IJCRR - 13(11), June, 2021
Pages: 81-86
Date of Publication: 04-Jun-2021
Print Article
Download XML Download PDF
Incidence and Factors Impacting Candiduria in Catheter-Associated Urinary Tract Infection in Tribal Patients of Medicine Intensive Care Unit in a Tribal-Dominated Tertiary Care Hospita
Author: Monalisa Subudhi, Jagatheeswary PAT, Susanta Kumar Sahu, Sudhanshu Kumar Das
Category: Healthcare
Abstract:Introduction: Candiduria in catheter-associated urinary tract infection (CAUTI) is most challenging because of the emergence of extreme drug-resistant infections especially in critically ill patients of medicine Intensive Care Unit (MICU) in a tribal-dominated rural tertiary care centre. Objective: The study aims to find out the incidence, risk factors and their impact on candiduria in CAUTI in the tribal-dominated rural tertiary care centre. Methods: This prospective study was conducted in MICU of SLNMCH, Koraput(Odisha) from March 2019 to February 2020. It included confirmed cases of CAUTI, diagnosed as per standard Centre's for Disease Control National nosocomial infection and diagnosed cases of candiduria. Demographic and clinical data of these patients were collected. Under all aseptic conditions, urine was collected transurethral and sent for microscopy and culture and sensitivity to the microbiology laboratory. Results: In our study, the incidence of candiduria in CAUTI was 19.5%.These cases were more common in the tribal population (88.9%), female gender(75%), age more than 40 years and up to 60 years(62.5 %), duration of the catheter up to 7 days(62.5%), low socioeconomic status(62.5%) Staphylococcus aureus being the commonest associated microorganism(37.5%), followed by E coli(25%) and type 2 diabetes mellitus(50 %) being the most common morbidity. Conclusion: Our analysis precisely of this Tribal population, brings several important and unique findings(risk factors of multi-organ involvement) than other study and population, which will modify or add in the development of some new or update guidelines that might help critical care physicians in dealing with these patients on multiple organs support, and reduce morbidity, mortality in the ICU.
Keywords: Catheter-associated urinary tract infection (CAUTI), Medicine Intensive Care Unit (MICU), Urinary tract infection (UTI), Diabetes mellitus (DM), Sickle cell anaemia (SCA), Device associated infection (DAI)
Full Text:
INTRODUCTION
Catheter-associated urinary tract infections (CAUTI) is the most common hospital-acquired infection and account for about 80% of nosocomial infections.1 The important risk factors for CAUTI are ICU admissions, diabetes mellitus, female gender, increasing age, more duration of Transurethral indwelling urinary catheterization, broad-spectrum antibiotic therapy, associated infections.2,3 CAUTI in critically ill patients of medical Intensive Care units is becoming an increasing problem and common due to candida infections. Incidence of candiduria is about 10-20% of nosocomial infection.
In MICUs, the incidence of candiduria is about 20% of UTI and second to E. coli.4 Candiduria is common in patients with transurethral indwelling urinary catheterizations in the MICU. Candida albicans is the most common yeast isolated in patients with CAUTI.5
There are three presentations of candiduria: (1) Colonization or contamination and usual presentations of candida, asymptomatic(most common presentation), (2) UTI- cystitis or pyelonephritis and (3) systemic infection mostly in critically ill and immunocompromised patients.6 The incidence of candida is about five to ten times in hospitalized patients than in the general population due to the presence of risk factors and still more in the critically ill patients of medical Intensive Care Centre. In hospitalized patients, the common cause of secondary healthcare-associated infection is catheter-related urinary tract colonisation. Candiduria is an unavoidable condition in 50% of cases, where catheterization is more than 5 days.7
The indwelling urinary catheters are more commonly associated with biofilm formation in the mucosal surface and surfaces of catheters, consisting of complex enclosing microcolonies of candida Albicans, hyphae and pseudohyphae. Biofilms are usually resistant to antifungal therapy, for which the indwelling urinary catheters are to be removed or replaced or antimicrobial urinary catheters are to be used with the management of associated risk factors.2
We know, what are the potential risk factors and pattern of the microbiological profile of CAUTI, in the ICU of Rural and Urban area tertiary care centres. But we do not have any knowledge or any recent studies describing the factors that influence candiduria in CAUTI in especially Tribal people. Unawareness, lack of health consciousness and living style, make them more prone to infection leading to more ICU admission, morbidity and mortality. Here we tried to explore the factors (demographic as well as risk factors ) responsible for more incidence and their influence on candiduria in CAUTI, which vary according to all this. So that, preventive strategies should be planned such as antifungal policy, a protocol for using the device, health awareness in the ICU to give quality health care and reduce morbidity and mortality in tribal people in the ICU of any hospital in Tribal area.
The study aims to find out the incidence, risk factors and their impact on candiduria in catheter-associated urinary tract infection in Tribal patients of Medical intensive care unit in a tribal-dominated tertiary care centre.
Materials and methods
Study Design
This prospective study was carried out in the Medical Intensive Care Unit of SriLaxmanNayak Medical College & Hospital, from March 2019 to February 2020 with the institutional ethical committee approval (02/28.02.2019 ).
Inclusion criteria
1. MICU patients aged ≥ 18 years old. 2. All MICU patients with a transurethral indwelling catheter for >48 hours. 3. Patients, who are willing to give, an admission urine sample following catheterization for culture and sensitivity to rule out preexisting UTI. 4. Patients having symptoms with microbiological confirmation of pyuria and presence of Candida spp. 5. Patients with risk factors as Diabetes mellitus and Sickle cell anaemia,6. Who is willing and signed the consent form to take part in the study.
Exclusion criteria
1. Patients with pre-existing UTI, 2. Presence of signs and symptoms of CAUTI within 2 calendar days of catheterization. 3. Patients who used antibiotics more than 2 weeks before the time of the study, 4. Risk factors other than DM and SCA.
Study population
The study population was all adult patients, aged ≥18 years, admitted to MICU with different complaints with an indwelling urinary Foley’s catheter, more than 48 hours during their admission, in a Tribal tertiary care centre. between the study period from April 2019 to March 2020, developed features of symptomatic urinary tract infection following catheterization were enrolled in the study. It included confirmed cases of CAUTI, diagnosed as per standard Centre for Disease Control National nosocomial infection and diagnosed cases of candiduria.
Sample collection & Processing
Urine was collected transurethrally without disconnecting the closed drainage system at any point of time with a sterile needle and syringe and the distal 5 cm of the aseptically removed urinary catheter was cut and sent to the microbiology laboratory. The urine samples and the catheter were sent to the laboratory within 1h of collection. The urine samples were processed as microscopy, culture identification and antibiotic susceptibility testing by the routine standard laboratory procedure in the microbiology laboratory. Urine microscopy was performed on the centrifuged catheter urine specimen. Urine Culture was done with the standard cultured method as appropriate for urinary pathogens. A positive fungal culture was defined as isolation of fungi with >10³ CFU/ml on a specimen collected at least 48 hrs after hospital admission and >105 CFU/ml of urine in non-catheterized and catheterized samples, respectively. The specimens were cultured by a semi-quantitative method using Mac Conkey Agar and Blood Agar as culture medium. The plates were read after 24 hours of incubation for any growth[1]. Based on colony morphology on 5% sheep blood agar and no growth on Mac Conkey agar, the colonies were suspected to belong to Candida species. Gram-stained smear showed Gram-positive budding yeast cell with pseudohyphae.
Data collection
Patient’s demographic and clinical data as age, sex, nutritional status, underlying illness, the severity of the illness and device utilization (duration of catheterization ), signs and symptoms of sepsis were recorded. Detailed investigations were collected.
Statistical Analysis
Microsoft Excel was used for data entry and analyzed with SPSS software version 20.0. For quantitative variable, median and for qualitative variable, frequency (percentage) were used to present the results.
Results
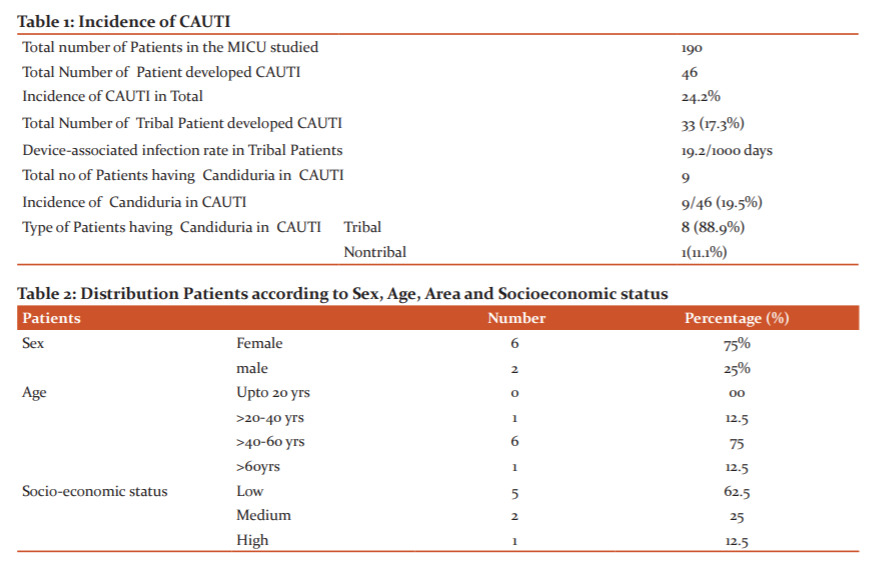
The study was conducted in a 20 bedded medicine intensive care unit, over one year from April 2019 to March 2020 in a Tribal tertiary care centre. A total of 190 patients were exposed to an indwelling urinary catheter device for a total duration of 1712 device days. Out of 190 catheterized patients, 46(24.2%) were diagnosed microbiologically as CAUTI with an incidence of 24.2%. Whereas, the DAI rate in 33 Tribal patients associated with CAUTI in our study, was 19.2 per 1000 device days with an incidence of 17.3%.Of these 46 cases of CAUTI, candiduria was present in 9 cases with an incidence of 19.5%. (Table 1).
According to the type of patients who developed CAUTI due to Candiduria in our MICU, Tribals were 8 (88.9% ) and Nontribals were 1 (11.1%). ( Table-1) Female Tribal patients 6 (75%) were affected more as compared to males 2(25%). Whereas in age factor, tribal patients with candiduria in 1 (12.5%) case under >20-40 years, 6 (75%) cases in >40-60 years and 1 (12.5% ) case in above 60 years old respectively. Depending upon the Socioeconomic status, most of the tribal patients 5 (62.5%) were under low socioeconomic status group than 2 (25%) in medium and 1(12.5%) in the high-status group (Table 2).
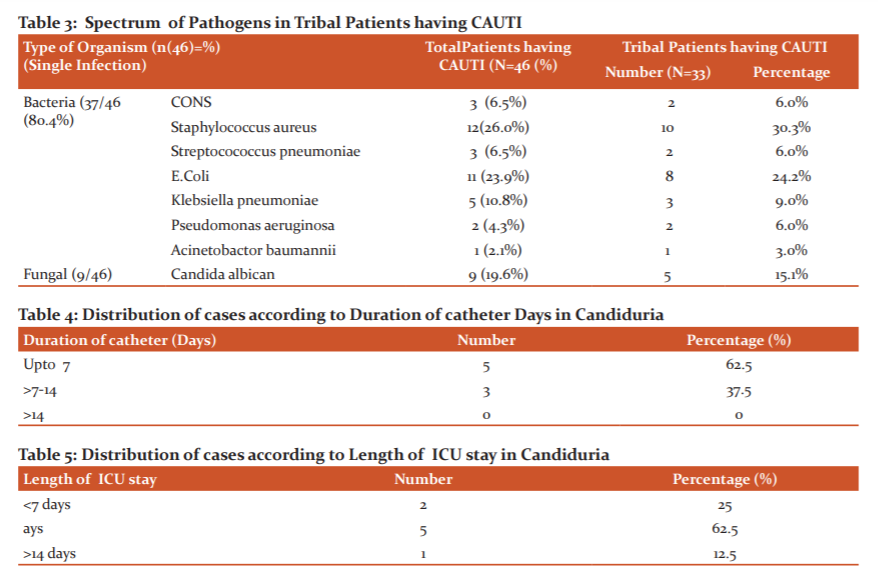
Over one year, in the trend in the microbiological profile of CAUTI in Tribal patients, the most common gram-positive pathogen was Staphylococcus aureus 10 (30.3%) followed by CONS 2(6.0%) and Streptococcus Pneumonae 2 (6.0%). Whereas in gram-negative bacilli , E. coli 8 (24.2%) were the most common pathogen followed by Klebsiella pneumonia 3 (9.0%), Pseudomonas aeruginosa 2 (6.0%) and Acinetobacter baumannii 1(3.0%) . Candida Albicans was the only common fungal pathogen accounting for 5(15.1%) (Table 3).
Duration of urethral catheterization up to 7 days were 6 cases (62.5%), more common in compared to duration more than 7 days and up to 14 days (37.5%, Table 4).
Length of ICU stay was another risk factor to develop candiduria in CAUTI in our study, according to which 5(62.5%) patients stayed for 7-14 days, 2 (25%) for less than 7 days and 1(12.5%) stayed for more than 14 days (Table 5).
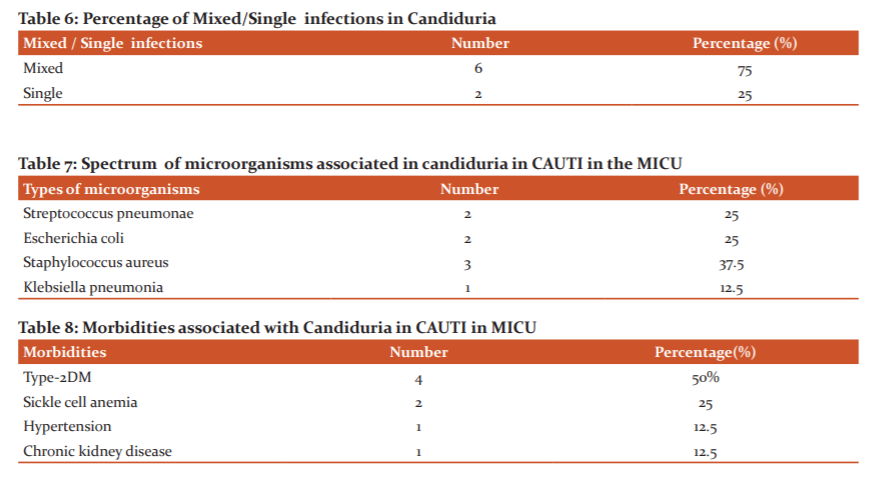
Single infections with microorganisms were less common in 2 cases (22.2%) as compared to mixed infections with microorganisms in 6 cases (77.8%) associated with Candiduria in CAUTI (Table 6).
The bacterial pathogens isolated in our study, in association with candiduria in CAUTI were Staphylococcus aureus 3 cases (37.5%) the commonest organism followed by E.coli and Streptococcus pneumonia 2 cases (25%) in each (Table 7).
Considering the risk factors associated with candiduria in Tribal patients, in the study, Type-2 Diabetes Mellitus in 4 (12.1%) cases, Sickle cell anaemia in 2 (25%) cases, Hypertension and Chronic kidney disease in 1(12.5%) cases each (Table 8).
Discussion
Catheter-associated urinary tract infection is a common healthcare-associated infection especially on critically ill patients of medical intensive care units. Moreover the presence of risk factors like type 2 diabetes mellitus, use of broad-spectrum antibiotics, longer indwelling catheterization, increase the development of urinary tract infection in catheterized patients. Many times, opportunistic organisms like candida Albicans colonize on urethral catheters leading to Candida associated UTI and other complications like candiduria, a more dangerous condition as described by Kauffman et al.8
The Incidence of CAUTI in our study was 24.2%, which was less than the findings of 29.55% in one study by Sawsan et al.9 In their study, they considered patients from both Ward and ICU, so their incidence was high because of the large sample size as compared to our study in MICU only. Where the incidence of CAUTI due to candiduria was 19.2%, more than the rate of catheter-associated candiduria 0.7% or 0.4 per 1000 device days in one study by Deorukhkar et al.10
In our study, it was revealed that candida in CAUTI (19.5%) was the third most common organism next to staphylococci and E.coli, against the studies showing Candida albicans, the second commonest pathogen11 and higher than the previous study showing 10%-15%.8,12 As like another study by Dan Pawader et al,13 Candida Albicans was also the most common candida spp identified in our study.
Female patients 6 (75%)cases were more affected in our study due to candiduria, as noted same by other studies.8,14 Candiduria in CAUTI was mostly present in the age group of more than 40 years and up to 60 years (75 %) compared to the young age group of Tribal people, which indicates increasing age is a risk factor, correlated well with the previous studies.5,8,14 Tribal low socioeconomic group was more involved (62.5%) due to their poor hygiene practice, living style and presence of risk factors such as DM and SCA.
The rise in increasing of CAUTI in critical care units is mainly because of not adopting meticulous aseptic precaution during catheter insertion, infrequent change of catheter and improper catheter care.15 The presence of indwelling urethral urinary catheter is the most important risk factor for the development of Candida in CAUTI.16 Our study stated that most cases were present with the duration of catheterization up to 7 days (62.5%) correlated well with another study.7 In a French ICU study, the mean onset of candiduria after ICU admission was at 17 days, which was in 7 to 14 days in our study, indicates Candiduria occurs late in the hospital stay.17 It may be, because of the formation of biofilm in the mucosal surface and surfaces of catheters of the indwelling urinary catheter.
Mixed infections with other microorganisms (75%) were more common as compared to the single candidal infections in Candiduria with CAUTI.3 Staphylococci (37.5%) was the most common associated microorganism, followed by E coli (25%), Streptococci (25%) and Klebsiella(12.5%). Our results in favour of some studies, where it was found that mixed-species biofilms consisting of C. Albicans and Staphylococcus epidermidis, a common agent of catheter-related infections. Scanning electron microscopy revealed numerous physical interactions between the common organisms staphylococci, Streptococci and both yeasts and hyphae in mixed-species biofilms.18,19
Platt et al,20 in their study, documented, presence of diabetes as a risk factor for CAUTI due to two possibilities: an increased prevalence of perineal colonization by potential pathogens and an increased ability of the urine of some patients with diabetes to support microbial growth. In our study, Type 2 diabetes mellitus was an important risk factor for candiduria in CAUTI, accounting for 50 % of cases which correlates well with another previous study,7,9,13 followed by Sickle cell anaemia in 25% cases, Chronic kidney disease in 12.5% cases. Candiduria is a relatively rare finding in a structurally normal urinary tract.21 when kidneys are the most common site of disseminated candidiasis.22,23 Concomitant candidemia can occur in up to 8% of such patients.24
However some limitations of our study, first the study group was small and the results have to be confirmed with the larger study groups. Second, Candida isolates were not identified up to species level. Third, Antifungal susceptibility was not tested in our study.
Conclusion
Candida Albicans is the most common cause of nosocomial fungal catheter-associated urinary tract infection (CAUTI). In the present study, Our analysis precisely of this Tribal population brings several important and unique findings(risk factors of multi-organ involvement) than other study and population, which will modify or add in the development of some new or updated guidelines that might help critical care physicians in dealing with these patients on multiple organs supports, in the ICU. With the knowledge of the antibiotic resistance pattern of these pathogens, a new antibiotic policy will be developed to start antifungal empirically, thereby reduce the length of ICU stay, morbidity and mortality in these Tribal patients in the MICU of Tribal tertiary care centre.
We propose that a large clinical trial should be carried out over these population to investigate risk factors, the cause of mixed infection affecting multiple organs, the antifungal pattern and the prevention of Candiduria in CAUTI.
Acknowledgement: The authors thank all the
participants who have participated in the study.
Funding: No funding sources
Conflict of interest: No
Authors contribution :
Study conception, Design of methodology & Intellectual content: Mrs Monalisa Subudhi,
Dr P.A.T. Jagatheeswary & Dr Susanta Kumar Sahu,
Acquisition, Analysis and Interpretation of data: Mrs Monalisa Subudhi, Dr Sudhanshu Kumar das.
Drafting, Review, Editing of the manuscript: Dr Sudhanshu Kumar das, Mrs Monalisa Subudhi.
Critical revision & Final approval: Dr P.A.T. Jagatheeswary, Dr Susanta Kumar Sahu, & Dr Sudhanshu kumar das .
References:
-
Forbes BA, Weissfeld AS, Sahm DF. Diagnostic Microbiology, 13th edition, 2013; 919-930.
-
Device-associated module, Cauti: January 2014: available at: http://www.cdc.gov/nhsn/pdfs/pscmanual/7psccauticurrent.pdf; 26.07.2014; 16:39.
-
Poudel CM, Baniya G, Pokhrel BM . Indwelling catheter-associated urinary tract infection. J Inst Med 2008;30:3.
-
Bagchi, Jaitely NK. Microbiological evaluation of CACTI in a tertiary care hospital. Peoples J SC. Res, 2015; 8.
-
Padawer D, Pastukh N. Catheter-associated Candiduria: Risk factors, medical intervention, antifungal susceptibility. Am J Infect Control 2015;e1-e4.
-
Tambyah PA, Maki DG. Catheter-Associated Urinary Tract Infection is rarely symptomatic: a prospective study of 1497 catheterized patients. Arch Int Med 2004;160:678-82.
-
Gould CV, Umscheid CA, Agarwal RK, Kuntz G, David A. Pegues and Health Care infection control practices advisory committee. Guideline for prevention of Catheter-Associated Urinary Tract Infection 2009. Infect Control Hosp Epidemiol 2010;31:319-26.
-
Kauffman CA. Candiduria. Clin Infect Dis 2005; 41: S371-S376.
-
Omer SA, Zahran FE, Ibrahim A, Sidahmed LA, Almulhim KG. Risk Factors for Catheter-Associated Urinary Tract Infections (CAUTI) in Medical Wards and Intensive Care Units (ICU). J Microbiol Res 2020;10(1):1-5
-
Deorukhkar SC, Saini S, Raytekar NA, Sebastian DM. Catheter-associated urinary tract Candida infection in intensive care unit patients. J Clin Microbiol Biochem Technol 2016;2(1):015-17.
-
Laupland KB, Bagshaw SM, Gregson DB, Kirkpatrick AW, Ross T, Church DL. ICU-unit acquired UTI in a regional critical caresystem. Crit . care 2005;9:R60-5.
-
Bukhari ZA. Candiuria: a review of clinical significance and management. Saudi J Kid Dis Transpl 2008;19(3):350-60.
-
Padawer D, Pastukh N. Catheter-associated Candiduria: Risk factors, medical intervention, antifungal susceptibility. Am J Infect Control 2015; e1-e4.
-
Achkar JM, Fries BC. Candida infections of the genitourinary tract. Clin Microbiol Rev 2010;23: 253-273.
-
Greene L, Marx J, Oriola S. Guide to the elimination of catheter-associated urinary tract infections (CAUTIs). The Association for Professionals in Infection Control and Epidemiology (APIC) Washington, DC; 2008
-
Bhayani P, Rawekar R, Bawankule S, Kumar S, Acharya S, Gaidhane A, Khatib MN. Profile of urinary tract infection in a rural tertiary care hospital: Two-year cross-sectional study. J Datta Meghe Inst Med Sci Univ 2019;14:22-6.
-
Bougnoux ME, Kac G, Aegerter P, d’Enfert C, Fagon JY; CandiRea Study Group. Candidemia and candiduria in critically ill patients admitted to Intensive Care Units in France: Incidence, molecular diversity, management and outcome. Intensive Care Med 2008;34:292?9
-
Baillie GS, Douglas LJ. Role of dimorphism in the development of Candida albicans biofilms. J Med Microbiol 1999;48:671–679.
-
Jenkinson HF, Lala HC, Shepherd MG. Coaggregation of Streptococcus sanguis and other streptococci with Candida albicans. Infect Immunol 1990;58:1429–1436.
-
Platt R, Polk BF, Murdock B, Rosner B. Risk factors for nosocomial urinary tract infection. Am J Epidemiol 1986;124:977–85.
-
Bukhary ZA. Candiduria: a review of clinical significance and management. Saudi J Kidney DisTranspl 2008;19: 350-360.
-
Fisher JF, Kavanagh K, Sobel JD, Kauffman CA, Newman CA. Candida urinary tract infection: Pathogenesis. Clin Infect Dis 2011;52 Suppl 6:S437?51.
-
Lehner T. Systemic candidiasis and renal involvement. Lancet 1964;2:1414?6.
-
Kauffman CA, Vazquez JA, Sobel JD, Gallis HA, McKinsey DS, Karchmer AW. Prospective multicenter surveillance study of funguria in hospitalized patients. The National Institute for Allergy and Infectious Diseases (NIAID) Mycoses Study Group. Clin Infect Dis 2000;30:14?8.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License