IJCRR - 13(11), June, 2021
Pages: 146-152
Date of Publication: 04-Jun-2021
Print Article
Download XML Download PDF
Study of Lipid Profile, Atherogenic Indices and Carotid Intima-Media Thickness as Predictors of Cardiovascular Disease in Individuals with Prediabetes
Author: Mukesh Kumar Shrewastwa, Viyatprajna Acharya, Subhashree Ray
Category: Healthcare
Abstract:Background: Prediabetes is the forerunner of diabetes mellitus (DM) which is the harbinger of cardiovascular disease because of the covert change in biochemical parameters in the prediabetes state. Atherogenic indices have been utilized for evaluation of the possibility for cardiovascular disease advancement. This study was taken up to estimate the correlation between atherogenic indices, such as cardiac risk ratio (CRR), atherogenic coefficient (AC), and atherogenic index of plasma (AIP) with cardiovascular parameters in the pre-diabetic stage. Objectives: This study was taken up to analyze atherogenic indices (CRR, AC, and AIP) against CIMT (carotid intima-media thickness), which is a surrogate marker in cardiovascular diseases, in prediabetic individuals and find out the correlation between them. Methods: In this cross-sectional study, a total of 120 human individuals were taken among whom 60 were prediabetic individuals and 60 were healthy individuals who served as control. Atherogenic indices were estimated from routine lipid profile parameters and carotid intima-media thickness (CIMT) was determined by ultrasonography in all subjects. Results: There was a significant increase in atherogenic indices, that is, CRR(P< 0.001), AC(P< 0.001), and AIP(P< 0.001), HbA1c(P< 0.001) and CIMT(P< 0.001) in prediabetic individuals as compared to controls and the CIMT was significantly positively correlated with atherogenic indices, that is, CRR(r=0.514,p< 0.01), AC(r=0.514,p< 0.01), and AIP(r=0.538,p< 0.01) respectively in the prediabetic group. Conclusion: Atherogenic indices may be utilized along with routine lipid parameters for the better evaluation of subclinical atherosclerosis in prediabetic individuals because these indices are inexpensive, non-invasive and can be determined from routine lipid parameters.
Keywords: Atherogenic indices, Atherogenic coefficient (AC), Atherogenic index of plasma (AIP), Carotid intima-media thickness (CIMT), Cardiac Risk Ratio (CRR), Small dense LDL-C (SdLDL-C)
Full Text:
Introduction
Diabetes Mellitus is one of the modern epidemics and as per International Diabetes Federation (IDF), the incidence of Type 2 (T2DM) will rise from 366 million in 2011 to 552 million by 2030, affecting one out of ten adults.1 In Europe, at least 131 billion dollars per year is spent on healthcare due to diabetes.2 A similar trend exists in South East Asian countries especially India, Nepal etc. The prevalence of DM will become double in people living in the urban area of developing countries in 2030 as compared to the year 2000 3. Prediabetic stage of diabetes is a longer phase, which is contemplated to be the harbinger and high-risk state for diabetes.4
Prediabetes can be defined as FBS in the range of 100-125 mg/dl.5,6 IFG and IGT constitute separate pathophysiological and biochemical and combinedly clinically known as “Prediabetes”.7,8 IDF evaluated that the worldwide prevalence of prediabetes was 318 million in the year 2015 and is forecasted to reach 482 million by the year 20409 and the same for Nepal was 10.3% in 2017.10 Prevalence of pre-diabetes: diabetes in Nepal is 19.5: 9.5%.11 Many studies have shown pro-atherogenic lipid profile in prediabetes leading to cardiovascular disease (CVD).12-14 Certain atherogenic indices have been formulated which can interlink the metabolic derangement of lipid fractions to clinical findings.15 The cardiac risk ratio (CRR)16, atherogenic coefficient (AC) which is Non-HDL-C: HDL-C correlates better than only LDL-C.17 Atherogenic index of plasma (AIP) is the logarithmic transformation of the curves that are created by dividing plasma triglyceride (TG) levels by the HDL-C levels and is a better risk predictor for CVD.18
Carotid intima-media thickness (CIMT) indicates subclinical atherosclerosis and there is an increase in intima-media thickness (IMT) of both the coronary vascular bed and the peripheral arteries.19-21 CIMT is determined through measurement of the thickness of the common carotid artery by ultrasound and has been demonstrated as an independent predictor of cardiovascular risk.22 The study targeted to correlate lipid profile, atherogenic indices: CRR, AC and AIP and CIMT that may be an early marker of atherosclerosis in prediabetic subjects.
Material and methods
A cross-sectional observational study was planned in the department of Biochemistry, Nepalgunj Medical College, Kohalpur, Nepal. In this study, a total of 120 human individuals were included among which 60 were prediabetic individuals in 18–55 years old of either gender and 60 were age and gender-matched control from community selected through a predesigned screening questionnaire from January 2019 to December 2019 in Banke district and having at least one of the main standard risk factors for DM like first degree relative with diabetes, Body mass index (BMI) ≥25 kg/m2, women with GDM, PCOS, sedentary lifestyle and other clinical conditions associated with insulin resistance like severe obesity, acanthosis nigricans, etc.
Ethical clearance was obtained from the Institutional Ethics Committee and written and verbal informed consent was obtained from all participants. Based on American Diabetes Association (ADA), the study subjects were diagnosed as prediabetic when fasting plasma glucose level was between 100–125 mg/dL (IFG), and two-hour plasma glucose (after giving 75 g of glucose) level was between 140–199 mg/dL (impaired glucose tolerance, IGT).
Participants having cardiovascular disease, renal disease, T2DM, hepatic disease, acute or chronic inflammatory disease, prolonged illness, pulmonary tuberculosis, gout and arthritis, patients taking medicines that alter glucose and lipid metabolism and plasma TG≥ 400 mg/dl were excluded from the study.
SBP, DBP, Body mass index (BMI), Waist circumference (WC), Hip circumference (HC) and Waist-to-hip ratio (WHR) were measured by standard methods. The CIMT was calculated by using a high-resolution B mode ultrasonography system with an electrical linear transducer mid-frequency of 7.5 MHz. 7 ml of venous blood samples were taken from all subjects after overnight fasting of 12 hours and 3 days of the fat-free diet, and biochemical parameters were analysed by a fully automated analyzer by standard methods.
Cardiac Risk Ratio was calculated as (CRR) = TC/HDL, Atherogenic coefficient was calculated as (AC) = non-HDL/HDLand atherogenic index of plasma was (AIP) = log TG/HDL, where the concentration of TG and HDL are in mmol/L. The entire data were expressed as mean ± standard deviation. The data were analyzed by using Statistical Package for Social Science version 16 (SPSS 16). The normal distribution of data was checked by using Kolmogorov-Smirnov (K-S) test and intergroup comparisons were analyzed by Student’s T-test while the Mann-Whitney U test was used for the intergroup comparisons of skewed data. The categorical data were analyzed by using the Chi-square test. The correlation was studied by Pearson’s correlation.
Results
The socio-demographic and biochemical characteristics of the studied individuals are depicted in Table 1. There was no statistically significant difference in age and gender between prediabetic and control groups, pointing that data were age and gender-matched. Participants of prediabetes had a statistically significant increase in the mean value of BMI (p<0.001), WC, HC, and WHR (p<0.001) as compared to control participants which demonstrated that prediabetic participants had high central obesity (based on WHR) and general obesity (based on BMI) (Table 1). In prediabetic individuals, both systolic blood pressure (p<0.001) and diastolic blood pressure (p<0.001) were significantly raised as compared to controls. There was a statistically significant increase in the lipid profile parameters: total cholesterol (p<0.001), triglyceride (p<0.001), LDL-C (p<0.001), and VLDL-C (p<0.001) in prediabetic individuals as compared to controls whereas prediabetic individuals had significantly lowered HDL values compared to control (p<0.001).In prediabetic individuals, There was a statistically significant rise in HbAlc (p<0.001), CIMT (p<0.001) and atherogenic indices, i.e. CRR (p<0.001), AC (p<0.001), and AIP (p<0.001), as compared with controls (Table 1).
In Table 2, all the cardiovascular risk factors, i.e. Body mass index(BMI), Waist-to-hip ratio(WHR), systolic blood pressure (SBP), diastolic blood pressure (DBP), fasting plasma glucose (FPG), two-hour post glucose (2 h-PG), Glycated haemoglobin (HbA1c), Total cholesterol (TC), Triglyceride (TG), low-density lipoprotein (LDL-C), and very-low-density lipoprotein (VLDL-C) were found significantly and positively correlated with Cardiac risk ratio(CRR) atherogenic coefficient (AC), atherogenic index of plasma (AIP) and Carotid intima-media thickness(CIMT) respectively in prediabetics. HDL-C was significantly negatively correlated with CRR (r=-0.801, p<0.01), AC (r=-0.801, p<0.01), AIP (r=-0.701, p<0.01) and CIMT (r=-0.342, p<0.01) in prediabetic individuals. Additionally, age was found be statistically significant and positively correlated with AIP (r=0.369, p<0.01), CRR (r=0.399, p<0.01), AC (r=0.399, p<0.01), and CIMT (r=392, p<0.01) in prediabetic subjects, pointing that as the age advances, the risk of cardiovascular disease development increases.
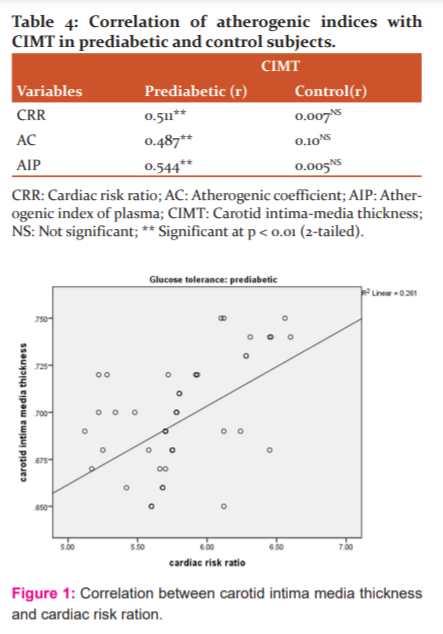
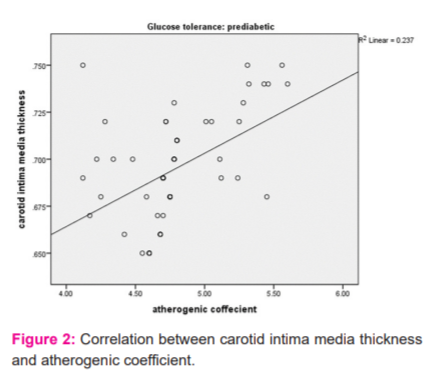
In Table 3, lipid profile parameters TC, TG and VLDL were significantly and positively correlated with CRR, AC and AIP whereas HDL was significantly and negatively correlated with CRR (r=-0.696, p<0.01), AC (r=-0.696, p<0.01) and AIP (r=-0.531, p<0.01) in control. But LDL-C was significantly and positively correlated with CRR (r=0.745, p<0.01) and AC (r=0.745, p<0.01) whereas age was significantly and positively correlated with CIMT in control individuals. In Table 4, atherogenic indices CRR (r=0.511, p<0.01), AC (r=0.487, p<0.01) and AIP (r=0.544, p<0.01) were significantly and positively correlated with CIMT in prediabetic subjects, whereas in control subjects, the correlation was not significant statistically (Figures 1, 2 & 3).
Discussion
Prediabetes state has been considered as a risk factor for diabetes mellitus and cardiovascular diseases (CVD).23 In this study, the mean fasting plasma glucose, mean 2-h post glucose, and mean glycated haemoglobin (HbA1c) levels have been statistically significantly increased from healthy to prediabetes which corroborates with the previous studies.24-26
Dyslipidaemia takes part in the pathophysiology for the development of atherosclerosis and is associated with increased risk for the development of CVD.27 LDL-C being pro-atherogenic and HDL-C being anti-atherogenic.28,29 We got statistically significant raised levels of TC, TG, LDL-C, and VLDL-C in prediabetic individuals as compared to controls, whereas HDL-C was significantly decreased which is consistent with previous studies (Table 1).13,14,27,30 Insulin resistance may lead to inhibition of suppression of lipolysis in adipose tissue that makes high free fatty acid influx in the liver and increases the secretion of hepatic VLDL-C which leads to raised TG levels and decreases the levels of HDL-C.31,32 It is established that a rise in TG levels raises the level of small dense LDL (sdLDL-C) particles that ultimately lead to increased risk for the advancement of cardiovascular disease.33 Small dense LDL particles are strongly atherogenic as they promote atherosclerosis by increasing lipid peroxidation.21
Hence, the HDL-C is called an antiatherogenic lipoprotein and also harbours paraoxonaseanti-oxidant enzymes that have a protective role on atherosclerotic heart disease and low HDL-C is associated with increased risk for CVD and carotid intima thickness.34-36 In our study, the CRR and AC are statistically significantly increased in prediabetic individuals which are in line with previous study (Table 1).26 Despite, standardized analysis of Apolipoprotein B is not always accessible in routine clinical practices and hence non-HDL-C is a better alternative.37 The ratio of non-HDL (atherogenic) and HDL-C (antiatherogenic) determines the increased risk for cardiovascular disease.38 Recently, the Atherogenic index of plasma (AIP) calculated as (logTG/HDL)is considered as an additional indicator and in fact, a better predictor for myocardial infarction and atherosclerotic heart diseases.39,40 The AIP is negatively correlated with LDL particle size and is positively correlated with the fractional esterification rate of HDL (FERHDL) and also precisely reflects the existence of atherogenic sdLDL-C and HDL-Cand is a sensitive predictor of coronary atherosclerosis and cardiovascular risk.41 It has been proposed that AIP values of -0.3 to 0.1 are correlated with low, 0.1 to 0.24 with medium, and above 0.24 with high cardiovascular risk (Table 2).42
In this study, AIP values have been found significantly increased in prediabetic individuals as compared to controls, which is consistent with the previous studies26,43,44 and we got an AIP value of 0.28 ±0.04 suggesting prediabetics at greater risk (Table 1). Both increases in Intima-media thickness and observation of plaque formation are signs of early-stage atherosclerosis and hence CIMT has been measured as an easy, non-invasive, sensitive, reliable and cheaper marker.45-47 In this study, there was a significant increase in CIMT values of prediabetic individuals as compared to control individuals which corroborated with previous studies.26,48
The increase in thickness of CIMT does not promptly give insight to cardiovascular events but consider the grade of atherosclerosis somewhere in the arterial system 51. In our study, CIMT significantly and positively correlated with atherogenic indices in prediabetic individuals but not in control which was in line with previous study26 (Tables 2-4 and Figures 1-3) and is similar to other studies.52,53 Hence it was determined that atherogenic indices can be utilized for the evaluation of the risk of subclinical atherosclerosis in prediabetic individuals. The limitation of this study was the cross-sectional nature of the data that limits the inferences about causal relationships and the sample size.
Conclusion
Our study concluded that the subtle biochemical alteration of atherosclerosis starts even before the onset of diabetes, in the prediabetes state. Hence, if diagnosed at the pre-diabetic stage preventive measures can be taken for halting the progression to full-blown DMor any of the cardiovascular complications. The atherogenic indices may be utilized along with routine lipid parameters for the better evaluation of subclinical atherosclerosis they being inexpensive, non-invasive and being easily determined from routine lipid parameters.
Acknowledgement: We acknowledge the support of the Department of Biochemistry and Medicine, Nepalgunj Medical College, Kohalpur, Nepal in this study.
Conflict of interest: None
Author contribution: Shrewastwa MK - Study planning, execution, statistical analyses and article writing; Acharya V- Article writing, review and overall supervision; Ray S- Article review
Source of Funding: Self-funde

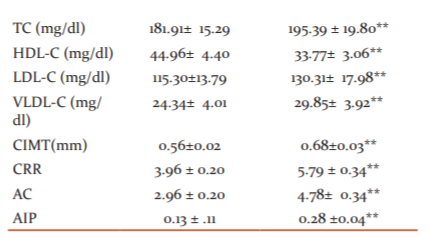
BMI: Body mass index; WC: Waist circumference; HC: Hip circumference; WHR: Waist-to-hip ratio; SBP: Systolic blood pressure; DBP: Diastolic blood pressure; FPG: Fasting plasma glucose; 2-h PG: 2-h post glucose; HbA1c: Glycated haemoglobin; TC: Total cholesterol; TG: Triglyceride; HDL: High-density lipoprotein; LDL: Low-density lipoprotein; VLDL: Very low-density lipoprotein; CIMT: Carotid intima-media thickness; CRR: Cardiac risk ratio; AC: Atherogenic coefficient; AIP: Atherogenic index of plasma; NS: Not significant; *Significant at p < 0.05; ** Significant at p < 0.001.
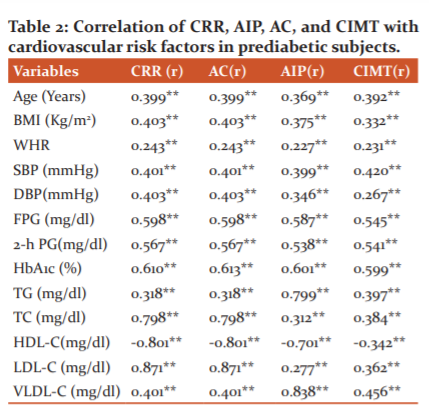
BMI: Body mass index; WHR: Waist-to-hip ratio; SBP: Systolic blood pressure; DBP: Diastolic blood pressure; FPG: Fasting plasma glucose; 2-h PG: 2-h post glucose; HbA1c: Glycated haemoglobin; TC: Total cholesterol; TG: Triglyceride; HDL: High-density lipoprotein; LDL: Low-density lipoprotein; VLDL: Very low-density lipoprotein; CRR: Cardiac risk ratio; AC: Atherogenic coefficient; AIP: Atherogenic index of plasma; CIMT: Carotid intima-media thickness; ** Significant at p < 0.01 (2-tailed).
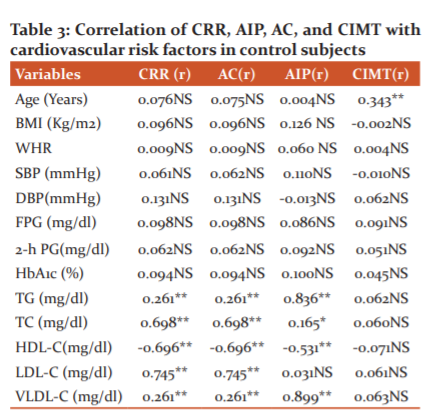
BMI: Body mass index; WHR: Waist-to-hip ratio; SBP: Systolic blood pressure; DBP: Diastolic blood pressure; FPG: Fasting plasma glucose; 2-h PG: 2-h post glucose;HbA1c:Glycated haemoglobin; TC: Total cholesterol; TG: Triglyceride; HDL: High-density lipoprotein; LDL: Low-density lipoprotein; VLDL: Very low-density lipoprotein; CRR: Cardiac risk ratio; AC: Atherogenic coefficient; AIP: Atherogenic index of plasma; CIMT: Carotid intima-media thickness;NS:not significant ;* significance at <0.05; ** Significant at p < 0.01 (2-tailed).

References:
1. International Diabetes Federation (IDF). The global burden — diabetes. http://www. idf.org/diabetes atlas/5e/diabetes.
2. International Diabetes Federation (IDF). Diabetes atlas. http://www.idf.org/diabetesatlas/5e/europe? language=zh-hans.
3. Sarah W, Gojka R, Anders G, Richard S, Hilary K. Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care 2004;27:1047–1053.
4. Ford ES, Zhao G, Li C. Pre-diabetes and the risk for cardiovascular disease: A systematic review of the evidence. J Am Coll Cardiol. 2010;55:1310–1317.
5. American Diabetes Association. Standards of medical care in diabetes-2010. Diabetes Care 2010; 33:S11-61.
6. National diabetes data group. Classification and diagnosis of diabetes mellitus and other categories of glucose intolerance. Diabetes. 1979;28(12):1039-57.
7. Mann DM, Carson AP, Shimbo D, Fanse V, Fox CS, Munter P. Impact of A1C screening criterion on the diagnosis of pre-diabetes among U.S adults. Diabetes Care 2010;33(10):2190-2195.
8. The expert committee on the diagnosis and classification of diabetes mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 1997;20(7):1183-97.
9. International Diabetes Federation. IDF Diabetes Atlas, 7th ed.; International Diabetes Federation: Brussels, Belgium, 2015.
10. Anjana RM, Deepa M, Pradeepa R, Mahanta J, Narain K, Das HK, et al. Prevalence of diabetes and prediabetes in 15 states of India: Results from the ICMR-INDIAB population-based cross-sectional study. Lancet Diabetes Endocrinol. 2017;5(8):585–596.
11. Ono K, Limbu YR, Rai SK, Kurokawa M, Yanagida J, Rai G, et al. The prevalence of type 2 diabetes mellitus and impaired fasting glucose in the semi-urban population of Nepal. Nepal Med Coll J. 2007;9:154–6.
12. Grundy S.M. Pre-diabetes, metabolic syndrome, and cardiovascular risk. J Am Coll Cardiol. 2012;59:635–643.
13. Kansal S, Kamble TK. Lipid profile in prediabetes. J Assoc Physicians India 2016;64:18–21.
14. Balgi V, Harshavardan L, Sahna E, Thomas S.K. The pattern of lipid profile abnormality in subjects with prediabetes. Int J Sci Study 2017;4:150–153.
15. Millan J, Pinto X, Munoz A, Zuniga M, Rubies-Prat J, Pallardo LF, et al. Lipoprotein ratios: Physiological significance and clinical usefulness in cardiovascular prevention. Vasc Health Risk Manag. 2009;5:757–765.
16. Bafna A, Maheshwari RS, Ved RK, Sarkar PD, Batham AR. Study of atherogenic indices in nephritic syndrome. Int J Biol Med Res. 2012;3:2257–2260.
17. Deric M, Kojic-Damjanov S, Cabarkapa V, Eremic N. Biochemical Markers of Atherosclerosis. JMB 2008;27:148–153.
18. Onat A. Lipids, lipoproteins and apolipoproteins among Turks, and impact on coronary heart disease. Anadolu Kardiyol Derg. 2004;4(3):236–245.
19. Liu T, Meng XY, Li T, Zhang DY, Zhou YH, Han QF, et al. Rosuvastatinmay stabilize vulnerable carotid plaques and reduce carotid intima media thickness in patients with hyperlipidemia. Int J Cardiol. 2016;212:20–21.
20. Hemerich D, van der Laan SW, Tragante V, den Ruijter HM, de Borst GJ, Pasterkamp G, et al. Impact of carotid atherosclerosis loci on cardiovascular events. Atherosclerosis 2015;243:466–468.
21. Cure MC, Tufekci A, Cure E, Kirbas S, Ogullar S, KirbasA, et al. Low-density lipoprotein subfraction, carotid artery intima-media thickness, nitric oxide, and tumour necrosis factor-alpha are associated with newly diagnosed ischemic stroke. Ann Indian Acad Neurol. 2013;16:498–503.
22. Mookadam F, Moustafa SE, Lester SJ, Warsame T. Subclinical atherosclerosis: Evolving the role of carotid intima-media thickness. Prev Cardiol. 2010;13:186–197.
23. Huang S, Peng W, Zhao W, Sun B, Jiang X. Higher plasma C-reactive protein and lower plasma adiponectin are associated with increased carotid artery intima-media thickness in patients with impaired glucose regulation. Asian Biomed. 2017;7:399–405.
24. Dullart RPF, De Vries R, Van Tol A, Sluiter WJ. Plasma adiponectin is a marker of increased intima-media thickness associated with type 2 diabetes mellitus and with the male gender. Eur J Endocrinol. 2007;156(3):387-394.
25. Ahsan S, Ahmed S, Ahmed SD, Nauman K. Status of serum adiponectin related to insulin resistance in prediabetics. J Pak Med Assoc. 2014; 64(2):184-8.
26. Mahat RK, Singh N, Rathore V, Gupta Akashara, Shah RK. Relationship between Atherogenic Indices and Carotid Intima-Media Thickness in Prediabetes: A Cross-Sectional Study from Central India. Med Sci (Basel). 2018;6(3):55.
27. Yang C, Sun Z, Li Y, Ai J, Sun Q, Tian Y. The correlation between serum lipid profile with carotid intima-media thickness and plaque. BMC Cardiovasc Disord. 2014;14:181.
28. Nakamura H, Arakawa K, Itakura H, Kitabatake A, Goto Y, Toyota T, et al . Primary prevention of cardiovascular disease with pravastatin in Japan(MEGA Study): A prospective randomised controlled trial. Lancet. 2006;368:1155–1163.
29. Cannon CP, Braunwald E, McCabe CH, Rader DJ, Rouleau JL, Belder R, et al . Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004;350:1495–1504.
30. Gholi Z, Heidari-Beni M, Feizi A, Iraj B, Askari G. The characteristics of pre-diabetic patients associated with body composition and cardiovascular disease risk factors in the Iranian population. J Res Med Sci. 2016;21:20.
31. Boden G, Laakso M. Lipids and glucose in type 2 diabetes: What is the cause and effect? Diabetes Care 2004;27:2253–2259.
32. McGarry JD. Banting lecture 2001: Dysregulation of fatty acid metabolism in the etiology of type 2 diabetes. Diabetes 2002;51:7–18.
33. Acharya V, Toora B D. A study of sdLDL-c and insulin resistance in apparently healthy South Indian obese young adults. IJCBR. 2015;2(1):41-47
34. Gaal K, Tarr T, Lorincz H, Borbas V, Seres I, Harangi M, et al. High-density lipoprotein antioxidant capacity, subpopulation distribution and paraoxonase-1 activity in patients with systemic lupus erythematosus. Lipids Health Dis. 2016;15:60.
35. Krauss RM. Lipids and lipoproteins in patients with type 2 diabetes. Diabetes Care 2004; 27:1496–1504.
36. Rosvall M, Persson M, Östling G, Nilsson PM, Melander O, Hedblad B, et al. Risk factors forthe progression of carotid intima-media thickness over a 16-year follow-up period: The Malmö Diet and Cancer Study. Atherosclerosis. 2015;239:615–621.
37. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final Report. Circulation 2002;106:3143–3421.
38. Singh M, Pathak MS, Paul A. A study on atherogenic indices of pregnancy induced hypertension patients as compared to normal pregnant women. J Clin Diagn Res. 2015;9:BC05–BC08.
39. Onat A, Can G, Kaya H, Hergenc G. Atherogenic index of plasma (log10 triglyceride/high-density lipoprotein-cholesterol) predicts high blood pressure, diabetes, and vascular events. J Clin Lipidol. 2010;4:89–98.
40. Dobiasova M. Atherogenic index of plasma [log(triglycerides/HDL-cholesterol)]: Theoretical and practical implications. Clin Chem. 2004; 50: 1113–1115.
41. Dobiasova M, Frohlich J. The plasma parameter log (TG/HDL-C) as an atherogenic index: Correlation with lipoprotein particle size and esterification rate in apoB-lipoprotein-depleted plasma (FERHDL). Clin Biochem. 2001;34:583–588.
42. Dobiasova M. AIP-atherogenic index of plasma as a significant predictor of cardiovascular risk: From research to practice. Vnitr Lek. 2006;52:64–71.
43. Regmi P, Baral B, Raut M, Khanal MP. Atherogenic index of plasma for prediction of future cardiovascular disease in prediabetes and diabetes population. Atherosclerosis 2016; 252:e120.
44. Thiyagarajan R, Subramanian SK, Sampath N, Trakroo M, Pal P, Bobby Z, et al. Association between cardiac autonomic function, oxidative stress and inflammatory response in impaired fasting glucose subjects: Cross-sectional study. PLoS ONE 2012;7:e41889.
45. O'Leary D.H, PolakJF,Kronmal RA, Manolio TA, Burke GL,Wolfson Jr Sk. Carotid-artery intimaand media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med. 1999;340:14–22.
46. Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intima-media thickness: A systematic review and meta-analysis. Circulation 2007;115:459–467.
47. Icli A, Cure E, Cure MC, Uslu AU, Balta S, Mikhailidis DP, et al. Endocan levels and subclinical atherosclerosis in patients with systemic lupus erythematosus. Angiology2016; 67: 749–755.
48. Altin C, Sade LE, Gezmis E, Ozen N, Duzceker O, Bozbas H, et al. Assessment of subclinical atherosclerosis by carotid intima-media thickness and epicardial adipose tissue thickness in prediabetes. Angiology 2016;67:961–969.
51. Touboul PJ, Grobbee DE, den Ruijter H. Assessment of subclinical
atherosclerosis by carotid intima media thickness: Technical issues. Eur J Prev Cardiol. 2012;19:18–24.
52. Yildiz G, Duman A, Aydin H, Yilmaz A, Hür E, Ma?gden K, et al . Evaluation of the association between the atherogenic index of plasma and intima-media thickness of the carotid artery for subclinical atherosclerosis in patients on maintenance hemodialysis. Hemodial Int. 2013;17:397–405.
53. Cure E, Icli A, UgurUslu A, Aydo?ganBaykara R, Sakiz D, Ozucan M, et al . The atherogenic index of plasma may be a strong predictor of subclinical atherosclerosis in patients with Behçet disease. Rheumatology 2017;76:259–266.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License