IJCRR - 13(11), June, 2021
Pages: 117-121
Date of Publication: 04-Jun-2021
Print Article
Download XML Download PDF
Role of Computed Tomography of the Nose and Paranasal Sinuses in COVID-19 Patients with Anosmia: Our Experiences at a Tertiary Care Teaching Hospital
Author: Swain SK, Das S, Kar D, Das SR
Category: Healthcare
Abstract:Background: Olfactory dysfunction is a unique clinical presentation reported among coronavirus diseases 2019(COVID-19) patients. The exact pathophysiology for olfactory dysfunction in COVID-19 infections is poorly understood. Objective: To evaluate the anosmia in COVID-19 infections with help of computed tomography (CT) scan of the nose and paranasal sinus. Methods: This prospective study was performed in COVID-19 patients with symptoms of olfactory dysfunction. We evaluated the conductive etiologies of the anosmia with help of the CT scan of the nose and paranasal sinuses. Results: There were 62 patients with anosmia with COVID-19 infections included in this study. The age ranges of the study patients were 18 to 76 years with a mean age of 46.3\?14 years. Complete anosmia was found in 67.74% of cases and 82.25% of cases presented with sudden onset of olfactory dysfunction. Gustatory dysfunction or dysgeusia was found in 51.61% of the cases. There were no pathological lesions of the olfactory cleft in the CT scan of the nose and paranasal sinuses. Conclusion: Obstructive or conductive pathology in the sinonasal tract does not play a significant role in causing the anosmia in COVID-19 patients. We did not find much sinonasal pathology in the CT scan of the nose and paranasal sinuses in COVID-19 patients with anosmia.
Keywords: Computed tomography, Anosmia, COVID-19 patients, Olfactory cleft
Full Text:
INTRODUCTION
The coronavirus disease 2019(COVID-19) pandemic is caused by severe acute respiratory syndrome coronavirus-2(SARS-CoV-2) and currently presenting as a global threat.1 The common clinical manifestations in COVID-19 patients are fever, dry cough and dyspnea. Other additional clinical presentations include fatigue, headache, nausea, vomiting, myalgia, anosmia and dysgeusia.2 The olfactory dysfunction may be anosmia (complete loss of smell), hyposmia(partial loss of smell), phantosmia(sensing odour without any external stimulant) and parosmia(a change in the usual feeling of odour). Anosmia is a cardinal clinical manifestation found in a COVID-19 patient.3 Although SARS-CoV-2 of COVID-19 pandemic and SARS-CoV have similar genetic sequencing, pathogenesis and cellular entry, the olfactory dysfunction was not documented during the previous SARS-CoV epidemic.4 The pathogenesis for post-viral anosmia includes conductive, sensorineural and mixed etiologies. The sinonasal pathology may block the entrance of the odorants to the olfactory epithelium of the nasal cavity, so causing conductive olfactory dysfunction. So, treatment of the olfactory dysfunction may by obstructive sinonasal pathology or conductive pathology is different from the sensorineural loss. So, detailed history and clinical examinations are vital before evaluating the anosmia in the COVID-19 pandemic. The detailed clinical examination includes complete ear, nose and throat examination along with diagnostic nasal endoscopy. However, performing the diagnostic nasal endoscopy in COVID-19 patients is considered a high-risk procedure for viral transmission to health care professionals. So, the CT scan of the nose and paranasal sinuses is the investigation of the choice for studying the sinonasal pathology in COVID-19 patients with anosmia.5 In this study, we considered the computed tomography (CT) scan of the nose and paranasal sinuses as an alternative to the diagnostic nasal endoscopy for evaluating the etiopathology of the olfactory dysfunction.
MATERIALS AND METHODS
This prospective study was done at a tertiary care teaching hospital attached to a 500 bedded COVID-19 hospital. This study was conducted between March 2020 to October 2020 and approved by the Institutional Ethical Committee (IEC) with the reference number of IEC/IMS/SOA/12.03.2020. The COVID-19 patients with anosmia attending the outpatient department were included in this study. The COVID-19 patients were confirmed by the reverse transcription-polymerase chain reaction (RT-PCR) assay of nasopharyngeal samples. Patients with age less than 18 years, previous history of smell abnormalities, neurological diseases, sinonasal surgery, endonasal neurosurgery and pregnant lady were excluded from this study. The sinonasal symptoms including smell status were evaluated subjectively with help of the questionnaires including different co-morbidities of the participants. The screening of the CT scan of the nose and paranasal sinuses with coronal views (Siemens, 64-channel) was performed for assessing the diseases of the nose and paranasal sinuses along with the status of the stomatal complex(OMC), ethmoidal sinuses, maxillary sinuses, sphenoid sinuses and olfactory cleft. The Lund-Mackay CT scan scoring was used for evaluating the nose and paranasal sinuses where 0 indicates normal, 1 partial and 2 indicates total opacity for the paranasal sinuses. The mucosal thickening and swelling at the olfactory cleft and ethmoidal sinuses are considered as obstructive olfactory dysfunction. Data were analyzed by SPSS and reports were reported as mean, standard deviation and percentage.
RESULTS
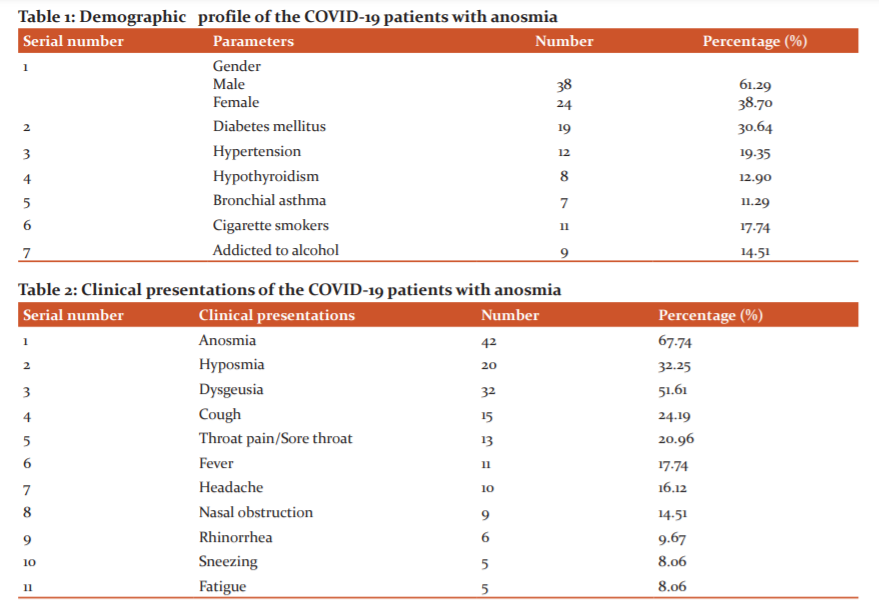
There were 62 COVID-19 patients with anosmia included in this study. The age ranges of the study patients were 20 to 76 years with a mean age of 46.3±14 years. There were 38 (68.29%) males and 24 (38.70%) females with male to female ratio of 1.58:1. The commonest morbidity associated with COVID-19 patients with anosmia was diabetes mellitus (30.64%) (Table 1).
Out of the 62 patients, 42 (67.74%) presented with complete anosmia and 20 (32.25%) with partial anosmia (hyposmia). Along with anosmia, the COVID-19 patients presented with certain accompanying symptoms such as fever (17.74%), headache (16.12%), cough (24.19%), nasal obstruction (14.51%), rhinorrhea (9.67%) and fatigue (8.06%) (Table 2).
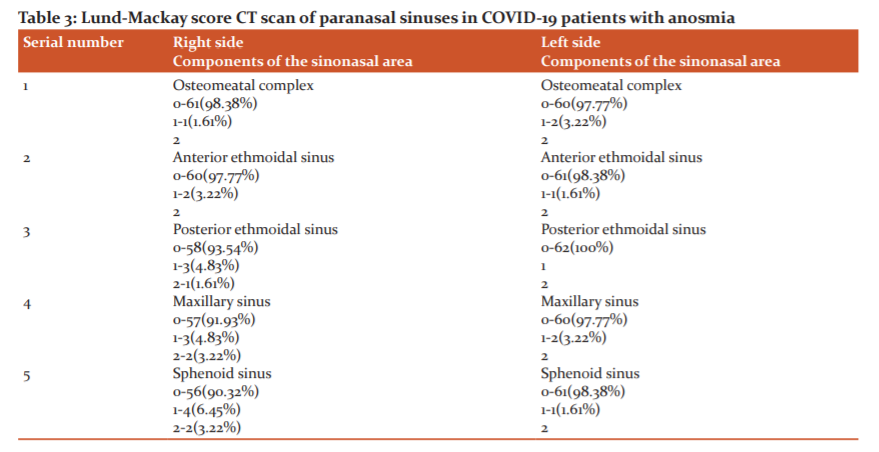
Out of 62 patients, 51(82.25%) were presented with sudden onset of olfactory dysfunction. There were 32 patients (51.61%) who presented with associated taste disturbances. The involvement of the paranasal sinuses in the CT scan was analyzed as per Lund-Mackay score. Total Lund-Mackay score was 0 in 61(98.38%) and 1 in 1(1.61%) patients at the right side of the stomatal complex whereas 0 in 60 (90.77%) patients and 1 in 2 (3.22%) patients on the left side of the stomatal complex (Table 3) There were no opacification or abnormalities at the olfactory cleft in any of the patients.
DISCUSSION
COVID-19 is an infectious disease of the respiratory tract caused by a novel virus called severe acute respiratory syndrome coronavirus 2(SARS-Co-2) and primarily spreads from human to human by droplets which carry virus. Novel coronavirus disease 2019(COVID-19) was an outbreak which emerged in China in December 2019 and has rapidly spread into a global pandemic.6 There are varieties of clinical presentations reported since starting of the COVID-19 pandemic including the symptom of anosmia.7 This infection often causes respiratory symptoms and even causes respiratory distress and death.8 Rapid spread of the COVID-19 infections currently threatens the world and also the healthcare system. In the COVID-19 pandemic, many patients have reported an acute loss of smell and taste. The association between the smell and taste disturbances in COVID-19 patients may carry important implications towards future investigations for understanding the SARS-CoV-2 virus ability to overwhelm the host immune response. The sudden onset of anosmia or dysgeusia should be considered an important symptom in the international forum for early diagnosis of COVID-19 patients. In this study, 82.25% of patients were presented with sudden onset of olfactory dysfunction. These symptoms act as a biomarker in this pandemic for early isolation of the patient. The most efficient method for preventing the spread of the COVID-19 infection is the early identification of the symptoms like smell and taste abnormalities and isolation of the patient. Olfactory dysfunction is usually associated with poor quality of life. Now the early identification of COVID-19 patient is urgently needed to isolate the patient and control the spread of the infection.8 The exact pathophysiology for smell disturbances in COVID-19 infections is not clear. There are controversies regarding the aetiology of impaired smell in COVID-19 patients whether by infecting directly or by neurological disease or other infections or direct damage of the organ itself. There are two potential mechanisms for explaining the olfactory dysfunctions such as mechanical blockage of the olfactory function due to inflammation, as found in the olfactory cleft syndrome or neuro-epithelial injury occurred when the olfactory epithelium and sensory neurons damaged by the infections.9,10
The explanations for olfactory dysfunction in the post-viral period are secretions, congestion and inflammatory changes in the mucosal lining of the sinonasal tract.11 The obstruction to the olfactory cleft or neurogenic invasion/involvement of the olfactory bulb in post-viral infections is also the explanation for the olfactory dysfunctions.12 So, the disturbances in the olfaction are mostly due to blockage of the airway, sensory deficits by neuroepithelial injury or damage to the olfactory bulb, olfactory tract or central olfactory tract including prefrontal lobe, septal nuclei, amygdala and temporal lobe.13 The neuroinvasive property of the SARS-CoV-2 might have a role in the pathophysiology of smell and taste disturbances.14 As the olfactory mucosa is found at the roof of the nasal cavity, a direct or indirect effect of the SARS-CoV-2 in situ may be another explanation for these clinical manifestations. Infections, inflammations and certain chemical agents have an impact on the dendritic processes at the olfactory epithelium by inflammatory cytokine release, so induces apoptosis of the olfactory neurons.15 SARS-CoV-2 is also directly responsible for causing olfactory dysfunctions.16 In the current COVID-19 pandemic, the symptoms such as anosmia and ageusia are found as isolated symptoms or in association with other respiratory symptoms.17 In this study, 32 patients (51.61%) presented with taste disturbances out of the 62 COVID-19 patients with anosmia.
Smell disturbances are often found in COVID-19 patients. These symptoms may be presented as the first and/or only symptoms by COVID-19 patients. Olfactory dysfunction due to diseases of the sinonasal mucosa has a high chance of recovery whereas the recovery of the olfactory dysfunction by sensorineural loss is uncertain or late recovery. So, the proper understanding of the exact mechanism for olfactory dysfunction is an important part of the treatment and prognostication of this symptom. The mucosal lining of the nasal cavity has high angiotensin-converting enzyme 2 (ACE2) receptor expressions, so permit for the route of the virus.18 Despite these findings, nasal symptoms are absent in the majority of the COVID-19 patients. In this study, nasal symptoms like rhinorrhea (9.67%), nasal block (14.51%) and sneezing (8.86%) were uncommon. One study documented that non-neuronal cells of the olfactory epithelium and non-olfactory neurons are the direct target of the SARS-CoV-2.18 The olfactory epithelium express genes involved for virus entry such as angiotensin-converting enzyme 2(ACE2) receptor and transmembrane protease serine 2 (TMPRESS2) whereas the sensory neuron of the olfactory area nor neurons of the olfactory bulb express these genes.19 The two proteins ACE2 and TMPRESS2 are needed for the host cell entry which facilitates replication, accumulation and binding of the SARS-CoV-2 and expressed in the sustentacular cells, receptor neurons of the olfactory neuro-epithelium which have a potential role in the loss of smell in COVID-19 patients.20 These reports explain that infection of the non-neural cell types in olfactory epithelium causes anosmia in COVID-19 patients.
Now the early identification of COVID-19 patient is urgently needed to isolate the patient and control the spread of the infection. Performing the diagnostic nasal endoscopy in COVID-19 patients is vulnerable to the spread of the infections to other persons. Imaging like CT scan is useful imaging for proper assessment of the nose and paranasal sinuses There is almost very little research related to imaging in the COVID-19 patients with anosmia. A study of MRI in cases of isolated anosmia in COVID-19 patients reveals a normal olfactory bulb. In another study, no mucosal congestion was found in the olfactory cleft.21 One study of FDG PET/CT scan in COVID-19 patients with anosmia showed metabolic activity of the olfactory pathways where hypometabolism was seen in the left orbit-frontal cortex under the neutral olfactory condition which suggest an impaired neural function as an underlying cause for anosmia.22 In this study, the olfactory tract was not blocked by any sinonasal pathologies.
Proper history taking, clinical examinations and imaging like CT scan and MRI are required for assessing the anosmia patients to rule out the underlying aetiology. Performing diagnostic nasal endoscopy for assessing the anosmia is a high-risk procedure during the COVID-19 pandemic as it often spread infections to health care professionals. So, imaging is useful for evaluating the nose and paranasal sinuses in COVID-19 patients with anosmia. Different imaging studies like CT scan and/or MRI are useful for assessment of the anosmia to confirm the underlying aetiology. In this study, we evaluated the COVID-19 patients with anosmia and performed a CT scan of the nose and paranasal sinuses to rule out the conductive mechanism for anosmia. We did not found significant pathologies like mucosal thickening or opacification at the sinonasal tract and olfactory region. In this study, clinical presentations like nasal obstruction were found in 14.51% and rhinorrhea found in 9.67%. So, this study favours the non-conductive mechanism such as sensorineural olfactory dysfunction as the important cause for anosmia in COVID-19 patients. The anosmia due to mucosal thickening or sinonasal obstructive pathology has a rapid recovery rate but in the case of neural pathology of the olfactory pathway, the recovery rate is uncertain or delayed. So, the exact understanding of the mechanism of anosmia in COVID-19 patients is an important prognostication and helpful for the treatment of this symptom in the current pandemic.
CONCLUSION
The coronavirus disease 2019(COVID-19) pandemic posed an overwhelming challenge for clinicians across the world in the last few months. The exact pathophysiology for the development of the anosmia in COVID-19 patients is still poorly understood. Diagnostic nasal endoscopy is not safe for routine assessment of the nose in COVID-19 patients with anosmia. The nasal endoscopy has a high risk for transmission of infections to health care professionals. CT scan of the nose and paranasal sinuses is very useful and safe for assessing the anosmia in COVID-19 patients and provides anatomical details in lieu of the diagnostic nasal endoscopy. As there was no significant obstructive or conductive pathology in the nose and paranasal sinuses found in this study among COVID-19 patients with anosmia, so certain therapies like steroids for treatment of the anosmia is questionable.
Conflict of Interest: Nil
Funding: Nil
Author Contributions: SKS: Concept, data collection and data analysis; SD: Data collection, data analysis; DK: Data collection and drafting the manuscript; SRD: Data collection.
References:
-
Swain SK, Agrawal R. Mastoid surgery: a high risk aerosol-generating surgical procedure in COVID-19 pandemic. Int J Otorhinol Head Neck Surg. 2020; 6(10):1941.
-
Xu YH, Dong JH, An WM, Lv XY, Yin XP, Zhang JZ, et al. Clinical and computed tomographic imaging features of novel coronavirus pneumonia caused by SARS-CoV-2. J Infect. 2020;80:394-400.
-
Swain SK, Acharya S, Sahajan N. Otorhinolaryngological manifestations in COVID-19 infections: An early indicator for isolating the positive cases. J Sci Soc. 2020; 47(2):63.
-
Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020; 395:565-74.
-
Busaba NY. Is imaging necessary in the evaluation of the patient with an isolated complaint of anosmia? J Ear Nose Throat. 2001;80(12):892-6.
-
Swain SK, Behera IC. Managing pediatric otorhinolaryngology patients in coronavirus disease-19 pandemic-A real challenge to the clinicians. Ind J Child Health. 2020;7(9):357-62.
-
Filatov AA, Sharma PP, Hindi FF, Espinosa PS. Neurological complications of coronavirus disease (COVID-19). Encephalopathy. 2020;12(3):e7352.
-
Swain SK, Das S, Padhy RN. Performing tracheostomy in intensive care unit-A challenge during COVID-19 pandemic. Sir Med J. 2020; 72(5):436-442.
-
Zhang W, Du RH, Li B, Zheng XS, Yang XL, Hu B, et al. Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes. Emerg Microb Infect. 2020;9(1):386-9.
-
Gane SB, Kelly C, Hopkins C. Isolated sudden onset anosmia in COVID-19 infection. A novel syndrome. Rhinology 2020;10:1-4.
-
Li KY, Liu J, Xiao W, Wu Y, Ren YY, Wei YX. Characteristics of post viral olfactory disorder. Chinese J Otorhinolaryngol Head Neck Surg. 2016;51(11):838-41.
-
Yao L, Yi X, Pinto JM, Yuan X, Guo Y, Liu Y, et al. Olfactory cortex and olfactory bulb volume alterations in patients with post-infectious olfactory loss. Brain Imag Behav. 2018;12: 1355-62.
-
Vaira LA, Deiana G, Fois AG, Pirina P, Madeddu G, De Vito A, et al. Objective evaluation of anosmia and ageusia in COVID-19 patients: Single centre experience on 72 cases. Head Neck. 2020; 42 (6):1252-8. .
-
Bilinska K, Jakubowska P, Von Bartheld CS, Butowt R. Expression of the SARS-CoV-2 entry proteins, ACE2 and TMPRSS2, in cells of the olfactory epithelium: identification of cell types and trends with age. ACS Chem Neurosci. 2020; 11 (11):155-62.
-
Kim BG, Kang JM, Shin JH, Choi HN, Jung YH, Park SY. Do sinus computed tomography findings predict olfactory dysfunction and its postoperative recovery in chronic rhinosinusitis patients? Am J Rhinol Allergy. 2015;29 (2015):69-76.
-
Hwang CS. Olfactory neuropathy in severe acute respiratory syndrome: report of a case. Acta Neurol Taiwan. 2006; 15(1):26-8.
-
Vavougios GD. Potentially irreversible olfactory and gustatory impairments in COVID-19: indolent vs. fulminant SARS-CoV-2 neuroinfection. Brain Behav Immun. 2020; S0889-1591(20):30674-7.
-
Sungnak W, Huang N, Bécavin C, Berg M, Queen R, Litvinukova M, et al. SARS-CoV- 2 entry genes are most highly expressed in nasal goblet and ciliated cells within human airways. Nat Med. 2020; 26:681-7.
-
Brann DH, Tsukahara T, Weinreb C, Marcela Lipovsek M, Koen Van den Berge K, Gong B, et al. Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia. BioRxiv. 2020. https://doi.org/10.1101/2020.03.25.009084.
-
Lechien JR, Chiesa-Estomba CM, De Siati DR, Horoi M, Le Bon SD, Rodriguez A, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Oto-Rhino-Laryng. 2020; 277:2251-61.
-
Karimi Galougahi M, Ghorbani J, Bakhshayeshkaram M, Safavi Naeini A, Haseli S. Olfactory bulb magnetic resonance imaging in SARS-CoV-2-induced anosmia: the first report. Acad Radiol. 2020; 27(6):892-3.
-
Karimi Galougahi M. Yosefi-Koma A, Bakhshayeshkaram M, Raad N, Haseli S. FDG PET/CT scan reveals hypoactive orbitofrontal cortex in anosmia of covid-19. Acad Radiol. 2020;27(7): 1042-43.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License