IJCRR - 13(9), May, 2021
Pages: 142-145
Date of Publication: 07-May-2021
Print Article
Download XML Download PDF
Predicting the Outcome of Treatment of Non-Traumatic Intracerebral Haemorrhage
Author: G. Kariev, A. Mamadaliev, B. Isakov, M. Khakimov, A. Kadirov
Category: Healthcare
Abstract:Introduction: Predicting the outcome of conservative and surgical treatment of non-traumatic intracerebral haemorrhage is an urgent task of modern neurology and neurosurgery, as it allows timely determination of the optimal treatment tactics. Objective: For preliminary prediction of the outcome of treatment based on our observations and previously proposed by foreign and domestic authors of forecasting methods, we have compiled and proposed scales that include the most extensive informa�tion about the patient's current state. Methods: Based on the scales and programs proposed by the authors and from our own observation experience, we have proposed several point parameters in the form of a scale. Results: When assessing the results of treatment according to RSHIG, it was revealed that an excellent result was observed most of all in young patients (38.9%), less in middle-aged and elderly patients (28.1% and 22.2%, respectively) and the lowest rates in this aspect were revealed in elderly patients - 5.6%. Conclusion: This scale has been introduced into the practice of the Andijan branch of the Republican Scientific Center for Emergency Medical Aid and the clinic of the Andijan State Medical Institute
Keywords: Non-traumatic intracerebral haemorrhage, Prediction, Scale, Treatment, Outcome, Moderate neurological deficit
Full Text:
INTRODUCTION
Non-traumatic intracerebral haemorrhage has become not only a medical but also a social and economic problem, since it ranks third among the causes of death and first among the causes of disability - up to 80% of patients who have suffered a stroke become disabled.1
Stroke affects 0.2% of the population every year. WHO registers about 20 million strokes annually. 1/3 of them die within the first year, a third become permanently disabled, and only 26% of patients return to an active social life.2 If we add two-thirds of surviving patients to the rest of the huge contingent of stroke survivors (about 1% of the population), of which half are disabled, the significance of stroke as a separate nosology leading to mortality and disability becomes enormous.3
MATERIALS AND METHODS
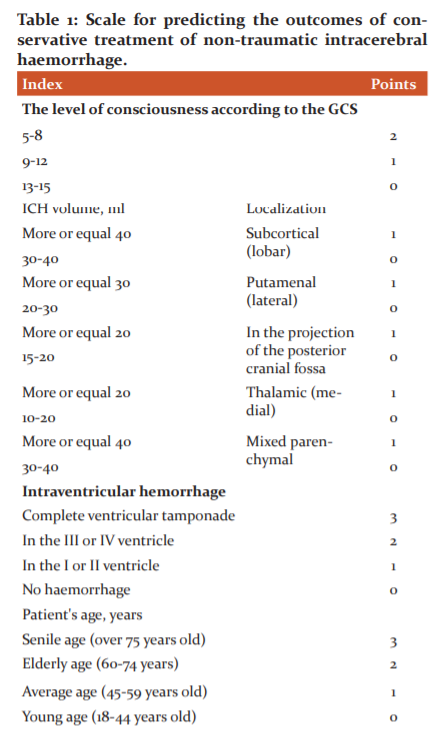
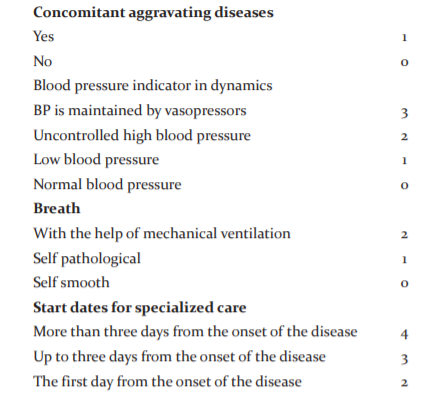
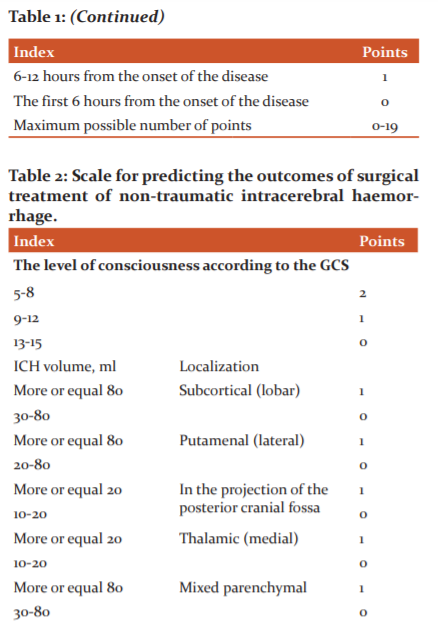
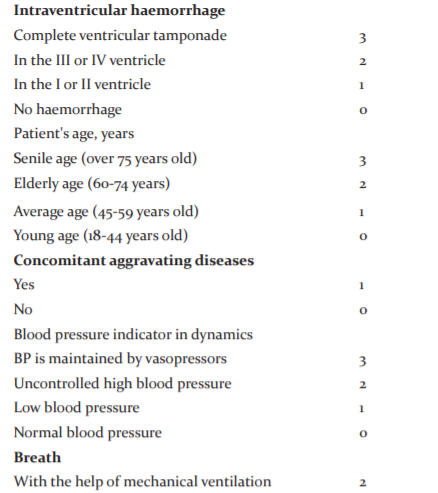
For preliminary prediction of the outcome of treatment based on our observations and previously proposed we have compiled and proposed scales that include the most extensive information about the patient's current state, that is, his consciousness, age, volume and depth of haemorrhage, the presence of aggravating concomitant somatic pathologies and the state of vital body functions.4-6
Parameters
15-19 points - an unfavourable outcome;
10-14 points - gross neurological deficit;
5-9 points – moderate neurological deficit;
0-4 points - a favourable outcome (minor neurological deficit).
The patient has assessed the possible outcome on both scales and, depending on the preliminary prognosis, the optimal treatment tactics were selected.
For clarity, let's give an example from a medical history:
Clinical example: Patient D., 53 years old, became acutely ill when, against the background of a rise in blood pressure at work, there were movement disorders in the right limbs and speech. Suffering from hypertension for 3-4 years. He was admitted to the Department of Neurology of the AF RSCEMP on February 20, 2018. On admission, he was in a state of moderate severity. Normal physique. Free breathing, 18 per minute. The heart rate is 80 per minute. BP 170/90 mm. Hg. Consciousness is depressed up to 11 points on the GCS. Lies with open eyes, inhibited, trying to follow instructions. Motor aphasia. Right-sided hemiparesis up to 2 points. Unilateral pathological reflexes of Babinsky and Oppenheim. No dislocation symptoms were found. MSCT of the brain revealed a mixed stroke-hematoma of the left cerebral hemisphere with a volume of 51 cm3, compression of the left lateral ventricle, displacement of the median structures to the right by 5.5 mm.
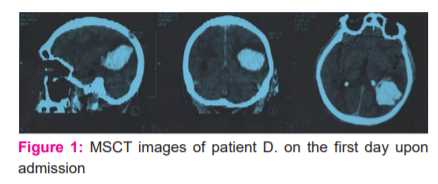
When predicting on the proposed scales, the patient scored a conditional 9 points for surgical treatment and 10 points for conservative treatment, and, accordingly, the patient was recommended to open transcortical removal of a stroke hematoma.
Within 4 hours, the patient underwent emergency surgery - resection craniotomy in the left parieto-occipital region, encephalotomy 0.5-1 cm long and removal of blood clots. During the operation, severe tissue bleeding was noted. After the operation, the patient's condition remained serious. Control MSCT of the brain, performed on the 3rd day after the operation, revealed a zone of oedema and hemorrhagic saturation of the brain in the area of ??the former hematoma with a volume of 49 cm3, displacement of the median structures to the right by 2 mm, minor haemorrhage into the lateral ventricles.
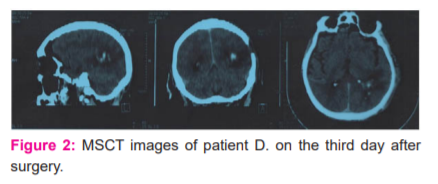
.The patient was discharged on the 12th day under the supervision of a neurologist and a cardiologist. Regression of neurological deficit was observed (right-sided hemiparesis up to 3 points), the surgical wound healed initially, the sutures were removed. At discharge, the GOSE score is 5 points. When assessing the general condition after 3 and 6 months, the patient's condition was assessed as good (6 and 7 points, respectively), which corresponded to our forecasts.
Results and discussion
To assess the results of treatment, we used the Glasgow Outcome Scale Extended (GOSE), modified by J.T. Wilson in 2000, the Glasgow Outcome Scale, which allows the quality of life of patients at various periods of follow-up, therefore, to assess the quality and adequacy of the treatment. Besides, the degree of impairment of consciousness was monitored on the Glasgow Coma Scale.
Thus, we observed a direct relationship between hospital mortality and recovery from age. In the young age group, the mortality rate in the hospital was 27.8%, in the middle - 28.8%, the elderly - 30.6%, and in the senile - 41.7%. Also, when assessing the results of treatment according to RSHIG, it was revealed that an excellent result was observed most of all in young patients (38.9%), less in middle-aged and elderly patients (28.1% and 22.2%, respectively) and the lowest rates in this aspect were revealed in elderly patients - 5.6%.
CONCLUSION
An inverse relationship was observed when assessing unsatisfactory outcomes, and the most unfavourable factor in predicting the outcome of treatment in patients in the elderly age group was the level of consciousness below the sopor, i.e. all elderly patients with a score below 9 points on the GCS on admission had a fatal outcome (62.5% - the first 7 days, 25% - the first 28 days, 12.5% ??- within 3 months). Our proposed criteria for evaluating the outcome of treatment of non-traumatic intracerebral haemorrhage make it possible to adequately predict the possible outcome of the course of the disease and choose the optimal treatment tactics.
ACKNOWLEDGEMENT
The authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors/editors/publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
Conflict of interest: None
Source of Funding: None
References:
-
Kuzibaev JM, Eshbobaev FY. The role of standard scales in the diagnosis and treatment of hemorrhagic strokes. Bull Emerg Med Tashkent 2009;1:35-39.
-
Hemphill JC, Farrant M, Neill TA. Prospective validation of the ICH Score for 12-month functional outcome. Neurology 2009;73:1088-1094.
-
Guzanova EV, Semenova TN, Trubilova MS, Kalinina SY. Survival of patients with non-operated non-traumatic intracerebral haemorrhage: prognostically significant factors. Med Almanac 2017;5(50):19-22.
-
Lee SH, Park KJ, Kang SH, Jung YG, Park JY, Park DH. Prognostic factors of clinical outcomes in patients with spontaneous thalamic haemorrhage. Medical science monitor. Int Med J Exper Clin Res 2015;21:2638-2646
-
Skvortsova VI, Krylov VV. Hemorrhagic stroke: a practical guide. GEOTAR-Media. 2005: 82.
-
Yakubov ZB, Sadykov BS. Predicting the results of treatment of intracerebral haemorrhages of non-traumatic aetiology. J Theor Clin Med Tashkent 2004;5:38-39.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License