IJCRR - 2nd Wave of COVID-19: Role of Social Awareness, Health and Technology Sector, June, 2021
Pages: 81-85
Date of Publication: 11-Jun-2021
Print Article
Download XML Download PDF
Effet of COVID-19 Pandemic on the Diagnosis of Breast Lesions Compared with Breast Lesions in the Previous Five Years
Author: Rohi Wani, Sheema Sheikh, Josepheen Shahmiri, Abdul Maajed Jehangeer, Misbah Rashid, Salma Gull
Category: Healthcare
Abstract:Background: Covid-19 pandemic caused havoc in both people, the health care system and more so in patients with malignancies. Breast malignancies being one of the most common and relatively curable malignancies got hit a lot due to the impact of the Covid-19 pandemic. The multistep impact of pandemic delayed the diagnosis as also the treatment of this multidisciplinary approach disease. Objective: To determine the effect of the Covid-19 pandemic on the diagnosis of breast lesions. Methods: This is a descriptive type of histopathological study in which we have collected and studied the data of Breast lesions over the Five years (Jan 2015-Dec 2019) and compared it with the data of Breast lesions in the Covid-19 year (the year 2020). Results: The number of cases of breast specimens received for histopathology per year declined from an average of 224/year to 124/year in the Covid-19 year of 2020. Conclusion: The decrease in the number of cases alludes to the downfall in the number of patients coming for diagnosis and in turn getting treatment. This study also highlights the importance of anticipation of various cases which will cluster shortly.
Keywords: Breast Carcinoma, Covid-19, Pandemic
Full Text:
INTRODUCTION
As the Covid-19 started in Wuhan in early January 2020, significant disruptions occurred in the health care system. This pandemic has hit all the aspects of our life and among the malignancies, it has hit Breast carcinoma badly, not only by hampering both its primary and secondary prevention but also its treatment.1 Breast Carcinoma is the most common and feared malignancy of women globally, with 1.7 million women getting diagnosed every year with this disease and it kills one patient out of the three.1 It stands second in the list of frequently occurring newly diagnosed cancers worldwide. It is estimated that nearly 70% of malignant tumours are caused by environmental factors, whereas in breast cancer this percentage reaches 90–95%.2
The breast although being an accessory organ is quite vital in terms of its varied pathologies and more importantly its accessibility to diagnostic procedures and potential of cure to its various life-threatening diseases. Most of the breast lesions turn out to be benign, however, the malignancies are nonetheless quite common. Diagnosis of breast lesions occurs usually by palpation in younger age groups and by screening mammographic procedures in the elderly. Covid 19 Pandemic has affected every aspect of this deadly disease with a potential cure, whether it's self-examination, an appointment with a doctor, clinical facility accessible to the patients and ultimately the treatment also. 3-6
Breast Carcinoma is the most common malignancy of women worldwide (except for non-melanoma skin carcinoma) and causes the majority of cancer deaths in women. Breast stands out most of the organs of the body in terms of its commonality of lesions, both benign and malignant, the convenience of self-examination, accessibility to diagnostic workup, better prognosis, and better cure rates.3,4
This article summarises the comparative data-driven impact on breast surgeries in the Covid-19 year 2020 and thus the diagnosis of breast lesions. We are presenting the data of breast lesions over the last five years in addition to the data of the last year of covid 19 the pandemic year 2020.
MATERIAL AND METHODS
All the breast specimens submitted for histopathological examination over six years were studied which is from Jan 2015-Dec 2020 including the specimens of the Covid-19 year 2020. It is a descriptive and retrospective type of study. All the breast cases which included Lumpectomy, Excision biopsies, Tru cut biopsies, Mastectomy specimens and Blocks for Review were included in the study irrespective of age and sex. There were no exclusion criteria. Only the specimens which had the pure diagnosis of dermal pathology were excluded. Specimens were received in 10% formalin and were subjected to routine Hematoxylin and Eosin stains.
All the sections were studied in detail, clinical history was noted down and the morphological diagnosis was made. Cases were clustered as those of the previous five years (2015-2020) of the non-Covid period and those of the Covid era which is the year 2020. The data was tabulated as benign and malignant lesions. The average number of cases from the previous Five year period was calculated and compared to Covid 2020 year. The total number of cases received in the departments every year for all Six years was calculated. Necessary details and variations in histopathology were noted down.
RESULTS
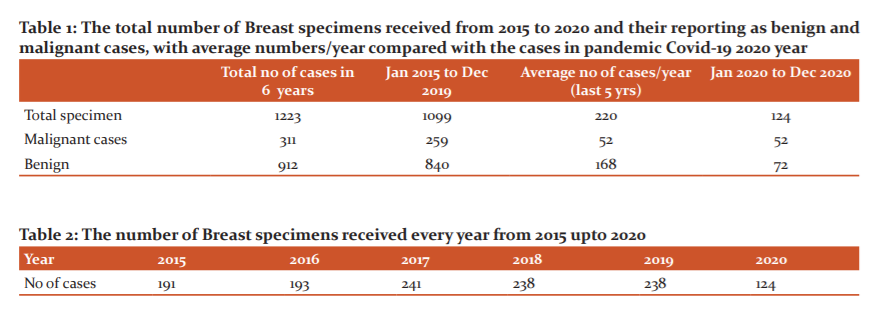
The total number of breast specimens received in our department in the last six years was 1223. Out of these total of 1099 breast specimens were received in the last five years from Jan 2015 to Dec 2019 with an average of 220 specimens in a year, whereas in the last year of the Covid 19 pandemic a total of only 124 specimens were received in our department. Among the total of 311 malignant specimens received in the last six years, 259 were received in the previous five years making an average of 52 (259/5) malignancies of breast reported per year. Interestingly we have reported a total of exactly 52 malignancies of the breast in the Covid 19 pandemic year (the year 2020). Among the benign breast cases were the total of 912 reports in all the six years, of which 840 were reported in the previous 5 years with an average of 168 (840/5) benign reports per year and an alarming number of only 72 benign reports in the Covid Pandemic year-2020year (Table 1).
When we compare the data of all the Six years individually (Table 2), we can make out that we received a total of 191 Breast specimens in 2015, 193 in the year 2016, 241 in the year 2017, 238 in the year 2018, 238 in the year 2019 and only 124 in the year 2020. As our data suggest that the most significant impact of the Covid-19 pandemic was on the benign breast lesions, which dumped down from an average of 168 cases per year to less than its half, and turned out to be only 72 cases in Covid-19 year, directly alluding to the impact of Covid -19 on the decreased number of surgeries performed on breast and in turn to the exponential decrease in the number of patients amenable to the medical amenities in the menace of Covid-19 (Table 1). Such an impact of the pandemic on this organ is quite distressing for such a disease which is accessible, amenable and even curable.
The total number of cases received in our department decreased to just 124 cases in the year 2020 from 238 cases of the year 2019, decreasing to almost half (Table 2). The decrease in the number of specimens occurred even though in addition to the routine breast specimens operated in our tertiary care, most of the surgeries done in the local surgical centres who used to sent these cases previously to the distant pathology labs landed in our department for histopathology, due travel restrictions.
DISCUSSION
There was a block at multiple levels for the diagnosis of this disease. It was not only multidisciplinary care algorithms that forced patients into delaying care but patients also self-selected to delay care. Almost 4 out of 10 patients revealed that the economic changes from the pandemic affected their ability to pay for medical care.3 Another survey by ACEP showed that almost one-third of patients (29%) delayed or avoided going to the medical facilities just to avoid COVID-19 exposures. And out of every Five patients Four were fearful of contracting the virus from a patient or health care worker if they did go. More than 81% of participants acknowledged practising social distancing.4,5 An Italian study, during the height of the outbreak, showed a significant increase in patients refusing to undergo diagnostic appointments and breast biopsies at a major cancer centre.5 In another study of 600 patients, almost four-fifth stated they had routine and follow up appointments delayed, two-thirds had reconstruction surgery delayed, and almost two-third had delayed diagnostic imaging. Therapies that require in-person visits to the hospital (radiation, chemotherapy infusion, and surgical lumpectomies) were more likely to be delayed than those that could be obtained through telehealth appointments or a prescription pick-up. On average, about 30% of patients experienced delays in the mainstays of breast cancer treatment including lumpectomies, radiation therapy, and chemotherapy.6
A survey conducted by Radiology reported that 97.4% of 228 radiology practices (urban, academic, and rural) experienced declines in imaging volume in March/April 2020, with a drop of greater than 90% of elective procedures and 60% of urgent procedures.7
A multidisciplinary group survey done by the European Breast Cancer Research Association of Surgical Trialists was distributed by breast cancer societies to 377 breast cancers in 41 countries. It was seen that the estimated time interval between the diagnosis and treatment initiation increased to almost 20% of institutions. There was a modification in 56% of cases for primary systemic therapy, with upfront surgery increasing from 33.7% to 42.2% and 39.8% to 50.7% in ER-negative/HER2-positive and T1cN0 triple-negative cases, respectively. Chemotherapy was considered as an increased risk for developing COVID-19 complications by 67% of responders and 51% reported modification in chemotherapy protocols. A large majority (68%) recommended endocrine treatment to postpone surgery in patients with luminal-A tumours. Even postoperative radiation therapy was postponed in 20% of cases. Thus breast cancer management was considerably modified during the COVID-19 pandemic.8,9
The full understanding of the implications of the delay in diagnosis and access to treatment of breast cancer cannot be done unless it is contextualised to the biology of this cancer itself and the patterns of clinical presentation, for example, the stage of the disease and the setting of care. Every patient presenting with a new breast lump that is highly suspicious of malignancy or the one who has already undergone a screening procedure with image findings highly suspicious for malignancy should be promptly referred for tissue diagnosis and/or imaging and should be designated as a high priority. So based on clinical and pathological criteria, priority must be given to the undeferrable cases in a multidisciplinary assessment. Histopathology diagnosis can have an immediate impact. For some, as with patients of symptomatic metastatic relapse, whenever the provision of treatment can be simply life-saving and/or can significantly modify the quality of life, a histopathology diagnosis should be simply included in a set of undeferrable health services.10
Pacino et al. stated very vividly that It is extremely important to maintain breast disease awareness and guarantee a safe health infrastructure of awareness for both the patients as well as the health workers.11 Assessing the data-driven delay in diagnosis we can make out approximately the burden of disease in the community which could not communicate to the medical centres. As of now when the vaccination has already started and we have been able to control the Covid-19 to some extent, we have to anticipate the number of cases that will increase to show up.12
This pandemic has led to a bid and sudden disruption in routine medical care, as also the treatment of cancer patient which is an especially vulnerable group, as here the outcome is strictly dependent on timely and high-quality multidisciplinary interventions. To add insult to the injury are the travel restriction which has made it difficult for some cancer patients to reach the hospital.13
Citgez et al. in their review in a Turkish hospital explained some changes in the approach to breast cancer and emphasized the tailored therapy must be our first goal individually. Breast cancer treatment requires a multidisciplinary approach. Dynamic changing of local conditions may affect the priority levels and treatment options. Patient treatment decisions should be made by thinking about both during and after the pandemic management of healthcare systems. Social distancing and precautionary measures are still in effect. More recently, regions with low rates of infection are planning to gradually reopen their economies and begin lifting some of these measures. Unfortunately, remaining at home may be difficult for patients among us with severe medical conditions that require urgent attention, but COVID-19 impacts everything, including how we manage breast cancer.14
As the experts in Italy rightly said that in the coming future we will see and assist in a shift toward a clinical presentation of more advanced breast cancer which could impair the oncological outcome, worsen the quality of life due to more invasive surgery, chemotherapy radiotherapy, and also increase the relative cost for the Public Health System. To organize our departments and hospitals as efficient as possible and to be ready to restart, epidemiological studies could be useful tools to evaluate the impact of screening programs to prevent a setback to where we were 20 years ago when a 2 cm lesion was considered an early diagnosis of breast cancer.15
One modelling study of 6281 new stage 1 to 3 cancer cases in the United Kingdom who were delayed multidisciplinary workup during the covid-19 pandemic suggested that an additional 181 lives and 3316 life years would be lost with a conservative estimate of only 25% of cases backlogged for 2 months.16 Just in the early phases of the pandemic, the number of new cancers diagnosed decreased.17,18 This drop was likely secondary to patients not presenting for care and not a true drop-in incidence. Thus, these cancers will come to the radar eventually at greater size or stage than they would have with earlier detection, which may affect prognosis. A model that assumed only a 6-month disruption of care during the pandemic estimated the potential excess deaths from breast and colorectal cancer secondary to the Covid-19 pandemic disruptions in care simply demonstrates an excess of more than 10,000 deaths in the next decade, peaking in the first few years.19
Analysis from a study in the UK suggests that the number of breast cancers diagnosed during the first half of 2020 is not as low as initially feared, and a substantial proportion of the shortfall can be explained by the suspension of routine screening in March 2020, thus underscoring the importance of the very first step of routine screening in this organ.20
CONCLUSION
We all need to gear up for the extra burden of this disease which is unaccounted for but highly anticipated for in this very common but curable disease. We all should have consensus guidelines to guide fair decision-making and developing empathic communication about these issues. Also, the effects of limiting care during this pandemic, and potentially in future crises, on both cancer specialists and patients should be carefully managed.
ACKNOWLEDGEMENTS: All the authors of this study have contributed to the scientific content and/or providing technical support. Further authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors/editors/publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
Source of Funding: Nil
Conflict of Interest: Nil
References:
-
Kumar V, Abbas AK, Aster JC, Turner JR. Robbins & Cotran Pathologic basis of disease. 10th ed. Elsevier: Elsevier Health Science; 2021.
-
Kolak A, Kami?ska M, Sygit K, Budny A, Surdyka D, Kukie?ka-Budny B, et al. Primary and secondary prevention of breast cancer. Ann Agric Environ Med. 2017;24(4): 549–553.
-
Printz C. When a global pandemic complicates cancer care: Although oncologists and their patients are accustomed to fighting tough battles against a lethal disease, Coronavirus Disease 2019 (COVID-19) has posed an unprecedented challenge. Cancer. 2020;126(14):3171–3173.
-
American College of Emergency Physicians COVID-19. 2020. Available at: https://www. emergencyphysicians.org/globalassets/emphysicia ns/all-pdfs/acep-mc-COVID19-april-poll-analysis.pdf. Accessed September 8, 2020.
-
Vanni G, Materazzo M, Pellicciaro M. Breast Cancer and COVID-19: The Effect of Fear on Patients’ Decision-making Process. Ann Agric Environ Med. 2020;34(3 Suppl):1651–1659.
-
Papautsky EL, Hamlish T. Patient-reported treatment delays in breast cancer care during the COVID-19 pandemic. Breast Cancer Res Treat. 2020:1-6.
-
Malhotra A, Wu X, Fleishon HB, DuszakJr R, Silvia E, Bender C, et al. Initial Impact of Coronavirus Disease 2019 (COVID-19) on Radiology Practices: An ACR/RBMA Survey. J Am Coll Radiol. 2020;17:1525-1531.
-
Gasparri ML, Gentilini OD, Lueftner D, Thorsten Kuehn, Kaidar-Person O, et al. Changes in breast cancer management during the Corona Virus Disease 19 pandemic: An international survey of the European Breast Cancer Research Association of Surgical Trialists (EUBREAST). The Breast. 2020;52:110-115.
-
Tsang-Wright F, Tasoulis MK, Roche N, MacNeill F. Breast cancer surgery after the COVID-19 pandemic. Future Oncol. 2020;16(33):2687-2690.
-
de Azambuja E, Trapani D, Loibl S, Delaloge S, Senkus E, et al. Management and treatment adapted recommendations in the COVID-19 era. Breast Cancer. ESMO Open 2020;5:e000793.
-
Pacino FAC, Ruiz CA, Sorpreso ICE, Costa AMM, Soares-Junior JM, et al. Management of benign and suspicious breast lesions during the coronavirus disease pandemic: recommendations for triage and treatment. Clinics. 2020;75:e2097.
-
Editorial. COVID-19: global consequences for oncology. Lancet Oncol. 2020;21(4):467.
-
Curigliano G, Cardoso MJ, Poortmans P, Gentilini O, Pravettoni G, et al. Recommendations for triage, prioritization and treatment of breast cancer patients during the COVID-19 pandemic. Breast. 2020;52:8-16.
-
Citgez B, Yigit B, Capkinoglu E, Yetkin GS. Management of Breast Cancer during the COVID-19 Pandemic. Med Bull Sisli Etfal Hosp. 2020;54(2):132–135.
-
Vanni G, Pellicciaro M, Materazzo M, Palombi L and Buonomo OC. Breast Cancer Diagnosis in Coronavirus-Era: Alert From Italy. Front Oncol 2020;10: 938.
-
Sud A, Torr B, Jones M, Broggio J, Scott S, Loveday C, et al. Effect of delays in the 2-week-wait cancer referral pathway during theCOVID-19 pandemic on cancer survival in the UK: a modelling study. Lancet Oncol. 2020;21(8):1035-1044.
-
IJzerman M, Emery J. Is a delayed cancer diagnosis a consequence of COVID-19?. 2020? Available at https://pursuit.unimelb.edu.au/articles/is-a-delayedcancer- diagnosis-a-consequence-of-covid-19. Accessed September 9, 2020
-
Kaufman HW, Chen Z, Niles J and Fesko Y. Changes in the Number of US Patients With Newly Identified Cancer Before and During the Coronavirus Disease 2019 (COVID-19) Pandemic. J Ame Med Ass 2020; 3(8)e2017267.
-
Sharpless NE. COVID-19 and cancer. Science 2020;368(6497):1290.
-
Gathani T, Clayton G, Macinnes E and Horgan K. The COVID-19 pandemic and impact on breast cancer diagnoses: what happened in England in the first half of 2020. Brit J Cancer. 2021;124:710–712;
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License