IJCRR - 13(10), May, 2021
Pages: 62-67
Date of Publication: 19-May-2021
Print Article
Download XML Download PDF
Three-year Study of Hydatid Cyst at Unusual Sites in a Tertiary Care Centre
Author: Rukhsana Akhter, Duri Mateen, Naheena Bashir, Aiffa Aiman
Category: Healthcare
Abstract:Introduction: Hydatidosis is a zoonotic infection due to the larval stage of the tapeworm echinococcus. In adults, the liver represents the prevalent site and the lungs are the second commonest site. Although these are common sites, they can occur at any site including the spleen, pancreas, peritoneum, retroperitoneum, central nervous system, soft tissues and breast. Objective: To present the histopathological spectrum of hydatid cyst at unusual sites in our hospital over three years Methods: The present retrospective study was conducted in the Department of Pathology, SKIMS during a period of 3 years from July 2016 to June 2019 Results: A total no. of 12 cases that were diagnosed as Hydatid Cyst at unusual sites on HPE during the study period were included. The male and female ratio of incidence found to be 1:1.4. Maximum no of cases i.e. 3 occurred in the brain, 2 in the spleen, 2 in thigh, 1 each in breast, omentum, kidney, sacral ala, omentum and mediastinum. Conclusion: The hydatid cyst can present in any part of the body and no site is immune. These unusual locations often produce nonspecific symptoms. Hydatid cystic disease should always be suspected in all cystic lesions of radio imaging investigations particularly in endemic areas to prevent life-threatening complications and avoid unnecessary radical surgeries.
Keywords: Hydatid cyst, Zoonotic infection, Hydatidosis
Full Text:
INTRODUCTION
Hydatid disease or hydatidosis (HD) is caused by the larval stage of parasite Echinococcus Infestation by which can result in encystation in various organs commonly involved organs include the liver (75%) and lungs (15%), while the remaining 10% occurs in other body organs including spleen, kidney, pancreas, peritoneum, retroperitoneum, central nervous system, soft tissues, and the breast.1,2 Theoretically, it can occur at any site except teeth, hair, and nails.3 Possible dissemination through lymphatic channels accounts for cases with hydatid cysts at uncommon sites.4,5 The exact percentage of site involvement varies and the exact incidence of unusual locations is difficult to ascertain as they are only reported as case reports.6 Breast is a rare site of involvement accounting for only 0.27% of all cases of Hydatid diseas.7-9 Cerebral involvement is very rare(13%), and more common in children.10 Cerebral hydatid cysts are usually supratentorial, the infratentorial lesions are quite rare. Intracranial hydatid cysts are commonly solitary. Multiple intracranial cysts are rare.11,12 The incidence of hydatid disease of bone from various studies is reported to be 0.5–4%. About 60% of cases of bone hydatidosis affect the spine and pelvis, 28% the long bone and 8% the ribs and scapula.13 Skeletal lesions in hydatidosis tend to present with pain or pathological fractures following trivial injuries.14
MATERIALS AND METHODS
The present retrospective study was conducted in the Department of Pathology, SKIMS during a period of 3 years from July 2016 to June 2019. All the cases of hydatid that presented at unusual sites like kidney, spleen, retroperitoneum, brain, bone and omentum were included in the study. Specimens received were fixed in formalin; HP diagnosis was made on routine H&E sections.
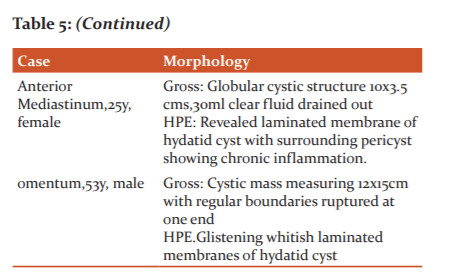
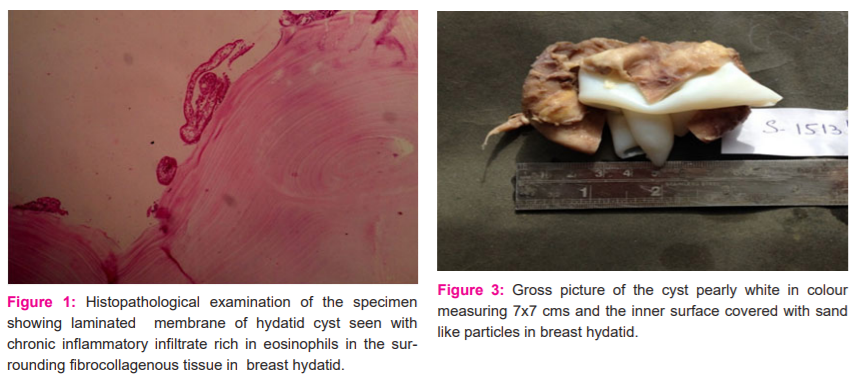
RESULTS
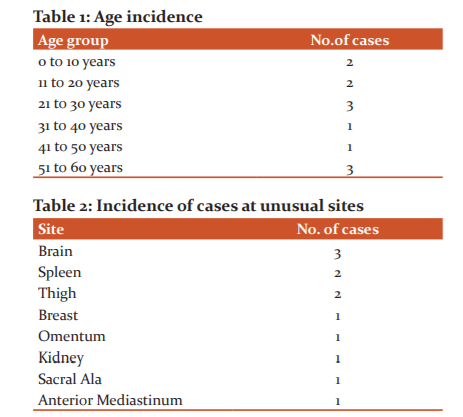
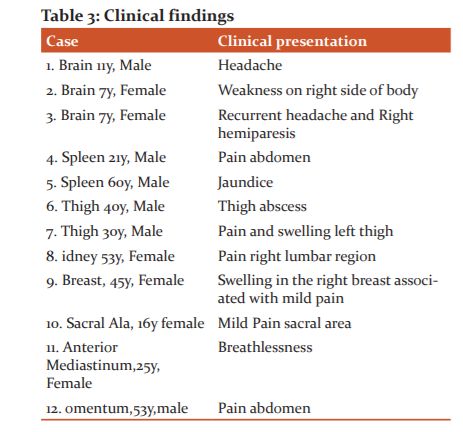
A total no. of 12 cases that were diagnosed as Hydatid Cyst at unusual sites on HPE during the study period were included. The youngest patient reported was 7years old, whereas the highest age was 60yrs (table 1). Males were 5 in number and females were 7; Male and female ratio of incidence found to be 1:1.4. Maximum no of cases i.e. 3 occurred in the brain, 2 in the spleen, 2 in thigh, 1 each in breast, omentum, kidney, sacral ala, and mediastinum (Table 2). The clinical presentation of the patients depended on o the site of the cyst ranging from headache and brain cysts and swelling and pain at the other sites (Table 3)
DISCUSSION
Hydatid disease is a parasitic infection caused by the larval form of Echinococcus granulosus and it is endemic in many sheep-raising communities, including South America, Spain, France and Italy, Eastern European countries.15,16 Our state, Kashmir, is endemic for hydatid disease.17 The adult echinococcus granulosus, a 5 mm long hermaphroditic tapeworm produces eggs that are released in the stool of infected canines.18,19 Animals such as cows, sheep and humans act as intermediate hosts and release embryos in the duodenum and enter into circulation by penetrating the intestinal mucosa.20 The liver acts as the first filter, while the lungs act as a second filter and thus, the liver is the most common site affected (75%), followed by lungs (15%), muscles (4%), kidney (2%), spleen (2%), bone (1%) etc. Only 15% of the embryos are free to develop cysts in other organs of the body.21,22
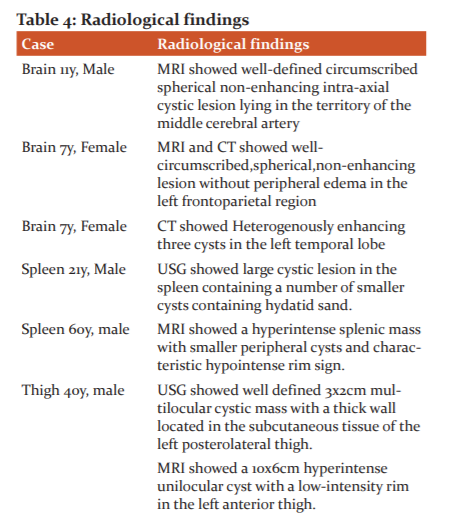
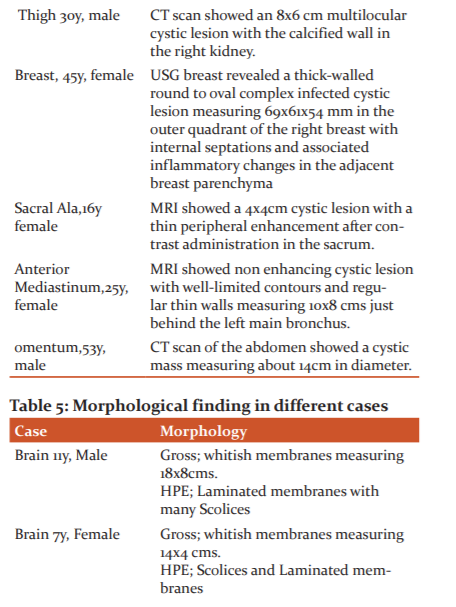
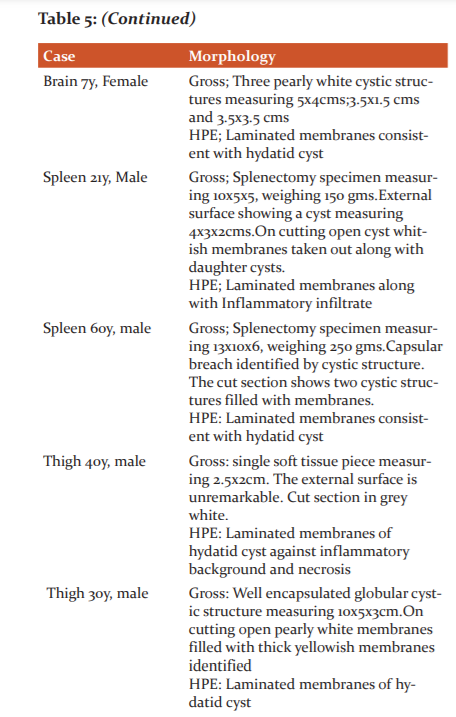
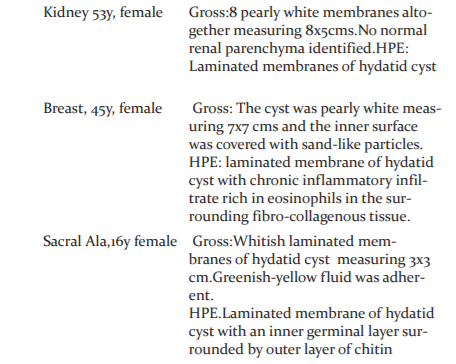
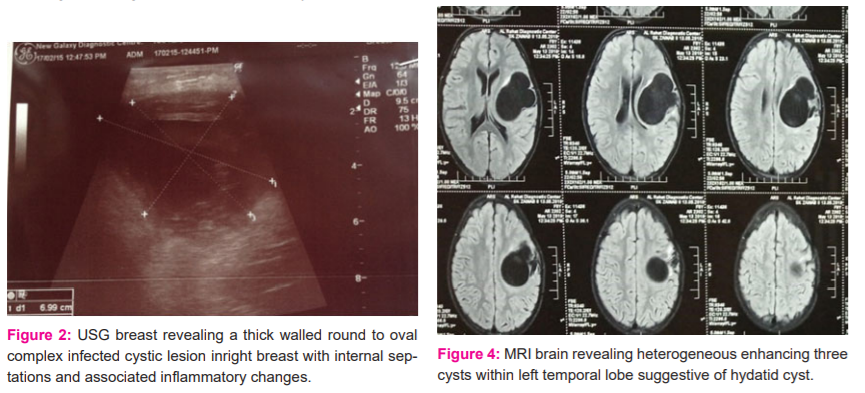
Hydatid cysts of the breast are extremely rare to find, even in endemic areas, accounting for only 0.27% of all cases.23 A total of 20 cases of breast hydatid were reported in Tunisia which forms the largest case series to date. The breast can be primarily infected or secondarily as a part of disseminated hydatidosis.23,24 Clinically, a hydatid cyst of the breast generally affects women in the age group of 30-50 years usually presenting with a painless, slowly increasing lump in the breast, of long duration without axillary lymphadenopathy. Ultrasonography and mammography are very effective in the evaluation of this mass. Despite its high cost, MR imaging has also been used in further evaluation of the mass.25 Serological investigations–indirect hemagglutination test, may be used for diagnosis and in the follow-up of patient.22 Preoperative diagnosis can be made by fine-needle aspiration cytology (scoliosis, hooklets or laminated membrane can be identified), but the use of fine-needle aspiration remains controversial with only a few studies describing this method without complications.21,26 but puncturing of the cyst may lead to an anaphylactic reaction and secondary cyst development due to spillage of hydatid fluid.27 Our case was a 45-year-old female, with swelling in the right breast with mild pain. On examination, there was swelling about 3x2 cms, soft to cystic inconsistency. FNAC was done which yielded 60 ml of clear fluid and a diagnosis of fibrocystic changes of the breast was made on microscopy.USG breast revealed a thick-walled round to oval complex infected cystic lesion measuring 69x61x54 mm in the outer quadrant of the right breast with internal septations and associated inflammatory changes in the adjacent breast parenchyma. The cyst along with the adjacent inflammatory tissue (pericyst) was removed subsequently. On histopathological examination of the specimen, the laminated membrane of the hydatid cyst was seen with chronic inflammatory infiltrate rich in eosinophils in the surrounding fibro collagenous tissue.
Cerebral involvement is very rare(13%), and more common in children.10 Cerebral hydatid cysts are usually supratentorial, the infratentorial lesions are quite rare. Intracranial hydatid cysts are commonly solitary. Multiple intracranial cysts are rare.11 Patients with intracranial hydatid cysts usually present with focal neurological deficit and features of raised intracranial pressure? the latter may be due to the large size or due to interference with the pathway of CSF. The typical intracranial hydatid cysts caused by Echinococcus granulosus, present as well defined solitary cystic lesions in the middle cerebral artery territory in parietal lobes, although they can be seen in any location including skull vault, extradural, intraventricular, meningeal, posterior fossa and brainstem.28 Operative diagnosis of hydatid cysts can be made by USG and confirmed by a CT scan. Magnetic resonance imaging is also of considerable value in intracranial hydatidosis. Surgically, intact cyst excision is the ideal treatment. Medical treatment with albendazole seems to be beneficial both preand postoperatively.11,29 The definitive diagnosis can be made by histopathologic examination.30 All three cases in our study were children with cerebral involvement. One case had multiple (three) cysts. Preoperative diagnosis was made on MRI. Surgically intact cysts were excised and histopathology was consistent with hydatid cyst. Incidence of hydatid disease of bone from various studies is reported to be 0.5.12
Primarily isolated bone hydatid is a very rare occurrence. The lesions in bone may lie dormant for 10 to 20years.31 The spine is the common site of infection.32 Hydatid disease of the spine usually spreads over the spine by direct extension from pulmonary, abdominal or pelvic infestation and most commonly affects the thoracic (52%), followed by the lumbar (37%) and then the cervical and sacral spine.33 Skeletal lesions in hydatidosis tend to present with pain or pathological fractures following trivial injuries.14 The most common radiological manifestation of skeletal hydatid disease is a lucent expansile lesion with cortical thinning. Bone hydatid disease lacks a typical clinical appearance and image characteristics on Xray or CT scan are similar to those of tuberculosis, metastases, giant cell tumour or bone cysts.34 Magnetic resonance imaging shows distinctive diagnostic features of bone hydatid disease, especially in the spine. The only de?nitive treatment when a bone is involved is complete resection of the involved area with a wide healthy margin. The combination of antihelminthic therapy, wide resection and the use of polymethylmethacrylate (PMMA) gives the best outcome in the treatment of bone hydatidosis.33 Our case was a young 16-year-old female with mild pain in the sacral region. She was already operated on in the past for hydatid cyst liver. Intraoperative findings revealed a large cyst with daughter cysts in the sacral ala area. HPE revealed laminated membranes of hydatid cyst.
The prevalence of splenic involvement ranges between 0.9% and 8%.35-37 Splenic HC generally develops using systemic dissemination or intraperitoneal spread from a ruptured liver cyst. Isolated splenic involvement is not very frequent.38 Splenic hydatidosis should be differentiated from other splenic cystic lesions, such as epidermoid cyst, abscess, hematoma, post-traumatic pseudocyst, neoplasms like lymphangioma and haemangioma.39,40 We had two cases of splenic hydatid cyst. One patient was a young 21-year-old male with disseminated hydatid disease. The second patient was elderly male 60 years and was being evaluated for CBD growth. On HPE he was found to be having two hydatid cysts in the spleen along with Adenocarcinoma of the Gall bladder in the background of Xanthogranulomatous cholecystitis.
Soft-tissue HC occurs in 0.5-4.7% of patients living in endemic areas38,41, the growth of the cyst within a muscle is difficult due to the contractility of muscles and presence of lactic acid.36,38 HC has an affinity for muscles of the neck, trunk and limbs. The increased vascularity and decreased activity of these muscle groups is the suggested cause for this increased affinity.36,38 We had two cases of soft tissue hydatid both in the thigh. One case presented as a thigh abscess. Other case had radiology suggestive of hydatid with positive hydatid serology.
Renal involvement is rare (1-4%).36,38 It is reported as the common site following liver and lung in several articles.42 They are however mostly solitary and located at the upper pole or cortex.38 Multilocular HCs can be misdiagnosed as simple renal cysts, cystic nephroma, and cystic variants of renal cell carcinoma38 and infected HCs can be misdiagnosed as renal abscess.38 The mediastinal hydatid cyst is uncommon but it should be included in the differential diagnosis of the mediastinal cyst in endemic parts of the world.43 The omental and retroperitoneal hydatid cysts are very uncommon, but these cysts can become huge.44
CONCLUSION
The hydatid cyst can present in any part of the body and no site is immune. These unusual locations often produce nonspecific symptoms. Hydatid cystic disease should always be suspected in all cystic lesions of radio imaging investigations, particularly in endemic areas to prevent life-threatening complications and avoid unnecessary radical surgeries.
References:
1. Engin G, Acunas B, Rozanes I, Acunas G, Hydatid disease with unusual localization. Eur Radiol 2000;10:1904-12.
2. Kiresi DA, Karabacakoglu A, Odeh K, Karakose S. Uncommon locations of hydatid cysts, Acta Radiol 2003;44:622-36.
3. Hamamci EO, Besim H, Korkmaz A. Unusual locations of hydatid disease and surgical approach, ANZ. J Surg 2004;74: 356-60.
4. Saidi F, Nyhus LM, Beker JR, Fsicher JE. Treatment of echinococcal cyst. Mastery of Surgery. 3rd Edn. Little, Brown and Company 1998:1035–2.
5. Prousalidis J, Tzardioglou K, Sgouradis L, Katsohis C, Aletras H. Uncommon sites of hydatid disease. World J Surg 1998;22:17–22.
6. Zippi M, Siliquini F, Fierro A. Diffuse abdominal hydatidosis: role of magnetic resonance imaging.ClinTer2007;158(3):231–3.
7. Vege A, Ortega E, Cavada A. Garijo F. Hydatid cyst of the breast: Mammographic findings. Am J Roentgenol 1994;162:825-826.
8. Tukel S, Erden I, Ciftci E, Kocak S. Hydatid cyst of the breast. MR imaging findings (letter). Am J Roentgenol 1997;168:1386-7.
9. Taori KB, MahajanSM, Hirawe SR,Mundhada RG. Hydatid disease of the breast. Ind J Rad Imag 2004;14(1):64-65.
10. Aras AM, Serarslan Y, Davran R, Evirgen O, Yilmaz N. A medically treated multiple cerebral hydatid cyst diseases. J Neurosurg Sci 2010 ?54(2):79–82.
11. CiureaAV, FountasKN, ComanTC. Longterm surgical outcome in patients with intracranial hydatid cyst. Acta Neurochir (Wien) 2006?148:421–6.
12. Torricelli P, Martinelli C, Biagini R, Ruggieri P, De Cristofaro R. Radiographic and computed tomographic findings in hydatid disease of bone. Skeletal Radiol 1990?19:435–9.
13. Yildiz Y,Bayrakci K,Altay M, Saglik Y. The use of polymethylmethacrylate in the management of hydatid disease of bone. J Bone Joint Surg Br 2001?83(7):1005–8.
14. Wani R, Wani I, Malik A, Parray F, Wan A, Dar A. Hydatid disease at unusual sites. Int J Case Rep Images 2012;3:1-6.
15. Grosso G, Gruttadauria S, Biondi A, Marventano S, Mistretta A. Worldwide epidemiology of liver hydatidosis including the Mediterranean area. World J Gastroenterol 2012;18(13):1425–1437
16. Kaplan M, Aygen E, Özyurtkan MO, Bakal Ü. Cystic echinococcosis cases in Firat University Hospital between 20052007. F?rat Uni Health Sci Med J 2010; 24:109-13.
17. Khuroo MS. Hydatid disease: Current status and recent advances. Ann Saudi Med2002;22:56–4.
18. Mushtaque M, Mir MF, Malik AA, Arif SH, Khanday SA, Dar RA. Atypical localization of hydatid disease: Experience from a single institute. Niger J Surg 2012;18:2-7.
19. ?ulafi? DJ, Kati?-radivojevi? s, Kerkez M, Vuk?evi? M, rankovi? V, stefanovi? D. Liver cystic echinococcosis in humans-a study of 30 cases. Helminthologia 2007;44:157-61.
20. Garcia LS, Shimizu RY, Bruckner DA. Sinus tract extension of a liver hydatid cyst and recovery of diagnostic hooklets in sputum. Am J Clin Pathol 1986;85:519-521.
21. Das DK, Choudhury U. Hydatid disease: an unusual breast lump. J Indian Med Assoc 2002;100: 327–328.
22. Mujawar P, Suryawanshi KH, Nikumbh DB. Cytodiagnosis of isolated primary hydatid cyst of the breast masquerading as a breast neoplasm: A rare case report. J Cytol 2015;32: 270-272.
23. Moazeni-Bistgani M. Isolated hydatid cyst of the breast that developed after breastfeeding. J Surg Case Rep J Surg Case Rep 2016;2016(5): rjw071.
24. Ouedrago EG. Hydatid cyst of the breast: 20 cases. J Gynecol Obstet Biol Reprod 1986;15: 187-194.
25. Tukel S, Erden I, Ciftci E, Kocak S. Hydatid cyst of the breast. MR imaging findings (letter). Am J Roentgenol 1997;168: 1386-7.
26. Mirdha BR, Biswas A. Echinococcosis: presenting as palpable lumps of the breast. Indian J Chest Dis Allied Sci 2001; 43: 239–241.
27. Mirdha BR, Biswas A. Echinococcosis: presenting as palpable lumps of the breast. Indian J Chest Dis Allied Sci 2001;43: 239–241.
28. Ba'assiri A, Haddad FS. Primary extradural intracranial hydatid disease: CT appearance. Am J Neuroradiol 1984;5(4):474–5.
29. Akdemir G, Daglioglu E, Seçer M, Ergüngör F. Hydatid cysts of the internal acoustic canal and jugular foramen. J Clin Neurosci 2007;14(4):394–6.
30. Tüzün M, Hekimoglu B. CT findings in skeletal cystic echinococcosis. Acta Radiology 2002 Sep;43(5):533–8.
31. Hooper J, McLean I. Hydatiddiseaseofthefemur: report of a case. J Bone Joint Surg Am 1977;59(7):974–6.
32. Sapkas GS, Stathakopoulos DP, Babis GC, Tsarouehas JK. Hydatid disease of bones and joints: 8 cases followed for 4–16 years. Acta Orthop Scand 1998;69(1):89–4.
33. Karadereler S, Orakdögen M, Kiliç K, Ozdogan C. Primary spinal extradural hydatid cyst in a child: Case report and review of the literature. Eur Spine J 2002;11:500–3.3 3.
34. Martin J, Marco V, Zidan A, Marco C. Hydatid disease of the soft tissues of the lower limb: findings in three cases. Skeletal Radiol 1993?22(7):511–4.
35. Ertabaklar H, Dayan?r y, Ertu? s. research to investigate the human cystic echinococcosis with ultrasound and serologic methods and educational studies in different provinces in Ayd?n/ turkey. Turkish J Paras 2012; 36: 142-6.
36. Demirci E, Altun E, Çal?k M, suba?? ID, ?ipal s, Gündo?du ÖB. Hydatid cyst cases with different localization: region of Erzurum. Turkish J Parasitology 2015;39:103-7.
37. Özekinci S, Bak?r ?, M?zrak B. Evaluation of cystic echinococcosis cases given a histopathologic diagnosis from 2002 to 2007 in Diyarbakir. Turkish J Paras 2009;33:232-5.
38. Polat P, Kantarci M, Alper F, suma s, Koruyucu MB, Okur A. Hydatid disease from head to toe. Radiog 2003;23:475-94.
39. Sawarappa R, Kanoi A, Gupta M, Pai A, Khadri s. Isolated splenic hydatidosis. J Clin Diagn Res 2014;8:nD03-nD04.
40. Pukar MM, Pukar SM. Giant solitary hydatid cyst of spleen- A case report. Int J Surg Case Reports 2013;4:435-7.
41. Sachar S, Goyal S, Goyal S, Sangwan S. uncommon locations and presentations of hydatid cyst. Ann Med Health Sci Res 2014;4:447-52.
42. Geramizadeh B. unusual locations of the hydatid cyst: A review from Iran. Iran J Med Sci 2013;38:2-14.
43. Traibi A, Atoini F, Zidane A, Arsalane A, Kabiriel H. Mediastinal hydatid cyst. J Chin Med Assoc 2010;73:3-7.
44. Rathod KJ, Lyndogh S, Kanojia RP, Rao KL. Multiple primary omental hydatids: rare site for a common infestation. Trop Gastroenterol 2011;32:134-6.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License