a 31 year old and the eldest was a 72 year old. There were seven patients in the age group of 30-39 years, 25 patients in the age group of 40-49, 35 patients in the age group of 50-59, 28 patients in the age group of 60 to 69 and 5 patients in the age group of 70 to 79 (Table 1). The highest incidence was in the age group of 5th decade. There were total of 18 female and 82 male patients (Table 2). Among the 100 patients, 18 had positive fungal cultures-12 males and 6 females (Table 3). Among the 18 fungal cultures, Candida species of fungal isolates were predominant; specifically strains of Candida albicans-16 samples and Candida tropicalis-2 samples (Table 4). Sex distribution of patients positive for C. albicans strains is shown in Table 5. Sex distribution of patients positive for C. tropicalis strains is shown in Table 6. In all patients both the strains cultured were sensitive to Fluconazole. Among the 100 patients studied, 13 patients had type 2 diabetes mellitus for less than 5 years and 32 patients had diabetes mellitus for 5 – 10 years, 10 patients had diabetes for 10 – 15 years, 12 patients had diabetes mellitus for 16-20 years and 33 patients had diabetes mellitus for more than 20 years (Table 7). Among the 100 patients, 76 were smokers and 68 were alcoholics (Table 8).
DISCUSSION
According to International Diabetes Federation’s atlas, there are about 65.1 million people in India suffering from diabetes with an alarming mortality rate of 55%1 . Approximately a quarter of all people with diabetes will develop sores or ulcers at some point during their lifetime2 . Diabetic foot ulcers (DFU) are one of the most dreaded and common complications of diabetes, which is associated with lower limb amputation and account for majority of non-traumatic amputations conducted3 . This is also associated with high morbidity and substantial health care costs4 . According to the World Health Organization and the international working group on the diabetic foot, ‘Diabetic foot is defined as the foot of diabetic patients with ulceration, infection and/or destruction of deep tissues, associated with neurological abnormalities and various degrees of peripheral vascular diseases of the lower limb’. Aetiology though being multi factorial, peripheral neuropathy and ischemia are the major factors for DFU along with several other contributing risk factors5 . Diabetes is one of the most common causes of multifocal peripheral neuropathy, which further gives rise to diabetic foot ulcers. Neuropathy in diabetic patients is manifested in the motor, autonomic and sensory components of the nervous system5,6,7,8.
Based on epidemiological study by Dyck et al, 60% 0f DFUs occur due to underlying diabetic neuropathy7 . Ischemic ulcers without significant associated neuropathy accounts for 15 to 20% of foot ulcers, and another 15-20% have a mixed neuropathic-vascular causative factor. In people with diabetes, atherosclerosis is very common. Peripheral arterial disease is responsible for the initiation of foot ulcers in up to 50% of the cases making it one of the major causative factors8 . Diabetic foot is one of the most feared complications of diabetes, which may result in repeated hospitalizations leading to amputations. It is common affecting up to 30% of Indian patients with diabetes in their lifetime9 . Another study conducted by Shahi et al in northern India claim that the prevalence of DFUs in patients with diabetes was 14.30%10. Diabetic foot ulcers associated infections are the most common cause of amputation. According to a multicenter study from India, conducted to determine the pattern and causes of amputation in diabetic patients from a sample size of 1985, 90% of the amputations were due to infection arising in the diabetic foot11. Diabetic foot lesions are responsible for more hospitalizations than any other complications of diabetes, increasing the burden on health care infrastructure and the cost of care. Among patients with diabetes, roughly about 15% develop a foot ulcer. Diabetes is the major cause of non-traumatic lower extremity amputation in our country and across the world. Foot infections in diabetic patients usually begin in skin ulceration. Most infections remain superficial, but 25% will spread contiguously from the skin to deeper subcutaneous tissues and/or bone. An infected foot ulcer precedes 60% of amputations, making infection perhaps the most important proximate cause of this tragic outcome. Because all skin wounds contain microorganisms, infection must be diagnosed clinically, that is, by the presence of systemic signs (e.g., fever, chills, and leukocytosis), purulent secretions (pus), or local classical signs or symptoms of inflammation (warmth, redness, pain or tenderness, and induration). In chronic wounds, additional signs suggesting infection may include delayed healing, abnormal coloration, friability, or foul odour12. Pathare et al13 in their ‘Microbiology of diabetic foot: Indian studies’, analysed 775 diabetic foot patients and found the infections are Polymicrobial. Averages of 3.07 organisms were isolated per case, 71.09% aerobic and 28.91% anaerobic. The fungal infection is difficult to diagnose and is a serious cause of morbidity or mortality in diabetes8 . Fungal infection among immuno-compromised patients is now a global major health concern, but the species of fungi infecting diabetic foot infections and its pathogenicity has not yet been researched thoroughly. As a result, clinicians and surgeons treating diabetic foot wounds suspect only the bacterial infections and prescribe accordingly. The deep tissue from the wound bed is not usually sent for fungal culture and sensitivity, either due to lack of literature substantiation or due to the belief that there would not be any fungal infections in the diabetic foot ulcers as they are rare occurrences. In the study conducted in India by Chellan et al14, enrolled 518 patients, among whom 382 were males and 136 females with type 2 diabetes admitted due to infections in the lowerlimb wounds. Samples from the ulcer bed of approximately 0.5 - 0.5 cm size were taken from the wound bed and cultured for fungi. Fungi were found in 27.2% (141/518) of the study population. Candida parapsilosis (25.5%), Candida tropicalis (22.7%), Trichosporonasahii (12.8%), Candida albicans (10.6%), and Aspergillus species (5.0%) were the most predominant fungal isolates. In a study by Chincholikar et al15,swabs were collected from 105 diabetic foot ulcer patients, which revealed that the fungal isolates accounted for 20.8%. Among this yeasts were predominant accounting for 94.55% and moulds comprised 5.46%. Candida tropicalis [54.55%] were most common followed by candida albicans [12.73%] among the yeasts. A study by Bansal et al16 in government medical college and hospital, Chandigarh demonstrated polymicrobial infection in 35% of the patients. In this, Pseudomonas aeruginosa [22%] and Staphylococcus aureus [19%] were predominantly isolated. Among fungal isolates candida species were most predominantly isolated. Subha et al17 conducted a study in Mysore Karnataka on 120 patients with diabetic foot infections and found that 66.66% of the isolates indicated candida sp. Yet another study was carried out by Nair S et al18 to assess the incidence of mycotic pathogens in diabetic foot ulcers. A total of 74 Type II diabetic patients with non-healing diabetic foot infections were recruited for the study. Among the diabetic patients, 65 % had yeast and mold infections. Pathogenic yeasts were noted in 77 % of the patients of which Candida species was predominant (93 %). The major Candida species isolated were C. albicans (49 %), C. tropicalis (23 %), C. parapsilosis (18 %), C. guillermondi (5 %) and C. krusei (5 %). The other yeast species isolated were Trichosporon cutaneum and T. capitatum. Trichophyton spp. was the only dermatophytic fungus found. Molds were isolated from 38 % of the infected patients of which Aspergillus species predominated (72 %). The other molds isolated were Fusarium solani, Penicillium marneffei and Basidiobolus ranarum. The duration of diabetes also plays a role in the formation of ulcer and the incidence of lower extremity amputation was more in patients who have diabetes for more than 5 years. Longer the duration of diabetes, higher are the chances of developing a non-healing ulcer. Mehamud et al19 reported that out of 120 patients, majority of patients who underwent amputation had diabetes more than 10 years (p<0.05). Among our patients, 13% had diabetes for less than 5 years, 32% of them had from 5 to 10 years, 10% had from 11 to 15, 12% had from 16 to 20 years, and 33% had for more than 20 years. The incidence of diabetic foot increases with increasing age20,21,22,24,25. . The youngest patient in our study was 31 years old and the oldest was 72 years of age. The peak age incidence of diabetic foot ulcer in our study was in the 5th decade. Many studies revealed that the mean age group was in the 6th and 7th decade. We found that the incidence of diabetic foot ulcers was higher in males, when compared to females. Even though it was not statistically significant, most authors agree that the males are at higher risk to develop foot ulcers. This may be explained, as males are at a higher risk for trauma to feet. In our study, 76% were smokers and 68% were alcoholics. Smoking and alcohol consumption were linked to higher incidence of foot ulcers in diabetics, and was a statistically significant risk factor for amputation in patients with diabetic foot ulcers. This could be attributed to vasculopathic effects of tobacco smoking. Alcohol consumption is known to increase risk of making the patients prone to trauma. Risk factors such as smoking and consumption of alcohol, favour poor wound healing. Many studies have indicated these factors as risk factors for poor wound healing and amputation. The risk of foot ulceration and limb amputation in people with diabetes is lessened by patient education stressing the importance of routine preventive podiatric care, appropriate shoes, avoidance of cigarette smoking, and control of hyperlipidemia and adequate glycemic control26,27,28,29. Risk factors associated with adverse outcomes in a population based prospective cohort study of people with their first diabetic foot ulcer by Winkley et al28 of UK explained the variables which were age, male gender, smoking, ulcer site, size, severity of neuropathy, ischemia and presence of vascular complications. Microvascular complications were the only explanation for recurrent ulceration. In our study, of all the 100 samples sent for microbiological examination only 18 samples were found to be positive for fungal strains, which are lower than a similar study, which was conducted in India by Chellan et al14, which reported positive Fungal isolates in 27.2% of the total number of samples. The same study reported that the most predominant fungal species, which was isolated, was found to be Candida species, which coincides with our study. The most common Candida species was found to be C albicans [88.8%] followed by C tropicalis [11.11%] of the total fungal isolates substantiated by a study conducted by Nair S et al18 to assess the incidence of mycotic pathogens in diabetic foot ulcers. Summary of our study being: 1. In our study foot ulcers were more among patients in the 5th decade. 2. Diabetic foot ulcers were more common among males. 3. Duration of diabetes as more than 5 years in majority of the patients. 4. Among the 100, 76 % were smokers and 68% alcoholics. 5. Most common fungal strains found were C albicans and C tropicalis.
CONCLUSIONS
Management of diabetic foot ulcers must include antifungal antibiotics as per fungal culture sensitivity report in addition to routine bacterial culture sensitivity and other modalities. This study may not reflect all the aspects of management of diabetic foot ulcers, further , the study was among a small group of 100 patients in a short period . A larger study spanning over longer period and a bigger sample size is required to draw definitive conclusions.
ACKNOWLEDGEMENT
Authors duly thank the department of general surgery, Mahatma Gandhi Medical College and Research institute and Sri Balaji Vidyapeeth University, for permitting us to publish the contents of PG Dissertation of Dr. Abilash.S as an article in IJCRR. Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
Source of funding:
Nil.
Conflict of interest:
All authors declare that there is no conflict of interest.
References:
1. IDF Diabetes Atlas Sixth Edition, International Diabetes Federation 2013.
2. Reiber, G., Lipsky, B., and Gibbons, G.The burden of diabetic foot ulcers. The American Journal of Surgery, 1998;176(2):5S– 10S.
3. The Diabetic Foot: Epidomology, Risk Factors And The Status Of Care; The Global Impact;Andrew Boulton, Diabetes Voice, November 2005;(50), Special Issue
4. Bowering CK Diabetic foot ulcers. Pathophysiology, assessment, and therapy. Can Fam Physician. 2001 May;47:1007-16.
5. Crawford F, Inkster M, Kleijnen J, Fahey T. Predicting foot ulcers in patients with diabetes: a systematic review and metaanalysis QJM. 2007 Feb;100(2):65-86.
6. Gerassimidis T, Karkos CD, Karamanos D, Kamparoudis A Current endovascular management of the ischaemic diabetic foot. Hippokratia. 2008 Apr;12(2):67-73.
7. Dyck PJ, Clark VM, Overland CJ, et al. Impaired glycemia and diabetic polyneuropathy: the OC IG Survey. Diabetes Care. 2012;35:584–91.
8. Clayton Jr, W., and Elasy, T. A. A review of the pathophysiology, classification, and treatment of foot ulcers in diabetic patients. Clinical diabetes, 2009;27(2):52.
9. Sunil Gupta, Management Of Diabetic Foot, Medicine Update 2012;22:287-93.
10. Shahi, S. K., Kumar, A., Kumar, S., and Singh, S. K.. Gupta S K, Singh T.B. Prevalence of Diabetic Foot Ulcer and Associated Risk Factors in Diabetic Patients From North India.. The Journal of Diabetic Foot Complications, 2012;4(3):83-91.
11. Viswanathan V. Epidemiology of diabetic foot and management of foot problems in India. Int J Low Extrem Wounds. 2010 Sep;9(3):122-6.
12. Lipsky BA, Berendt AR, Deery HG, Embil JM, Joseph WS, Karchmer AW et al. Diagnosis and treatment of diabetic foot infections.Clin Infect Dis. 2004;39 (7):885-910.
13. Pathare NA, Bal A, Talvalkar GV, Antani DU. Diabetic foot infections: a study of microorganisms associated with the different Wagner grades. Indian J Pathol Microbiol 1998;41:437-41.
14. Chellan G, Shivprakash S, Karimassery Ramaiyar S, Varma AK, Varma N, Thekkeparambil Sukumaran M, et al. Spectrum and prevalence of fungi infecting deep tissues of lower-limb wounds in patients with type 2 diabetes. J Clin Microbiol. 2010;48:2097– 102.
15. Cincholikar DA, Pal R B. Study of fungal and bacterial infections of the diabetic foot. Indian journal of pathology and microbiology, 2002;45(1):15-22.
16. Bansal E, Garg A, Bhatia S, Attri, A K, Chander J. Spectrum of microbial flora in diabetic foot ulcers. Indian journal of pathology and microbiology, 2008;51(2):204-8.
17. Subha KS, Isolation and Identification of Pathogens from Diabetic Foot Infections from K.R. Hospital, Mysore, Indian Journal Of Developmental Research, 2013;3(5).
18. Nair S, Peter S, Sasidharan A, Sistla S, Unni A K K. Incidence Of Mycotic Infections In Diabetic Foot Tissue, Journal of culture collections. 2006-2007;(5):85-89.
19. Mehmood K, Akhtar ST, Talib A, Talib A, Abbasi B, Siraj-UlSalekeen et al. Clinical profile and management outcome of diabetic foot ulcers in a tertiary care hospital. J. Coll. Physicians Surg. Pak. 2008;18(7):408-12.
20. Al-Maskari F, El-Sadig M. Prevalence of risk factors for diabetic foot complications. BMC Fam Pract. 2007;8:59.
21. Al-Tawfiq JA , Johndrow JA, Presentation And Outcome Of Diabetic Foot Ulcers In Saudi Arabian Patients. Adv. Skin Wound Care 2009;22(3):199-121.
22. Alwakeel, J. S., Al-Suwaida, A., Isnani, A. C., Al-Harbi, A., and Alam, A. (2009). Concomitant macro and microvascular complications in diabetic nephropathy. Saudi Journal Of Kidney Dis. Transpl. 2009;20(3):402-09.
23. Imran, S., Ali, R., and Mahboob, G. (2006). Frequency of lower extremity amputation in diabetics with reference to glycemic control and Wagner’s grades. J. Coll, Physicians Surg. Pak. 2006;16(2):124-7.
24. Unnikrishnan, A. G An approach to a patient with a diabetic foot.(vol 21, pg 134, National Medical Journal Of India 2008;21(4):201.
25. Tajunisah, I., Nabilah, H., and Reddy, S. C. (2006). Prevalence and risk factors for diabetic retinopathy--a study of 217 patients from University of Malaya Medical Centre. The Medical journal of Malaysia, Med. Journal Of Malaysia 2006;61(4):451-456.
26. Moss SE, Klein R, Klein BE The 14-year incidence of lowerextremity amputations in a diabetic population. The Wisconsin Epidemiologic Study of Diabetic Retinopathy. Diabetes Care. 1999;22(6):951-9.
27. Nather A, Bee CS, Huak CY, Chew JL, Lin CB, Neo S, et al. Epidemiology of diabetic foot problems and predictive factors for limb loss. J Diabetes Complications. 2008;22(2):77-82.
28. Winkley K, Stahl D, Chalder T, Edmonds ME, Ismail K. Risk factors associated with adverse outcomes in a population-based prospective cohort study of people with their first diabetic foot ulcer. J Diabetes Complications. 2007;21(6):341–349.
29. Chaturvedi N, Abbott CA, Whalley A, Widdows P, Leggetter SY, Boulton AJ. Risk of diabetes-related amputation in South Asians vs. Europeans in the UK. Diabet Med. 2002;19(2):99- 104.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License