IJCRR - 13(8), April, 2021
Pages: 152-156
Date of Publication: 25-Apr-2021
Print Article
Download XML Download PDF
Regenerative Endodontic Treatment in Bilateral Dens Evaginatus Teeth - Interesting Case Report
Author: Sivadas Ganapathy, Shilpa Hiremath, Vaishnavi Vedam, Abhishek Jeyaraj
Category: Healthcare
Abstract:Aim: The current report presents an interesting case scenario that describes the management of immature bilateral second premolar with Dens Evaginatus (DE) that developed pulp necrosis and symptomatic apical periodontitis. Case Report: An 10yrold healthy Chinese boy presented to the AIMST Paediatric clinic with the complaint of intermittent pain and fluid discharge from the buccal sulcus of a permanent mandibular left first premolar and permanent mandibular right first premolar for the past 1½ years. Upon intraoral examination and appropriate radiographic investigations, a diagnosis of pulp necrosis with symptomatic apical periodontitis was made for both teeth. The patient was explained regarding the aberrant tooth morphology and periapical condition. The treatment option of regenerative endodontic procedure was performed on the patient Discussion: DE is an anomaly presented as an outward projection of the tooth with a tubercle on the occlusal surface exhibiting outer enamel coverage, dentinal core and varying amounts of the pulp tissue. Complications usually increase in a developing young permanent tooth causing an interruption in the root formation root completion and closure, and sometimes periapical inflammation which can further delay a normal root development. Planning a preventive prophylactic restoration of such teeth to maintain the haemodynamic of the pulp and normal development of the root is a better option. This case was managed using Mineral Trioxide Aggregate (MTA) in regenerative endodontic treatment (RET) which resulted in continued root growth. Long term follow-up was recorded successfully. With past literature and the present case, it is safe to conclude that the revascularization of the tooth is progressing successfully for both teeth. Conclusion: Chronic apical periodontitis due to dens evaginatus requires special treatment strategies to eliminate the infection especially in young permanent teeth. Based on the results of the present case, it can conclude that Regenerative endodontic treatment is an ideal treatment method for Dens Evaginatus with an immature permanent tooth with apical periodontitis/ abscess.
Keywords: Dens evaginatus, Pediatricendodontics, Young permanent teeth, Endodontics, Case report
Full Text:
Introduction
Dens evaginate (DE) is an anomaly that is described as the outward projection of the tooth that appears as a tubercle on the occlusal surface with a dentinal core, outer enamel coverage and varying amounts of the pulp tissue. The synonyms for dens evaginatus includes odontoma of the axial core type, evaginatus odontoma, occlusal enamel pearl, occlusal tubercle, tuberculum anomalous, interstitial cusp, tuberculated cusp, Leong’s premolar, talon cusp. Different types of DE include smooth, grooved, terraced and ridged, as classified by Lau in 1955.1 This condition is predominantly found on the occlusal surface of mandibular premolars and lingual surface of anterior teeth (mainly maxillary lateral incisors).2 Prevalence of DE ranges from 1% to 4%3; with 2% prevalence among the Asian population4 and that higher rates were reported among the Chinese population (1.29%–3.6%). Dens Evaginatus occurs with a bilateral, symmetric distribution and a slight female predilection.5
The clinical significance of DE is the possible interference with occlusion. This traumatic occlusion may result in fracture of tubercle of micro exposure of the pulp resulting in pulpitis the sequel of which ranges from irreversible pulpitis to cellulitis and osteomyelitis in severe case.6
The current case describes the management of immature bilateral second premolar with DE that developed pulp necrosis and symptomatic apical periodontitis. This case was managed using regenerative endodontic treatment (RET) which resulted in continued root growth (maturogenesis).
Case presentation
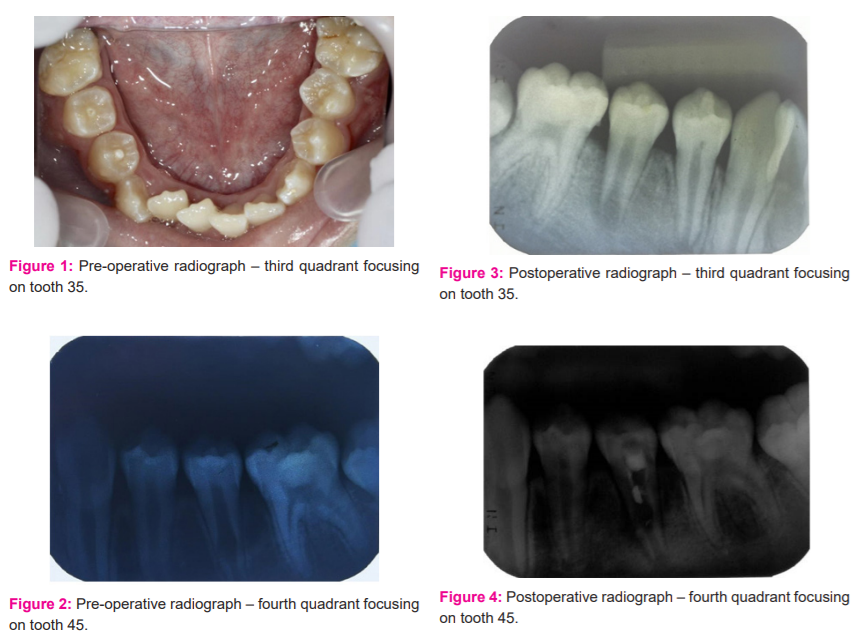
A 10 yr old healthy Chinese boy presented to the AIMST Paediatric clinic with the chief complaint of intermittent pain and fluid discharge from the buccal sulcus of a permanent mandibular left first premolar (tooth 35) and permanent mandibular right first premolar (tooth 45) for the past 1½ years. On intraoral clinical examination, the permanent mandibular left first premolar was caries-free with peculiar occlusal anatomy. There was a protruding mass in the mid?occlusal surface, identified as dens evaginatus. [Figure 1] On the buccal gingiva, a small 2 cm × 2 cm bluish, fluctuant swelling was noticed. On probing through the gingival margin, straw-coloured fluid discharge was noticed, denoting a cystic pathology with a probing depth of 6 mm. An intraoral periapical radiograph (IOPA) showed a periapical, 2 cm × 2 cm well?circumscribed radiolucency on the root apex on permanent mandibular left first premolar. An almost similar finding was seen clinically and radiographically on the permanent mandibular right first premolar tooth. permanent mandibular right first premolar had exhibited internal resorption. The apices of both permanent mandibular left first premolar and permanent mandibular right first premolar were open with widened periodontal ligament space. Pulp vitality test was found to be negative for both teeth. A diagnosis of pulp necrosis with symptomatic apical periodontitis was made for both permanent mandibular left first premolar and permanent mandibular right first premolar. [Figures 2 and 3] permanent mandibular left first premolar was found to have a midfoot radiolucency suggestive of internal resorption. The patient was explained regarding the aberrant tooth morphology and periapical condition. The treatment option of regenerative endodontic procedure was explained to the patient and consent was obtained before treatment.
In the first visit, local anaesthesia (Scandonest 2% L, Mepivacaine hydrochloride 2% with levonordefrin 1:20,000) was administered and the tooth was isolated using a rubber dam (Coltene). Access opening was completed on permanent mandibular right first premolar. Once access was gained, canals were irrigated gently and copiously with sodium hypochlorite (1.5%, 20mL/canal, 5 min). This was followed by irrigation with saline (20mL/canal, 5 min). Once the canals were dried with paper points low concentration of triple antibiotic paste (mixture of 1:1:1 ciprofloxacin: metronidazole: minocycline to a final concentration of 1-5 mg/ml) was placed into the canal using a syringe. The mixture was placed below the cement enamel junction to minimize crown staining. This was followed by a sealing pulp chamber with a dentin bonding agent. 3-4mm of a temporary restorative material (Cavit™) was used to seal the chamber. The patient was recalled after 3 weeks to assess the response to initial treatment. The absence of signs/symptoms of persistent infection indicated resolution of infection to the triple antibiotic mixture placed intracanal. In the second appointment after administering local anaesthesia (Scandonest 2% L, Mepivacaine hydrochloride 2% with levonordefrin 1:20,000) and the tooth was isolated. Canals were copiously irrigated with saline (20mL/canal, 5 min) to flush out the canal contents. After drying the canal with the paper point, bleeding was introduced into the canal system by over-instrumenting (induced by rotating a pre-curved K-file at 2 mm past the apical foramen). The bleeding was stopped at a level that allows for 3-4 mm of restorative material. Approximately at 3 mm distance MTA (Angelus) was placed over the canals and pulp chamber followed by the placement of wet cotton pellets on the top of the MTA after blood clot formation. A layer of glass ionomer (Fuji IX™, GC) flows gently over the capping material and light-cured for 40 s. the same protocol followed for permanent mandibular right first premolar was used for management of permanent mandibular left first premolar too. In the second appointment of management of permanent mandibular left first premolar the internal resorption lesion was found to increase radiographically suggestive of failure of treatment. So it was decided to remove the MTA and repeat the triple antibiotic dressing for 3 weeks. Later after inducing bleeding the MTA was placed so that it reached the internal resorption region. [Figures 4 and 5] This was done so that the material placed would help reduce the resorption and improve the root closure. The patient was recalled after 3, 6, 9, 12 months [Figures 6 and 7] and thereafter every six months for follow-up. The patient is being recalled regularly to see clinically and radiographically for continued root closure.
Discussion
Dens evaginate (DE) is an uncommon dental anomaly documented since 1925. It occurs primarily in Asians as a protrusion of a tubercle from occlusal surfaces of posterior teeth, and lingual surfaces of anterior teeth. Tubercles have an enamel layer covering a dentin core containing a thin extension of pulp. The potential serious complication of dens evaginatus is that it is highly prone to fracture of the extension resulting in pulp exposure. Complication increases in a developing young permanent tooth causing a crucial interruption in the root formation and subsequently roots completion and closure. Exposure of the pulp due to fracture or wear off of the DE can result in pulp necrosis and periapical inflammation, which can further delay a normal root development. Hence, it is an excellent idea to plan a preventive prophylactic restoration of such teeth to maintain the haemodynamics of the pulp and normal development of the root.
The aetiology of this condition remains unknown; however causative event leading to dens evaginatus malformation may be determined by multifactorial inheritance, i.e. combining both primary polygenetic with some environmental factors. Dens evaginatus originates during the morph differentiation stage of tooth development. The majority of cases reported indicate that dens evaginatus is an isolated anomaly rather than a primary part of any syndrome. But literature reveals that Dens evaginatus sometimes occurs together with a generalized syndrome. It is not reported as an integral part of any specific syndrome, although it appears to be more prevalent in patients with Rubinstein-Taybi Syndrome7, Mohr Syndrome (oral-facial-digital II Syndrome)8 Sturge-Weber Syndrome (encephalo-trigeminal angiomatosis)9, and in Ellis-van-Creveld Syndrome10
The presented case is not attached to any such syndrome and hence it is safe to assume that he had a multifactorial inheritance as a causative factor. The presented case is of a Malaysian Chinese descendant which has a 5.2% prevalence in dens evaginates cases. According to the Schulze classification, the presented case was Type V in which a tubercle arising from the occlusal surface obliterated the central groove. According to the classification given by Levitan and Himel, it was Type VI because of necrotic pulp and immature apex. For decades the conventional treatment for immature permanent teeth has been the traditional apexification techniques or the use of an artificial apical barrier method with mineral trioxide aggregate (MTA). However, studies have shown that in the long term these teeth are prone to root fracture as neither of these methods can increase the root thickness or the root length.
The presented case had intermittent pain and fluid discharge from the buccal sulcus of the mandibular right and left the first premolar. Therefore it was decided to open the access for tooth 34 on the first visit followed by pulp extirpation, debridement and disinfecting the canal with triple antibiotic paste. Triple antibiotic paste (TAP) containing metronidazole, ciprofloxacin and minocycline has been used widely as a root canal medicament due to its antimicrobial effects in endodontic regenerative procedures.11 Systemic antibiotic therapy depends on the patient’s compliance in taking a specific dosage regimen, the absorption of these drugs by the gastrointestinal system, the transportation via the blood circulatory system. Therefore, local application of antibiotics within the canal may be a more effective model for delivering the drug. TAP is effective in disinfecting necrotic infected pulps, thereby a suitable environment for vital tissue regenerative processes. In a retrospective study, Bose et al. suggested that regenerative endodontic treatment with TAP and calcium hydroxide has more significant effects in increasing the root length than either the non-surgical root canal treatments or MTA apexification. Also, dentin thickness increased with TAP application during the treatment as compared with the calcium hydroxide or formocresol.12
On the second visit (20 days later), the canal was revisited, inspected for necrotic tissues and cleaned with saline. The canal was dried thoroughly to induce bleeding. Lovelace et al. showed that the evoked-bleeding step in regenerative procedures after disinfection with TAP stimulates the increase of undifferentiated stem cells into the canal space from the periapical region. These cells help in the pulp regeneration process after effective disinfection. Therefore, TAP disinfected root canals had a significantly fewer chance of having a periapical lesion, and greater chances of gaining root length and wall thickness.
The formed blood clot provides a scaffold where various stem cells from apical regions, such as bone marrow mesenchymal stem cells, stem cells from apical papilla (SCAP), stem cells from periodontal ligament (SCPL), etc., can get implanted. Placement of Mineral Trioxide Aggregate over the induced clot is extremely crucial for the success of the RET as most often the blood clot could have limited growth factors and needs to be well protected from any external stimuli which might either dislodge the clot or contaminate it. There close monitoring is advised.13
In the presented case the patient was monitored clinically and radiographically monitored every 6 months for 18 months duration. For the permanent mandibular right first premolar, the same protocol was followed that was used for permanent mandibular left first premolar. The radiographic examination of the treated teeth permanent mandibular left first premolar and permanent mandibular right first premolar revealed continued root development and apical closure at 18 months after treatment. As the months progressed an increase in the root length of both permanent mandibular left first premolar and permanent mandibular right first premolar was observed radiographically. The apical third of the tooth started forming into a narrow apex initiating a root closure. Using MTA over the clot is indeed an important and crucial step for safely protecting the scaffold tissue from external factors. With this evidence, it is safe to conclude that the revascularization of the tooth is progressing successfully for both teeth.
Conclusion
Chronic apical periodontitis due to dens evaginatus requires special treatment strategies to eliminate the infection, especially in young permanent teeth. Every dentist must be aware of the existence of such dental anomaly and their treatment. Based on the results of the present case, it can conclude that Regenerative endodontic treatment is an ideal treatment method for Dens Evaginatus with an immature permanent tooth with apical periodontitis/ abscess. Besides, patients should also be made aware of the risks of the treatment and long term follow-ups. Observing the successful outcome of the present case, it is advised that early detection and careful treatment planning are needed to prevent further complication of the condition.
Acknowledgement: Nil
Conflicting Interest: Nil
Source(s) of support: Nil


References:
1. Levitan ME, Himel VT. Dens evaginatus: Literature review, pathophysiology, and comprehensive treatment regimen. J Endod 2006;32:1-9.
2. Echeverri EA, Wang MM, Chavaria C, and Taylor DL. Multiple dens evaginatus: diagnosis, management, and complications: case report. Pediatr Dent 1994;16(4):314-317.
3. Stecker S and DiAngelis AJ. Dens evaginatus. A diagnostic and treatment challenge. J Am Dental Assoc 2002;133(2):190-193.
4. Dankner E, Harari D, and Rotstein I. Dens evaginatus of anterior teeth. Literature review and radiographic survey of 15,000 teeth.Oral Surgery, Oral Med Oral Pathol Oral Radiol Endod 1996; 81(4):472-475.
5. Hill FJ and Bellis WJ. Dens evaginatus and its management. Br Dent J 1984;156(11):400–402.
6. Jerome CE, Hanlon Jr RJ. Dental anatomical anomalies in Asians and Pacific Islanders.Journal of the California Dental Association 2007;35(9):631–636.
7. Gardner DG, Girgis SS. Talon cusp: a dental anomaly in the Rubinstein-Taybi syndrome. Oral Surg Oral Med Oral Pathol 1979;47:519-521.
8. Goldstein E, Medina JL. Mohr syndrome or oral-facial-digital II: report of two cases. J Am Dent Assoc 1974;89:377-382.
9. Chen RJ, Chen HS. Talon cusp in the primary dentition. Oral Med Oral Surg Oral Pathol 1986;62:67-72.
10. Hattab FN, Yassin OM, Sassa IS. Oral manifestations of Ellis-van Creveld syndrome (Chondroectodermal Dysplasia): Report of two siblings with unusual dental anomalies. J Clin Pediatr Dent Winter 1998;22(2):159-163.
11. Zahed M, Jafarzadeh H, Shalavi S, Yaripour S, Sharifi F, Kinoshita JI. A Review on Triple Antibiotic Paste as a Suitable Material Used in Regenerative Endodontics. Iran Endod J 2018;13(1): 1–6.
12. Bose R, Nummikoski P, Hargreaves K. A retrospective evaluation of radiographic outcomes in immature teeth with necrotic root canal systems treated with regenerative endodontic procedures. J Endod 2009;35(10):1343–1349.
13. Lovelace TW, Henry MA, Hargreaves KM, Diogenes A. Evaluation of the delivery of mesenchymal stem cells into the root canal space of necrotic immature teeth after the clinical regenerative endodontic procedure. J Endod 2011;37(2):133–138.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License