IJCRR - 13(9), May, 2021
Pages: 146-149
Date of Publication: 07-May-2021
Print Article
Download XML Download PDF
Evaluation of Incidence, Distribution and Etiopathology of Cervical Lymphadenopathy in Patna Population
Author: Mukesh Kumar, Ram Prasad Sah, Abhinav Raj Gupta
Category: Healthcare
Abstract:Introduction: The lymphatic system is a network of tissues and organs that eliminate toxins and other waste products from the body. The chief function of the lymphatic system is to transport lymph all through the body. Lymphadenopathy may be described as an enlargement of the lymph node due to swelling of the histiocytes in the sinus, hyperplasia of lymph follicles or invasion of tumour cells. Cervical lymphadenopathy refers to cervical lymph nodes measuring more than 1 cm in diameter. Objective: The present study was conducted to evaluate the incidence of cervical lymphadenopathy and to describe the distri�bution of the various etiologies of cervical lymphadenopathy in all age groups. Methods: This study was conducted on 100 patients more than 12 years of age presenting to the O.P.D with neck swelling for more than 3 weeks. All the cases were confirmed histopathologically with FNAC of the involved node. Results: A total of 100 subjects presenting with a complaint of neck swelling for more than 3 weeks were included in the study. All the subjects were between the age group of 14 years to 55 years. The present study comprised 65 males and 35 females. 20 out of 100 were diagnosed with neoplastic nodes, whereas 80 were diagnosed with non-neoplastic nodes. In the non-neoplastic variety, the majority of the patient's had tuberculous lymphadenopathy, In the neoplastic variety, 06 had Hodgkin's lymphoma, 04 had Non-Hodgkin's lymphoma and 10 patients present with lymphadenitis associated with secondaries. Conclusion: Cervical lymphadenopathy may pose a special challenge to the attending physicians. Sole dependence on clini�cal presentation may lead to a flawed diagnosis. FNAC is a simple, secure, dependable and non-invasive procedure for the diagnosis of cervical lymphadenopathy. The present study may act as the foundation of awareness regarding the distribution of lymphadenitis, their mode of presentation and predilection for different strata.
Keywords: Cervical Lymphadenopathy, Lymph Nodes, Lymphoma, Reactive Lymphadenitis, Tuberculosis
Full Text:
INTRODUCTION
The lymphatic system is a network of tissues and organs that eliminate toxins and waste products from the body. The chief function of the lymphatic system is to transport lymph all through the body. It primarily comprises lymphatic vessels, which are connected to lymph nodes along with tonsils, adenoids, spleen and thymus.1 Lymph nodes are located at the convergence of major blood vessels, and a human body comprises around 800 nodes distributed around the neck, axilla, thorax, abdomen, and groin. Around 300 nodes are located in the neck, entrenched in the soft tissue of the neck partly or surrounded by fat.2 Lymph nodes act as a filter for lymph, phagocytose foreign materials including micro-organisms, help in proliferation and circulation of T and B cells and enlarge subsequently to local antigenic stimulation. 3
The American Academy of Otolaryngology has classified the cervical nodes into Level I- submental and submandibular; Level II- upper jugular; Level III- middle jugular; Level IV- lower jugular; Level V- posterior triangle; Level VI- anterior compartment and Level VII- superior mediastinal. Based on their location in the neck, they may be classified as circular/ horizontal and vertical. The circular chain of nodes comprises submental, submandibular, facial, preauricular, postauricular, occipital, anterior cervical, inferior hyoid, prelaryngeal, pretracheal and superficial cervical nodes. The vertical chain comprises prelaryngeal, pretracheal, paratracheal and retropharyngeal nodes.4
They are kidney-shaped, vary in size from 1-2 cm and are encapsulated by fibrous tissue, however, may be considered pathological if they increase in size, lose their kidney/ oval shape and become round in shape, with the loss of hilar fat, asymmetrical thickening of the cortex. Enlargement of the lymph node may be due to swelling of the histiocytes in the sinus, hyperplasia of lymph follicles or invasion of tumour cells.5 This condition is described as lymphadenopathy and may be caused by the invasion or propagation of either inflammatory or neoplastic cells into the lymph node. Etiological factors considered responsible for lymphadenitis include malignancies, inflammatory conditions; infections; autoimmune disorders; iatrogenic causes (phenytoin and vaccines). Based on the distribution, it may be classified as localized, generalized, and dermatopathic, based on the duration, it may be acute (2 weeks), subacute (4–6 weeks) and chronic (> 6 weeks duration).6
Cervical lymphadenopathy refers to cervical lymph nodes measuring more than 1 cm in diameter. The Head and neck region is considered a common site for lymphadenopathy. The presence of the same is indicative of underlying pathology ranging from a trifling infection (benign lymphoid hyperplasia or reactive lymphadenitis) to a metastatic malignancy. Etiology of cervical lymphadenopathy may be multifactorial including conditions like infections, malignancies, autoimmune disorders, medications, etc. Infectious conditions comprise Epstein Barr virus infection, Toxoplasmosis, Cytomegalovirus, Initial stages of HIV infection, Cat scratch disease Pharyngitis due to group A Streptococcus, Gonococcus, Tuberculosis lymphadenitis, Secondary syphilis, Hepatitis B, Rubella, Brucellosis, Typhoid fever. Autoimmune diseases comprise Lupus erythematosus, Sjogren’s syndrome, Dermatomyositis, etc. Malignant conditions include Lymphoma, Leukemia, Kaposi’s sarcoma, and Metastasis. Miscellaneous conditions comprise Gaucher’s disease, Niemann Pick disease, Fabry’s disease, Hyperthyroidism, Histiocytosis X, Hypertriglyceridemia, Angiofollicular lymph node hyperplasia, Angioimmunoblastic lymphadenopathy, Kikuchi’s lymphadenitis, Kimura’s disease, Sarcoidosis, Kawasaki disease, Silicosis/ berylliosis, etc. Medications associated with lymphadenopathy are Penicillin, Allopurinol, Phenytoin, Atenolol, Primidone, Captopril, Pyrimethamine, Carbemazipine, Quinidine, Cephalosporins, Sulfonamides, Gold, Sulindac, Hydralazine. Acute infective lymphadenopathy is usually self-resolving and can be managed with antibiotic therapy.7
During a thorough clinical examination of lymphadenopathy, the following things should be evaluated: Location: the site of the lymph node or the type involved should be examined carefully along with the number of nodes involved (generalized or localized; unilateral or bilateral); Size: Cervical lymph nodes and axillary nodes are atypical if > 1 cm, as compared to supraclavicular > 0.5cm, and inguinal nodes >1.5 cm; Consistency: a firm lymph node is indicative of an infective condition whereas a stony hard node indicates malignancy; Pain: can is a non-specific finding, however, may be a sign of inflammation or an acute reaction to an infection.8 The present study was carried out to evaluate the incidence of cervical lymphadenopathy and to describe the distribution of the various etiologies of cervical lymphadenopathy in all age groups.
MATERIALS AND METHODS
This study was carried out on 100 patients who attended the Out-Patient Department of Dentistry, Sri Krishna Medical College and Hospital, Muzaffarpur, Bihar with enlarged cervical lymph nodes; from August 2019 to February 2020.
Patients >12 years presenting to the OPD with neck swelling for more than 3 weeks were included in the study. Patients with neck swelling less than 3 weeks were excluded from the study. All the cases were confirmed histopathologically with Fine Needle Aspiration Cytology of the involved node.
All the data was recorded in an excel sheet. Patients distributed according to age, gender and carcinogenicity. Chi-square test was applied. [Ref no. 645/2019/SKMCH]
RESULTS
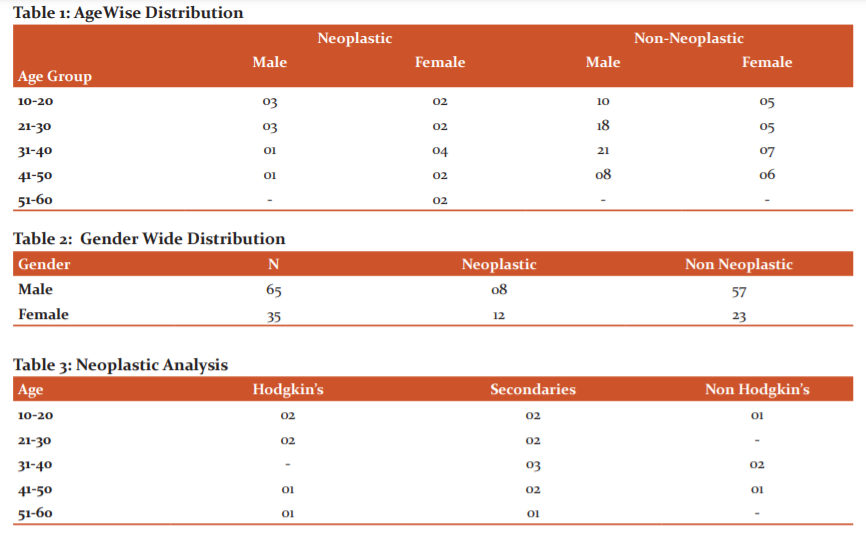
A total of 100 subjects presenting with a complaint of neck swelling for more than 3 weeks were included in the study. All the subjects were between the age group of 14 years to 55 years. 20 patients belonged to the age group of 10-20 years; 28 patients belonged to 21-30 years; 33 subjects belonged to 31-40 years; 17 patients belonged to 41-50 years and 02 patients belonged to 51-60 years (Table 1).
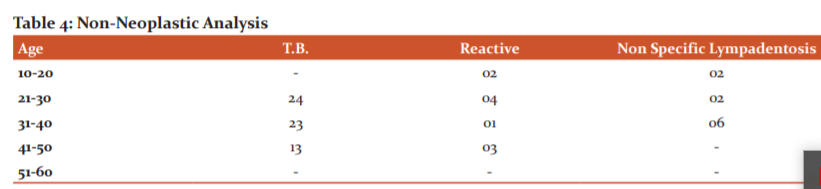
The present study comprised 65 males and 35 females (Table 2). Twenty out of 100 were diagnosed with neoplastic nodes, whereas 80 were diagnosed with non-neoplastic nodes. 57 out of these 80 non-neoplastic subjects were males, whereas 23 were females. 08 out of these 20 neoplastic subjects were males, whereas 12 were females. In the non-neoplastic variety, the majority of the patient’s had tuberculous lymphadenopathy, i.e 60 subjects; 10 had reactive lymphadenitis and 10 had non-specific lymphadenitis (Table 3). In the neoplastic variety, 06 had Hodgkin’s lymphoma, 04 had Non-Hodgkin’s lymphoma and 10 patients present with lymphadenitis associated with secondaries (Table 4).
DISCUSSION
Hundred histopathologically confirmed cases of cervical lymphadenitis were included in the study. The majority of the cases were below 50 years of age, i.e. 98 patients were between 14-50 years and only 02 patients were above 50 years. Cervical lymphadenopathy is commonly seen amongst young individuals. The incidence of lymphadenopathy decreases considerably with age.9 Majority of the subjects in the present study comprised males, being 65 with only 35 females. A study on 112 patients with cervical lymphadenopathy, out of which 79 were males and 33 were females.10 20 out of 100 were diagnosed with neoplastic nodes, whereas 80 were diagnosed with non-neoplastic nodes. Results are similar to previous study which showed that the incidence of non-neoplastic and neoplastic lesions by 90.6% and 9.4% respectively. 11
In the non-neoplastic variety, the majority of the patient’s had tuberculous lymphadenopathy, i.e 60 subjects; 10 had reactive lymphadenitis and 10 had non-specific lymphadenitis. The findings were similar to the study carried out by Jha et al. 2001 who conducted a study on 94 cases with cervical lymphadenopathy and found that tuberculosis accounted for enlargement in 60 cases.12 It has been reported that tuberculosis persists to be a ubiquitous health problem in developing countries affecting around 1.5% of the Indian population. Tuberculous adenitis is the most common cause of cervical lymphadenitis and involves upper and anterior deep cervical nodes followed by sub-mandibular and sub-mental lymph nodes.13 The condition is referred to as “scrofula” and primarily affects the cervical lymph nodes, followed by axillary and inguinal nodes. Associated systemic symptoms include unexplained weight loss, malaise, fever, cough or hemoptysis. TB lymph nodes may be multiple, matted, hard to fluctuant with draining sinuses, however, in the early stages; the consistency of the nodes may be discrete, firm, and rubbery. Jones and Campbell (1962) described stages of TB lymphadenitis as follows: enlarged, firm, mobile, discrete nodes; large rubbery nodes fixed to surrounding tissue; central softening abscess; collar stud formation and sinus tract formation.14 Only 10 subjects had reactive lymphadenitis, which may be attributed to bacterial, viral infections, dental infections and surgical procedures in the head and neck region. 10 subjects had nonspecific lymphadenitis, which is commonly seen in children and may occur secondary to bacterial infections (Staphylococcus aureus and beta-hemolytic Streptococcus); viral infections or inflammation of the draining sites or direct inflammation of the lymph nodes. These are self-resolving and do not require treatment.15
In the neoplastic variety, 06 had Hodgkin’s lymphoma, 04 had Non-Hodgkin’s lymphoma and 10 patients present with lymphadenitis associated with secondaries. Hodgkin’s lymphoma is a malignant neoplasm of cells of lymphoid tissue (B cell-derived cancer) and is the commonest of malignant lymphomas. Cervical lymph nodes are involved in the majority of cases followed by mediastinal, axillary, para-aortic and inguinal nodes. Initial symptoms may be non-specific and may include pruritus, fever, weakness, malaise, weight loss and night sweats.16
Non-Hodgkin’s Lymphoma originates from B cell precursors, mature B cells, T cell precursors, and mature T cells. It may be associated with Epstein-Barr virus (Burkitt lymphoma), Human T-cell leukaemia virus type 1, Hepatitis C virus, Helicobacter pylori; drugs like phenytoin, digoxin, TNF antagonists, immune-deficiency conditions like Wiskott-Aldrich syndrome; autoimmune disorders like Sjogren syndrome, rheumatoid arthritis, and Hashimoto thyroiditis.17
Secondary involvement of lymph nodes in the cervical region is very common and carcinoma tends to metastasize to regional nodes. Patients usually present with painless swelling, however, the presence of pain is indicative of involvement of nerves and surrounding structures. Patients usually present with symptoms like anorexia, weight loss or weakness, hoarseness of voice, etc. These nodes are initially mobile and firm later become hard and get matted together. They are usually painless and not tender.18
Conclusion
Cervical lymphadenopathy may pose a special challenge to the attending physicians. The present study reports majority of the patients with cervical lymphadenopathy belong to the non-neoplastic category, tuberculosis being the most predominant type. Sole dependence on clinical presentation may lead to a flawed diagnosis. FNAC is a promising tool to diagnose the condition and start the management accordingly. It is an easy, simple, safe, reliable and non-invasive procedure for the diagnosis of cervical lymphadenopathy. The present study may act as the foundation of awareness regarding the distribution of lymphadenitis, their mode of presentation and predilection for different strata.
Type of study: original research paper
Conflicts of interest- none
Acknowledgement- Self-financed- no funding by anyone
References:
-
Mandal A, Pan K, Maity PK, Panchadhyayee S, Sarkar G, Chakraborty S, et al. Isolated Mediastinal Lymphadenopathy – Etiological Analysis. Int J Cur Res Rev 2014;06:14-19.
-
Gupta R, Dewan D, Suri J. Study of incidence and cytomorphological patterns of tubercular lymphadenitis in a secondary care level hospital of Jammu Region. Indian J Pathol Oncol 2015;2:161?4.
-
Bazemore AW, Smucker DR. Lymphadenopathy And Malignancy. Am Fam Physician 2002;66:2103-2110.
-
Ramadas AA, Jose R, Varma B, Chandy Ml. Cervical Lymphadenopathy: Unwinding The Hidden Truth. Dent Res J (Isfahan) 2017;14:1:73-78.
-
Quadri KS, Hamdani NH, Shah P, Lone MI, Baba KM. Profile Of Lymphadenopathy In Kashmir Valley; A Cytological Study. Asian Pacific J Cancer Prevention 2012;13(1):3621-5.
-
Misra D, Panjwani S, Rai S, Misra A, Prabhat M, Gupta P, Talukder SK. Diagnostic Efficacy Of Color Doppler Ultrasound In Evaluation Of Cervical Lymphadenopathy. Dent Res J 2016;13:217-24.
-
Singh S, Arora I, Singh S, Khan DR.Cytological Diagnosis of Lymphadenopathy on FNAC - A study from rural tertiary care. J Dental Med Sci 2018;17:7:75-83
-
Malhotra AS, LahoriM, Nigam A, Khajuria A. Profile of lymphadenopathy: An institutional-based cytomorphological study. Int J App Basic Med Res 2017;7:100-3.
-
Mitra SK, Misra RK, Rai P. Cytomorphological patterns of tubercular lymphadenitis and its comparison with Ziehl-Neelsen staining and culture in eastern up. (Gorakhpur region): Cytological study of 400 cases. J Cytol 2017;34:139-43.
-
Mili Mk, Phookan J. A Clinico- Pathological Study Of Cervical Lymphadenopathy. Int J Dent Med Res 2015; 1:5: 24-27.
-
Ullah S, Shah SH, Rehman AU, Kamal A, Begum N. Tuberculous Lymphadenitis In Afghan Refugees. J Ayub Med Coll Abbottabad 2002;14:2:22-33.
-
Jha BC, Dass A, Nagarkar NM. Cervical Tuberculous Lymphadenopathy: Changing Clinical Pattern And Concepts In Management. Postgrad Med J 2001;77:185-187.
-
Chaudhary V, Ali MA, Mathur R. Tubercular Cervical Lymphadenitis: Experience Over A Four Year Period. Int J Curr Res Rev 2014;6(6):93-99.
-
Thakkar K, Ghaisas SM, Singh M. Lymphadenopathy: Differentiation Between Tuberculosis And Other Non-Tuberculosis Causes Like Follicular Lymphoma. Front Public Health 2016;4:31.
-
Pulgaonkar R, Chitra P, Moosvi Z. Benign Reactive Lymphadenopathy Associated With Submandibular Gland Enlargement During Orthodontic Treatment. J Oral Maxillofac Pathol 2017;21:181.
-
Küppers R, Engert A, Hansmann Ml. Hodgkin Lymphoma. J Clin Invest. 2012; 122:10: 3439-3447.
-
Sapkota S, Shaikh H. Non-Hodgkin Lymphoma. [Updated 2020 Sep 4]. In: Statpearls [Internet]. Treasure Island (Fl): Statpearls Publishing; 2020 Jan-
-
Som PM. Detection Of Metastasis In Cervical Lymph Nodes: Ct And Mr Criteria And Differential Diagnosis. Ajr Am J Roentgenol 1992;158(5): 961-9.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License