IJCRR - 13(9), May, 2021
Pages: 75-81
Date of Publication: 07-May-2021
Print Article
Download XML Download PDF
Proximal Femoral Nail Versus Dynamic Hip Screw in Unstable Peritrochanteric Fractures of Femur,
A Comparative Clinical Study
Author: Nagesh Cherukuri, Raja Ramesh Badavath, Srikanth E
Category: Healthcare
Abstract:Introduction: Trochanteric fractures constitute one of the commonest fractures encountered in the elderly. Operative management which allows early rehabilitation and offers the patient the best chances for functional recovery is the treatment of choice for virtually all trochanteric fractures.
Objective: To compare the clinical, functional and radiological outcome of unstable intertrochanteric fractures femur treated randomly with proximal femur nail(PFN) and Dynamic hip screw(DHS). Functional and clinical outcome measurement using harris hip score.
Methods: This prospective randomized study compared the outcome of elderly patients with pertrochanteric fracture and carried out in Nizam`s institute of medical sciences Hyderabad in the year 2018 and 2019. 60 patients with unstable intertrochanteric fractures were included. 30 patients were operated on by the Proximal Femoral Nail (PFN) and 30 patients were operated on by Dynamic hip screw (DHS). Functional outcome was assessed by Modified Harris Hip Score.
Results: The rate of union was similar in both groups. The mean Harris hip Score in the DHS group was 82.1 compared to 83.5 in PFN. Effective results were seen in 63.3% of cases in the DHS group and 73.3% cases in the PFN group. The mean surgery time for DHS (76 min) was marginally higher than that for PFN (76 min) which is non-significant (P=0.281). The blood loss was also marginally lower in the IM Nail group (264ml) compared to the DHS group (354 ml) which was also not statistically significant (P=0.14).
Conclusion: The implant-related complications were much lesser in the patients treated with Dynamic Hip Screw(DHS). We did not encounter any secondary femoral fracture in patients managed by proximal femoral nails though this is one of the common complications reported in other studies.
Keywords: Dynamic Hip Screw(DHS), Proximal Femoral Nail, Peritrochanteric Fractures, femoral fracture, Functional outcome, Modified Harris Hip Score
Full Text:
INTRODUCTION
Intertrochanteric fractures are one of the commonest fractures especially in the elderly with osteoporotic bones and are usually due to low energy trauma like simple fall. It occurs most commonly in the age group above 70 years. Hip fractures have a bimodal age distribution. Approximately 97% occur in patients over 50 years of age (the incidence increases with age), and only 3% in patients under the age of 50. In the latter group, they occur most commonly between 20 and 40 years of age, usually in men, and are due to high-energy trauma associated with sports and industrial and motor vehicle accidents. In this young group, most hip fractures are subtrochanteric or basic cervical.
Intertrochanteric hip fractures account for nearly half of the hip fractures in the elderly; out of this more than 50 per cent of fractures are unstable. The unstable pattern occurs more frequently with increased age and with low bone mineral density. By 2025, the incidence of hip fracture is estimated to be doubled worldwide. Fractures in the elderly are serious injuries, often occurring in the terminal years of life and they have a major impact on society, our health care system and the cost of care. Fractures in the young age group lead to long-lasting elimination from working process or even loss of job thus causing socio-economic problems.1
The overall increase in the incidence of trochanteric fracture can be attributed to two factors: increased life expectancy which increases the aged population and high energy trauma which victimizes more young adults. Fractures of the hip in patients between 40 and 50 years of age usually occur in alcoholics or patients with multiple medical diseases, whose fractures are related to osteoporosis. The goal of treatment of an intertrochanteric fracture is to restore mobility safely and efficiently while minimizing the risk of medical complications and technical failure and to restore the patient to preoperative status.1 Moreover as this fracture occurs in elderly patients the risks from prolonged immobility and recumbency arise. Thus, treatment should be designed in a way that promotes union without deformity and enables early mobilisation at the same time. Since then a variety of different implants has been used either extramedullary or intramedullary.
The most commonly used implant is a sliding hip screw with a side plate (DHS), it is currently considered the gold standard for fixation of extracapsular hip fractures. DHS has been shown to produce good results, however, complications are frequent particularly in unstable fractures.2 Nailing has the advantage of providing rotational as well as axial stability in cases of trochanteric fractures allowing a faster postoperative restoration of walking ability when compared with DHS. The nails are load-sharing implants, whereas extramedullary devices are load-bearing. Proximal femoral nailing creates a shorter lever arm, which translates to a lower bending moment and a decreased rate of mechanical failure.
Potential disadvantages are related to a greater risk of jamming the sliding mechanism and stress risers at the site of the tip of the nail and distal locking bolts.3 Intramedullary implants have been associated with an increased risk of intraoperative and postoperative femur fractures compared with sliding hip screws. The increased peri-implant fracture incidence has been linked to stress concentration at the tip of the nail, stress concentration at the distal locking bolt, and reaming of the proximal femur to accommodate the wider proximal diameter of the nail necessary to allow a large diameter lag screw to pass through the nail.
Data published so far confirm that PFN is a reliable implant, producing results similar to those obtained with the DHS for unstable trochanteric fractures. However, some authors have reported a screw cut-out of the femoral head and a higher incidence of PFN intra-operational difficulties. For unstable trochanteric fractures and reverse oblique fractures, therefore controversy continues regarding the optimum choice of implant. The purpose of the present study is to compare outcome and complications between the PFN and DHS in the treatment of patients with an unstable pertrochanteric fracture.
MATERIALS AND METHODS
The present thesis work involves a prospective randomized study of 60 patients with unstable intertrochanteric fractures treated surgically in the Department of orthopaedics, Nizam`s institute of medical sciences, Hyderabad. Institutional ethical clearance was obtained (EC/NIMS/2237/2018).
Inclusion criteria: Patients with unstable intertrochanteric fractures femur which include
Inclusion criteria: Age 20 to 90 years, posterior medial large separate fragment (unstable), Failure to reduce fracture before internal fixation, Reverse oblique pattern and Fractures with subtrochanteric extension
Exclusion criteria: Stable fractures i.e fractures with intact posterior medial cortex, Pathological fractures, Patients with significant hip or knee arthritis and Compound fractures
Patients with unstable intertrochanteric fractures are taken into the study, a note of age, sex, occupation and mechanism of injury is made. The patient’s ambulatory status before the injury is considered. Clinical features do not contribute much to the assessment of type and comminution of fracture. Patients underlying past or present medical conditions are noted which have a bearing on the management and outcome. Measures taken in the acute stage for hemodynamic stabilization of the patient due to the fracture or due to other reasons are not taken in to account. Immediate immobilization of the injured limb with Buck`s skin traction is done to prevent further soft tissue damage and give comfort to the patient.
After the limb is immobilized radiographs are taken to confirm the diagnosis, delineate the fracture pattern, its obliquity and quality of bone present. All the fractures are classified according to Evan`s, Boyd & Griffin classification, AO classification system based on roentgenograms. All routine investigations are done for anaesthetic fitness. If operative treatment is undertaken, the following fractures determine the strength of fracture – Implant assembly, namely the 1) bone quality 2) fragment geometry 3) reduction. 4) implant design and 5) implant placement will be stressed upon. Once anaesthetic fitness is obtained routine preoperative preparation is carried out. Each patient is given antibiotic prophylaxis of injection cefotaxime 1gm just before surgery. The anaesthesia employed is left to the anaesthetist`s choice.
RESULTS
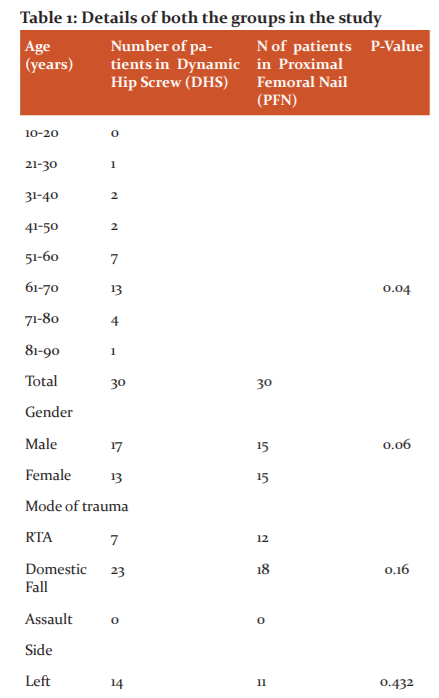
In our study, the maximum number of cases were in the age group of 50-70 years.
Males are more in number compared to females in our present study. Most of our patients were 50 years and above and in the domestic fall (fall at home) and trivial trauma was the main reason behind fracture while in young patients road traffic accident (RTA) was the main cause.c58% of the patients in our study were right-sided. Average time-lapse for surgery: 7 days in our study
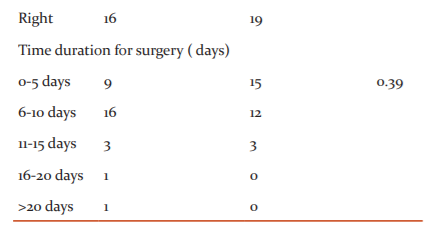
43.3% of patients in the DHS group belongs to the 31A2 type. Similarly, 38.3% of PFN patients belong to the 31A2 type.
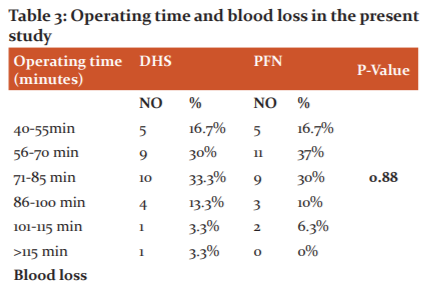
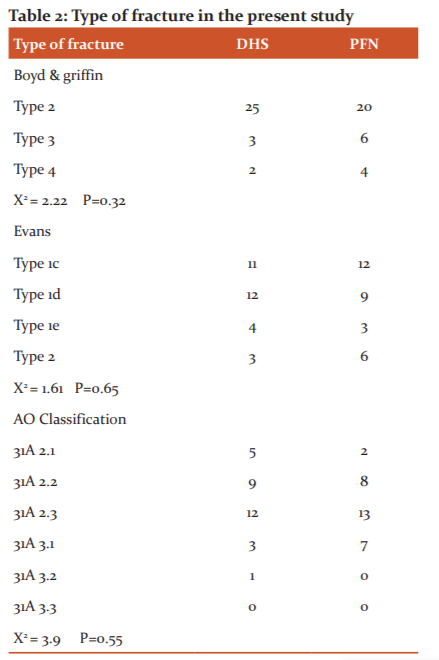
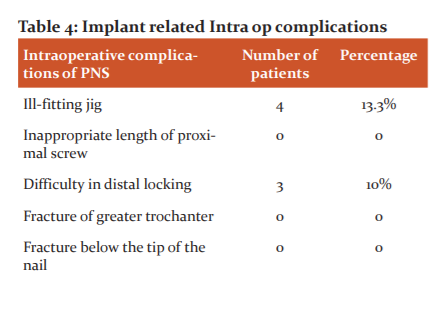
The mean duration of operation (in minutes) in our study was 72min in the PFN group and 76 min in the DHS group. Mean blood loss in the DHS group was 354 ml and mean blood loss in the PFN group was 264 ml
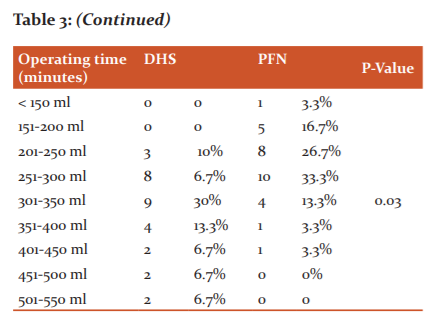
Mean duration of radiation exposure in sec was 61.5 in the PFN group and 58.3 in the DHS group.
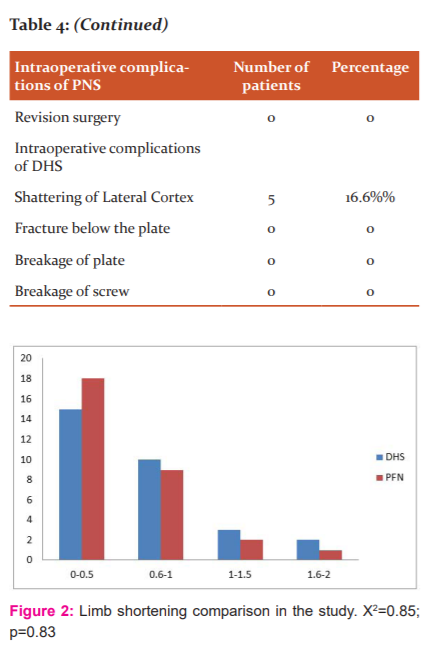
The average shortening in the P.F.N group was 8.4 mm as compared to 9.4 mm in the D.H.S group.
Mean Harris hip Score in the DHS group was 82.1 compared to 83.5 in PFN.
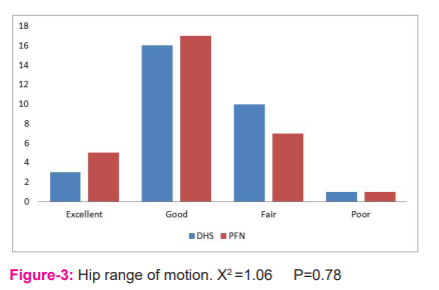
Excellent and good results were seen in 63.3% of cases in the DHS group and 73.3% cases in the PFN group.
DISCUSSION
The present study was carried out in Nizam`s institute of medical sciences Hyderabad in the year 2018 and 2019. 60 patients with unstable intertrochanteric fractures were included. 30 patients were operated on by the Proximal femoral nail(PFN) and 30 patients were operated on by the Dynamic hip screw (DHS).
In our study, the maximum number of cases were in the age group of 50-70 years. The average age was 59.2 years, the average age for males was 56.8years and for females was 62 years. The mean age in years for the group operated by PFN was 57.6 years. The mean age in years for the group operated by DHS was 60.9 years. The youngest patient was 21 years old and the oldest patient was 84 years old. In a study done by Adeel K et al mean age of patients in PNF was 59.32±2.39 years and in DHS was 60.88±12.49 years.4 Dorotka et al. reported in their series of 182 patients, the mean age of 77.1 years.5 Moran et al in a mega study of 2903 cases, reported the mean age of 80 years for hip fractures.6 In the present study, the mean age was found to be 71.1 years. The lower peak age as compared to the West may simply be linked to a shorter life span, as also to the inclusion of traumatic/ non-fragility fractures in the analysis.
Most of the patients from the present study were males. There was a slight male preponderance in our patients. The ratio of males to female was 1.1:1. In western countries, women suffering from osteoporosis far outnumber men, and this is largely thought to be due to the effects of menopause.7 The men: women ratio may be distorted in India because men are more likely to be brought for hospital care. Moran et al. reported 76% females with male to female ratio of 1:3.1.6 While Gardner et al. reported 78% females with male to female ratio of 1:3.5 in his series of 80 patients But in our study male to female ratio was 1.5:1.8 This sex distribution is against most of the international data but is following different local studies. The majority of the patients in the series were male as they are more outgoing and engaged in activities like agriculture, driving motor vehicles and are more likely to be involved or prone to accidents/fall. Females play a more dormant role and are involved more in household activities.9
Most of our patients were 50 years and above and in the domestic fall (fall at home) and trivial trauma was the main reason behind fracture while in young patients road traffic accident (RTA) was the main cause. 90% of hip fractures in the elderly result from a simple fall.10 In the cases treated by PFN, there were 18 cases(60%) due to domestic fall and 12 cases(40%) due to road traffic accident(RTA) while there were no cases due to assault. In the patients treated with DHS, there were 23 cases(76.6) where the mode of injury was due to domestic fall, while 7 cases(23.3%)were due to Road traffic accident (RTA). There were nil assault cases. Young patients with intertrochanteric fractures sustained trauma either as a result of a road traffic accident or fall from height, thereby reflecting the requirement of high-velocity trauma to cause a fracture in the young. Whereas in elderly people trivial trauma caused the hip fracture.
We have studied 60 cases of different types of intertrochanteric fractures in our present study. Among the 30 cases operated by PFN, 11(36.6%) patients were found to have proximal femoral fractures on the left side while 19 (63.3%) patients were having fracture on the right side. Among the 30 cases operated by DHS,14 (46.6%) patients were found to have proximal femoral fractures on the left side while 16 (54.4%) patients were having fracture on the right side.
The majority of patients in the present study series were operated on within 10 days following admission to the hospital (52/60). But in some patients (8/60) operative procedure was delayed due to medical problems (Hypertension and Diabetes) of patients. Average time-lapse for surgery: 7 days. Amongst patients who had a delay in operative intervention, 6 patients came to the hospital following 10 days of trauma. The delay in surgery was attributed to two major reasons. The first was the time lag between injury and hospitalization. The second reason for the delay was the time lag between hospitalization and surgery. This was attributed to the poor general condition of the patient towards requiring further workup for fitness for anaesthesia and surgery and associated injuries.
The most commonly used classification currently is the AO/OTA classification, which classifies IT fractures into three types: 31A1, 31 A2 and 31A3 with increasing instability as the grade increases. In A1 and A2 fractures, axial loading leads to fracture impaction, whereas in A3 fractures such impaction does not occur, and medial displacement of the distal fragment of the fracture is common due to the instability. All the fractures in our study were unstable intertrochanteric fractures and were classified according to the AO classification for peritrochanteric fractures. 49 (81.6%) patients were AO type 2 in both DHS and PFN group while 11(18.3%)patients were AO type 3 in both DHS and PFN group
In patients with domestic fall, distal radius fracture was seen in 2 patients which were treated conservatively, 1 patient had iliac wing fracture treated conservatively. 1 patient had an L2 wedge compression fracture which was treated conservatively. Associated injuries seen in patients with fall from height are distal end radius fracture in 1 patient treated conservatively.
In patients who sustained high energy trauma is as the head injury was seen in 2 patients, CT brain study was normal in one and the other had cerebral oedema and was treated conservatively. Blunt injury abdomen was seen in 1 patient CT scan showed Grade 1 liver laceration and was treated conservatively. 1 patient had radius fracture and patella fracture, 1 patient had a shaft femur fracture and patella fracture,1 patient had both bones leg fracture. Associated injuries were more common in the high-velocity trauma group. In our study 23 patients had hypertension, 10 patients were diabetic,7 patients had CAD, 1 patient with post CABG status, 4 patients had hemiparesis, 1 patient undergone PTCA, 2 patient had bronchial asthma,3 patients had COPD and 2 patients had CKD.
The majority of the patients were diabetic and hypertensive in our group.
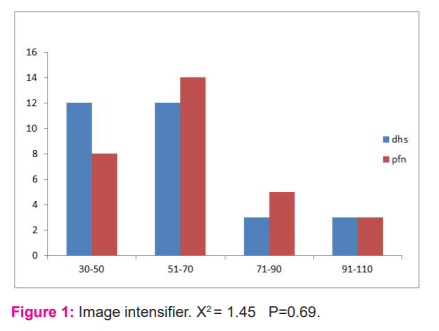
In our study, we considered various intraoperative parameters like radiographic exposures, duration of surgery and amount of blood loss. Radiographic exposure was more for PFN where the closed reduction was done and for comminuted fractures with difficult reduction. Duration of surgery was more for DHS compared to PFN. Blood loss was measured by mop count and collection in suction. Blood loss was more for DHS compared to the PFN group. Operating time and blood loss in various other studies are as follows.11
Mean blood loss of our study was comparable with that of Pan et al.12 Mean duration of surgery was comparable with that of Saudan et al. Mean operating time was more when compared to Giraud et al because most of the fractures were unstable pattern which required more radiation exposure for closed reduction.13 Superficial wound infection was seen in 4 cases in total. 3 cases were seen in those operated by DHS. The 3 cases operated by DHS had superficial wound infection at the suture site. This may be attributed to the long duration of surgery because of difficulty reduction& more soft tissue exposure, which is more in cases operated by DHS. In all the cases infection was treated by removal of skin sutures and antibiotics were continued. The wound healed by secondary intention. One case operated by PFN had a superficial infection which was treated with removal of skin sutures, antibiotics and regular dressing. In all the cases the wound healed in the end. In the series of patients operated by DHS by Dr. G.S Kulkarni, there were two cases of deep infections which were treated by removal of the implant.14 The infected sinuses thus healed after implant removal.
Two cases of fascia lata pain were noted due to the laterally protruding plate in the DHS group. No incidence of anterior thigh pain was noted in our study. In 4 cases (13.3%) operated cases by Proximal Femoral Nailing (PFN), there was ill-fitting of the jig. Due to the corresponding holes of the jig and nail was not matching at times. In 3 cases treated by PFN, we encountered difficulty in distal locking of the nail due to mismatch of corresponding holes of jig and nail. While in those cases operated by Dynamic Hip Screw (DHS) we encountered 2 cases (6.6%)having difficulty in reduction. This was due to excessive comminution and displacement. There is no incidence of crewcut out or breakage of the implant or femoral shaft fracture noted in the follow-up period in our study.
Varus angulation was noted in one operated case in the DHS group due to the pull of the muscle the distal shaft fragment tends to migrate upwards thus resulting in varus deformity. The other reason that patients had coxa vara deformity was due to inadequate reduction and failure to maintain neck-shaft angle preoperatively, however, varus angulation was less than 10 ? and there was no incidence of screw cut out. In the series by K.D Harrington, out of 72 cases, there were 4 cases of coxa vara and 56 cases of limb shortening at an average of 1.5 cms. The average shortening in the PFN group was 8.4 mm as compared to 9.4 mm in the D.H.S group. So, shortening is less in the PFN group which is not statistically significant, p-value 0.21.
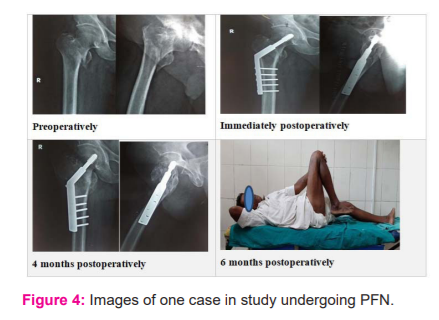
In the present study, in the cases that we operated by PFN, we have not encountered the ‘Z’ effect or reverse ‘Z’ effect. In patients with unstable intertrochanteric fractures treated with proximal femoral nailing, technical or mechanical complications seem to be related to the fracture type, operating technique, and time to weight-bearing rather than the implant itself.
The range of movement calculated by the Harris Hip Scoring system treated by both the implants i.e PFN and DHS was good, Mean Harris hip Score in the DHS group was 82.1 compared to 83.5 in PFN. Excellent and good results were seen in 63.3% of cases in the DHS group and 73.3% cases in the PFN group, however, results were not statistically significant(P value>0.05). Mean union time for fracture union in PFN group was 13.7 weeks while in DHS group was 14.8 weeks however results were not statistically significant (p-value >0.05) (Range:12 to 18 weeks). We have used criteria for the union as the presence of bridging callus at the fracture site. Most of the fracture circumference with a density similar to adjacent cortical bone. Clinically, absence of pain at the fracture site. Kevin D. Harrington11 in his series reported the average radiological time of fracture union as 16 weeks.
A randomized post-op rehabilitation study by Pajarinen et al. comparing peritrochanteric femoral fracture treated with DHS or PFN suggested that the use of PFN may allow faster postoperative restoration of walking ability when compared to DHS.16 Preservation of ambulatory function is the most important issue in the treatment of hip fractures. Larsson et al also showed that severe loss in ambulatory function would increase the risk of having socioeconomic problems.17 The level of ambulation achieved in the post-op period is a function of the pre-operative mobility status and medical condition, associated skeletal injuries, the quality of fracture stabilization, perioperative complications and early ambulation.
CONCLUSION
Both the implants PFN and DHS are excellent modalities in the management of pertrochanteric fractures of the femur. Functional outcome was assessed by Modified Harris Hip Score. Mean Harris hip Score in the DHS group was 82.1 compared to 83.5 in PFN. Results were excellent and good in 63.3% of cases in the DHS group and 73.3% cases in the PFN group, however, results were not statistically significant. The incidence of wound infection was found to be lower with intramedullary implants. 10% in DHS vs 3% in PFN. Non-union of trochanteric fracture is a rare entity, no case was found in our series of patients. The implant-related complications were much lesser in the patients treated with Dynamic Hip Screw(DHS). We did not encounter any secondary femoral fracture in patients managed by proximal femoral nails though this is one of the common complications reported in other studies. Since the sample size of this study was small the outcome cannot be generalised. However, a longer follow-up period and further study with a larger number of patients is required to confirm the results of our study
ACKNOWLEDGEMENT: The authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors/editors/publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
Conflict of interest-Nil
Financial support-Nil
References:
-
Babhulkar SS. Management of trochanteric fractures. Indian J Orthop 2006;40(4):210-218.
-
Gupta SKV, Valisetti VS. Comparative study between dynamic hip screw vs proximal femoral nailing in inter-trochanteric fractures of the femur in adults, Int J Orthop Sci 2015;1(1):07-11.
-
Maniscalco P, Rivera F, D’Ascola J, Del Vecchio EO: Failure of intertrochanteric nailing due to distal nail jamming. J Orthop Traumatol 2013:14:71–7.
-
Adeel K, Nadeem RD, Akhtar M, Sah RK, Mahy-Ud-Din I. Comparison of the proximal femoral nail (PFN) and dynamic hip screw (DHS) for the treatment of AO type A2 and A3 pertrochanteric fractures of the femur. J Pak Med Assoc 2020;70(5):815-819.
-
Dorotaka R, Schoechtner H, Buchingerw. The influence of immediate surgical treatment to proximal femoral fractures on mortality and quality of life within six hours of the fracture versus late than six hours. J Bone Joint Surg 2003;85:1107-13
-
Moran CG, Wennrt, Sikand M. Early mortality after hip fracture: Is delay before surgery important. J Bone Joint Surg 2005;87:483-9.
-
McCarus DC. Fracture prevention in postmenopausal osteoporosis: A review of treatment options. Obstet Gynecol Surv 2006; 61:39-50.
-
Gardner MJ, Brophy RH, Demetrakopoulos D. Interventions to improve osteoporosis treatment following hip fracture: A prospective, randomized trial. J Bone Joint Surg 2005;87:1-7.
-
Sengodan VC, Elangovan S, Kumar JS. Management of ipsilateral fracture of hip and shaft of the femur. Int J Curr Res Rev 2017; 07(17):7-14.
-
Koval KJ, Chen AL, Aharonoff GB, Egol KA, Zuckerman JD. Clinical pathway for hip fractures in the elderly: the Hospital for Joint Diseases experience. Clin Orthop Relat Res 2004;4(25):72-81.
-
Windoff J, Hollander DA, Hakimi M, Linhart: Pitfalls & complications in the use of proximal femoral nail. Lagenbecks Arch Aurg 2005:3901(1):234.
-
Pan X, Xiao D, Lin B, Huang G. Dynamic hip screws (DHS) and proximal femoral nails (PFN) in treatment of intertrochanteric fractures of the femur in elderly patients. Chin J Orthop Trauma 2004:6(7):785–789.
-
Saudan M, Lübbeke A, Sadowski C, Riand N, Stern R, Hoffmeyer W. Petrochanteric fractures: is there an advantage to an intramedullary nail? A randomized, prospective study of 206 patients comparing the dynamic hip screw and proximal femoral nail. J Orthop Trauma 2002:16(6):386–393.
-
Kulkarni GS, Miraj AW. Treatment of trochanteric fractures of hip by modified Richard's compression and collapsing screw. Indian J Orthop 1984:18(1):30.
-
Domingo LJ, Cecilia D, Herrera A, Resines C. Trochanteric fractures treated with a proximal femoral nail. Int Orthop 2001;25:298-301.
-
Pajarinen J, Lindahl J, Michelson O, Savolainen V, Hirvensalo E. Pertrochanteric femoral fractures treated with dynamic hip screws or a proximal femoral nail: A randomized study comparing post-operative rehabilitation. J Bone Joint Surg Br 2005;87(1):76–81.
-
Larsson S, Friberg S, Hansson LI. Trochanteric fracture; Influence of reduction and implant position on impaction and complication. Clin Orthop 1990;259:130-139.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License