IJCRR - 13(8), April, 2021
Pages: 149-151
Date of Publication: 25-Apr-2021
Print Article
Download XML Download PDF
Retinopathy Associated with Hyperviscocity Syndrome
Author: Sadafnaz Sabah, Abdul Waris, Syed Asghar Rizvi, Mohd Rameez Reza
Category: Healthcare
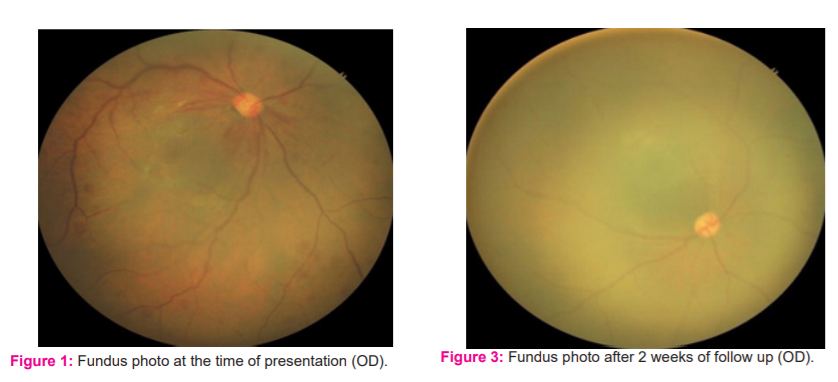
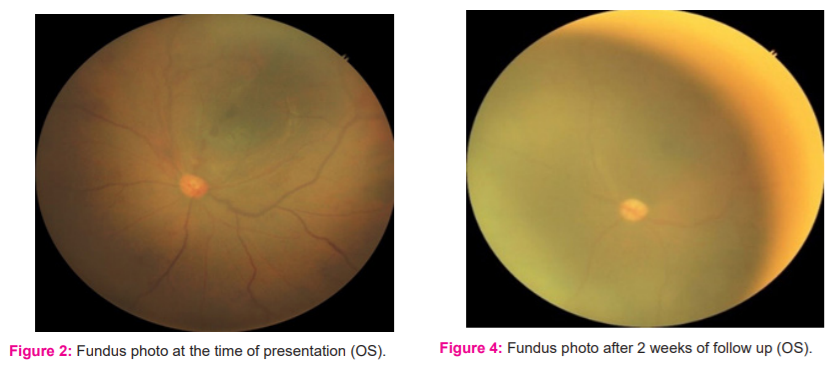
Abstract:Introduction: Hyperviscosity syndrome is clinically manifested by oronasal bleeding, retinal haemorrhages, and variable neuro-logical symptoms. The most reliable clinical manifestations of serum hyperviscosity are visual disturbances and oronasal bleed. Its early recognition is important as it constitutes important morbidity and may lead to blindness. Case presentation: Herein, we present a case of a newborn female on day 3 of life who presented with lethargy, poor feeding, tachypnoea and cyanosis. Dilated fundoscopy showed extensive mid-peripheral retinal haemorrhages with dilated and tortuous retinal veins. The patient was investigated and haematocrit, blood counts, and bilirubin level was found to be raised due to hyperviscosity of blood. The patient was managed with phototherapy haemodilution to decrease blood viscosity which resulted in the uneventful recovery of the patient with normal blood count, haematocrit and other lab values. On follow up after two weeks, ophthalmoscopy showed normal retinal vessels with few retinal haemorrhages. Discussion: We describe a unique case of retinopathy associated with hyperviscosity syndrome. The retinal changes as seen in our case were due to increased haematocrit and blood viscosity. As there are scarcely a few studies about retinopathy associated with hyperviscosity syndrome, this case illustrates the prompt and accurate diagnosis of hyperviscosity syndrome for the institution of appropriate therapy.
Keywords: Mucosal bleeding, Visual abnormalities, Serum hyperviscosity
Full Text:
INTRODUCTION
The classic triad of hyperviscosity includes mucosal bleeding, visual abnormalities, and neurological abnormalities. The most reliable clinical manifestations of serum hyperviscosity are visual disturbances and oronasal bleed. Whenever hyperviscosity is suspected, ophthalmoscopy should be performed. Retinal haemorrhages with dilation and tortuosity of retinal veins may be seen as seen in our case. Prompt diagnosis of hyperviscosity syndrome from the eye examination enables the institution of appropriate therapy. There are scarcely a few studies about retinopathy associated with hyperviscosity syndrome. Early recognition is important as it constitutes important morbidity and may lead to blindness.
CASE PRESENTATION
A newborn female weighing 3.0 kg at term to a 27-year young healthy primigravida developed lethargy with poor feeding, tachycardia, tachypnoea and cyanosis on day 3 of life. The baby was intubated and kept on ventilatory support. The cyanosis was improved after three days and the baby was extubated. The patient also developed hypocalcaemia, hypoglycaemia and two episodes of seizures which were managed conservatively. The essential ocular findings were retinal haemorrhages in the mid-peripheral retina with dilated and tortuous retinal veins in OD [Figure 1] and OS [Figure 2] which was evaluated with indirect ophthalmoscopy and scleral depression. Optic disc was found to be normal. Relevant investigations were done. The haemoglobin level was 24 gm/dl. The haematocrit was 68%. The white cell count was 17100 /cu mm (differential count: Neutrophils 72.1 %, lymphocytes 19.5%, monocytes 8.4 %) and platelet count was172000/cu mm. Bilirubin level was 5.7 mg/dl. Renal functions and liver function test was mildly deranged. The electrocardiogram was normal and an x-ray examination of the chest was also normal. Ultrasonography of the skull was found to be normal. The patient was managed with haemodilution of blood which showed remarkable symptomatic improvement and thus stabilisation of the patient. The patient was given phototherapy treatment following which there was considerable improvement in jaundice. On follow up after two weeks, the fundus examination showed normal blood vessels with no dilation and tortuosity. Also, the retinal haemorrhages were found to be decreased in OD [Figure 3] and OS [Figure 4]. On investigations, haematocrit, blood counts and bilirubin level were found to be normal which was previously increased. Thereafter baby showed an uneventful recovery with normal growth and development on further follow-up.
TREATMENT AND OUTCOMES
The patient was managed with haemodilution and was followed up after two weeks. After one week of treatment, there was a remarkable improvement in HVS-induced retinal changes promptly. Vision improved remarkably and retinal haemorrhages were resolved with normal retinal venous diameter. Haematocrit level reduced to 48% with normal haemoglobin, and bilirubin counts. The patient improved symptomatically. The patient came for follow up after two weeks with normal ocular findings. Also, the fundus showed no pathologies.
DISCUSSION
HVS was described by JanWaldenstrom in his original 1944 report of 2 patients with macroglobulinemia.1 Bleeding, usually skin and mucosal, is known to be the most common manifestation of HVS. However, blurred vision, headache, vertigo, dizziness, nystagmus, deafness, and ataxia also occur in HVS.2-4 Patients with severe hyperviscosity syndrome may present with confusion, dementia, stroke, or coma. However, heart failure and other cardiovascular signs are less common.2,5-9 All the symptoms associated with polycythaemia and hyperviscosity are common to many neonatal disorders. In a study, the symptoms suggestive of polycythaemia included lethargy in 15%, refusal of feeds in 13%, respiratory distress in 10%, hypoglycaemia in 10.8%.9 Incidence of hypoglycaemia may be as high as 40%.10 Patients with hyperviscosity syndrome have an increased blood volume because of an expanded plasma volume. This plasma volume expansion correlates with the rise in relative serum viscosity. Also, hyperviscosity syndrome is unlikely unless the serum viscosity is greater than 4.2,5,7-9 Viscosity levels in HVS vary significantly between patients. However, viscosity values correlate closely with signs and symptoms in the same patient (“symptomatic threshold”).2,4,5-9 We can diagnose HVS from the physical examination by the funduscopic finding of marked retinal venous engorgement resembling hot dogs on a string (i.e., “sausaging”).4,5-9,11 Haemorrhages, microaneurysms, exudates, papilledema, and an appearance indistinguishable from central retinal vein occlusion may be seen in later stages. Early diagnosis of hyperviscosity syndrome from the eye examination enables the institution of appropriate therapy (i.e. plasmapheresis).2,4,11-13 Urgent plasmapheresis using a cell separator should be carried out for patients experiencing visual symptoms to reduce the likelihood of blindness from retinal haemorrhages/retinal detachment.14 Plasmapheresis can also reverse HVS-induced retinal changes promptly, including reducing the retinal venous diameter and increased venous blood viscosity.15 The retinal examination findings correlate with the symptomatic threshold for HVS.In the case of neonates, an asymptomatic baby with polycythaemia can be managed by keeping the baby well hydrated with increased maintenance fluid requirements to prevent hyperviscosity. Any baby with polycythaemia who is symptomatic should have a partial exchange transfusion if the peripheral venous haematocrit is more than 65%. Asymptomatic infants with peripheral venous haematocrit between 60-70% can usually be managed by increasing fluid intake and repeating the haematocrit in 4-6 hours. Most neonatologists perform an exchange transfusion when the peripheral venous haematocrit is above 70% in the absence of symptoms, but this is controversial.16 In our case, haemodilution of blood resulted in stabilisation of the patient with remarkable improvement in hyperviscosity induced retinal changes. The long-term outcome in infants with asymptomatic hyperviscosity whether treated or untreated remains controversial.17
CONCLUSION
We describe a unique case of retinopathy associated with hyperviscosity syndrome. The retinal changes as seen in our case were due to increased haematocrit and blood viscosity. However, the haemodilution of blood resulted in remarkable improvement in hyperviscosity induced retinal changes. As we know, prompt diagnosis of hyperviscosity syndrome from the eye examination enables the institution of appropriate therapy so, early recognition is important as it constitutes important morbidity and may lead to blindness.
References:
1. Singh S, Narang A, Bhakoo ON. Polycythaemia in newborn. Indian Pediatr 1990;(27):349-52.
2. Mehta J, Singhal S. Hyperviscosity syndrome in plasma cell dyscrasias. Semin Thromb Hemost 2003;(29):467-471.
3. MacKenzie MR, Babcock J. Studies of the hyperviscosity syndrome: II. Macroglobulinemia. J Lab Clin Med 1975;85(2):227-234.
4. Stone MJ. Waldenstro¨m’s macroglobuli emia: hyperviscosity syndrome and cryoglobulinemia. Clin Lymphoma Myeloma 2009;9(1):97-99.
5. Fahey JL, Barth WF, Solomon A. Serum hyperviscosity syndrome. J Am Med Assoc. 1965;192(6):120-123.
6. Perry MC, Hoagland HC. The hyperviscosity syndrome. JAMA 1976;236(4):392-393.
7. Bloch KJ, Maki DG. Hyperviscosity syndromes associated with immunoglobulin abnormalities. Semin Hematol 1973;10(2):113-124.
8. MacKenzie MR, Lee TK. Blood viscosity in Waldenstro ¨m’s macroglobulinemia. Blood. 1977;49(4):507-510.
9. MacKenzie MR, Brown E, Fudenberg HH, et al. Waldenstro¨m’s macroglobulinemia: correlation between expanded plasma volume and increased serum viscosity. Blood. 1970;35(3):394-408.
10. Wiswell TE, Cornish JD, Northam RS. Neonatal polycythaemia: frequency of clinical manifestations and other associated findings. Pediatrics 1986;(78):26-30.
11. Stone MJ, Pascual V. Pathophysiology of Waldenstro ¨m’s macroglobulinemia. Haematologica 2010;(95):359-364.
12. Schwab PJ, Fahey JL. Treatment of Waldenstrom ¨m’s macroglobulinemia by plasmapheresis. N Engl J Med 1960;263(2):574-579.
13. Solomon A, Fahey JL. Plasmapheresis therapy in macroglobulinemia. Ann Intern Med 1963;58(5):789-800.
14. Thomas EL, Olk RJ, Markman M, et al. Irreversible visual loss in Waldenstro¨m’s macroglobulinaemia. Br J Ophthalmol 1983;67:102-106.
15. Menke MN, Feke GT, McMeel JW, et al. Ophthalmologic techniques to assess the severity of hyperviscosity syndrome and the effect of plasmapheresis in patients with Waldenstro¨m’s macroglobulinemia. Clin Lymphoma Myeloma 2009;9(1):100-103.
16. Goorin AM. Polycythaemia. In: John P Cloherty, Ann R Stark, editors, 4th ed. Manual of neonatal care. Lippincott Raven 1998;466-70.
17. Bada SH, Korones SB, Wilson WM. Asymptomatic syndrome of polycythemia hyperviscosity. Effects of plasma exchange transfusion. J Pediatr 1992;120:579-85.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License