IJCRR - 13(8), April, 2021
Pages: 05-09
Date of Publication: 25-Apr-2021
Print Article
Download XML Download PDF
The Pattern of Creatinine Clearance in Gestational and Chronic Hypertension Women from the Third Trimester to 12 Weeks Postpartum
Author: Mardhiah Kamaruddin, Siti-Azrin Ab Hamid, Fauziah Jummaat, Azreen Syazril Adnan, Bachok Norsa'adah
Category: Healthcare
Abstract:Introduction: Hypertension complication during the pregnancy will lead to morbidity and fatality in pregnancy. Objective: The study was done to identify the differences of calculated creatinine clearance level between two groups of pregnant patients which were gestational and chronic hypertension patients from pregnancy to the postpartum period. Methods: A prospective cohort study was done from September 2015 to April 2016 on the Obstetrics & Gynaecology Clinic of Hospital USM patients. A total of 10 pregnant mothers from gestational hypertension patients and 10 pregnant mothers from chronic hypertension patients who signed the consent form were included in the study. The patient's medical records were re-viewed. Patients with proteinuria > 300mmHg, preeclampsia or eclampsia, on Angiotensin-converting enzyme (ACE) inhibitors or angiotensin-receptor blockers (ARBs), and those who have present or history of diabetes, renal disease, liver disease, systemic lupus erythematosus, hepatitis, hyperaldosteronism, renal artery stenosis or thyrotoxicosis were excluded from the study. Blood for renal function test was collected at three phases. The collection was at the last trimester of pregnancy followed by six weeks and 12 weeks after labour. Repeated measure ANOVA was used to analyze the pattern of the calculated creatinine clearance between the groups from pregnancy to postpartum. Results: The pattern of calculated creatinine clearance is the difference between groups. In the gestational hypertension group, the calculated creatinine clearance was an increase from 6 weeks postpartum to 12 weeks. The pattern of calculated creatinine clearance still declined in the chronic hypertension group after 6 weeks postpartum. Conclusion: The women with previous hypertensive disorders during pregnancy should have a regular checkup especially on checking renal function test as it is one of the major causes of unintended of having renal disease.
Keywords: Creatinine clearance, Chronic hypertension, Gestational hypertension, Pregnancy, Postpartum
Full Text:
Introduction
Globally, hypertension existing in all pregnancies by up to 10%. This complication during the pregnancy will lead to morbidity and fatality in pregnancy.1 The disease has been growing among inpatients who delivered at the hospital.1 The occurrence of hypertensive disorders during pregnancy in the United States is 5 to 10% that shown the second-highest leading cause of mortality in maternal death.2 Based on the study in Kuala Lumpur, 7.14% maternal death was reported because of preeclampsia and 4.41% patients had gestational hypertension during pregnancy.3
Human renal function will change due to the hormonal changes in pregnancy. The increase of creatinine clearance during pregnancy because of the increase of ultrafiltration volume and reduced average colloid osmotic gravity.4 The size of the pregnant women will rise to 1 cm and the most notable modifications that can be found are in the urinary area.5 The renal hemodynamic will changed and it can be noticed during the completion of the first trimester when both creatinine clearance and renal plasma flow increase by 50%.5 The renal plasma flow decline starting from week 12 till week 38 while GFR will stabilize around 4 to 6 weeks after delivery.6 The discrepancy in GFR value happens when serum creatinine level decreases during pregnancy. In pregnancy, the average of serum creatinine falls to a pregnancy range of 0.4-0.8 mg/dl.7 It was found that the creatinine clearance was 40% higher compared with non-pregnant women.4 Then, the value of creatinine clearance returns to normal around a month after delivery.4
Prakash et al. (2006) reported 25% of chronic hypertension pregnant women had a normal renal function.8 Of all the reported patients with chronic hypertension, 9.72% had a higher serum creatinine concentration which is more than 3 mg/dl with a not serious renal failure. The majority had mild renal failure while four patients had a serious renal failure that depends on the haemodialysis. The risk causes that contribute to the exposure of getting renal problem among chronic hypertension patient was gout, the users of the diuretic agent, obesity and older age.9 The hazard ratio of getting chronic kidney disease (CKD) and end-stage renal failure (ESRD) in hypertensive disorders women was 9.3 compared to healthy women.10
Another study reported the effect of increased systolic blood pressure (SBP) towards the probabilities of a fast decrease of renal function.11,12 Hanratty et al. (2011) reported there was an association between high blood pressure and CKD.13 Increased level of SBP that more than 120 mmHg will increase the risk of developing CKD.13 The collaboration of a multidisciplinary team between obstetricians and nephrologists is crucial to monitor the blood pressure in women with renal injury so that it can keep the kidney from other worsening condition.14 The objective of the study was to determine the changes of calculated creatinine clearance from the third trimester to 12 weeks after delivery in gestational and chronic hypertension women.
Materials and Methods
Study Participants and Categories
A prospective cohort study was conducted on women who were diagnosed with gestational and chronic hypertension and had to follow up treatment at Obstetrics and Gynaecology (O&G) Clinics of Hospital Universiti Sains Malaysia (USM) during the antenatal and postpartum period from December 2015 to February 2016. The patients were excluded if had proteinuria > 300mmHg, preeclampsia or eclampsia, on Angiotensin-converting enzyme (ACE) inhibitors or angiotensin-receptor blockers (ARBs), and had a history of diabetes, renal disease, liver disease, systemic lupus erythematosus, hepatitis, hyperaldosteronism, renal artery stenosis or thyrotoxicosis. The study protocol was approved by a hospital university where the research was conducted. A written consent form was given to each patient before joining the research as an agreement towards the study protocol.
Hypertension was defined as SBP over 140 mm Hg and/or DBP over 90 mm Hg during pregnancy.8 chronic hypertension was defined as hypertension that diagnosed before the pregnancy or before the 20 weeks of pregnancy 18 and gestational hypertension was defined as hypertension that never diagnosed before the pregnancy and was diagnosed after 20 weeks of pregnancy.
Clinical data and sample collection and measurement
A study proforma was used to collect information from the medical record on maternal parameters and foetal parameters. Maternal parameters include age, weight, height, gestational age at delivery, body mass index (BMI), gravida and parity, type of hypertension, creatinine clearance and blood pressures. Foetal parameters include gender, birth weight, Apgar score, complication and method of delivery. Blood samples for the renal function test were collected at the third trimester, six weeks after delivery and 12 weeks after delivery. The Modification of Diet in Renal Disease (MDRD) formula was used to calculate the creatinine clearance level. The serum creatinine results from the renal function tests were obtained to generate the creatinine clearance. The blood taken was done by the nurse at O&G Clinic. The blood was submitted to the chemical pathology laboratory. The result of the blood tests was obtained from the electronic record.
Statistical analysis
Univariable analyses were performed to compare the baseline characteristics and foetal parameter between gestational and chronic hypertension patients. Mann Whitney was applied to determine the difference of means between groups for variables: age, gestational ages at delivery, birth weight, and BMI. The level of significance was set as 0.05. Repeated Measure ANOVA was used to see the differences of creatinine clearance from the last trimester of pregnancy to 2 months postpartum for both groups. Statistical Package for Social Sciences version 24.0 (IBM Corporation, 2013) was used to perform data entry and data analyses.
Results
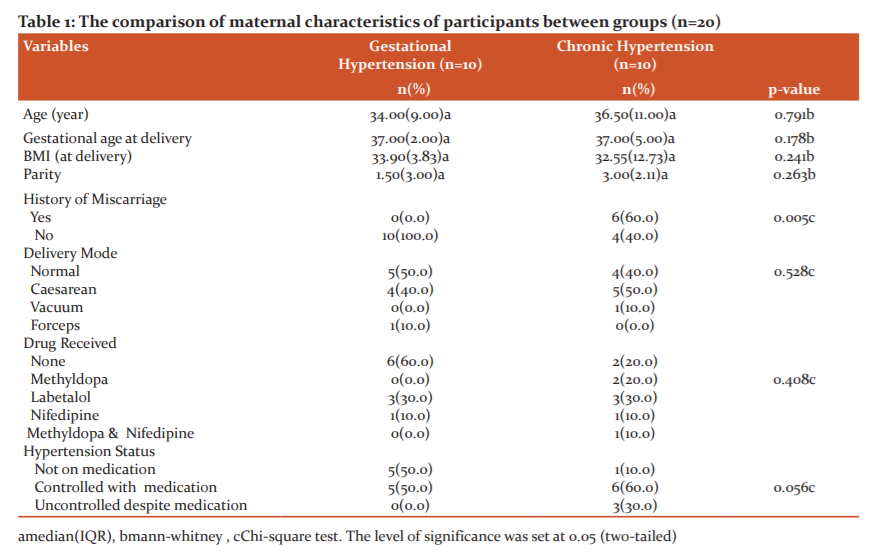
The maternal characteristics between chronic hypertension and gestational hypertension were not statistically significant except for the history of previous miscarriage (Table 1).
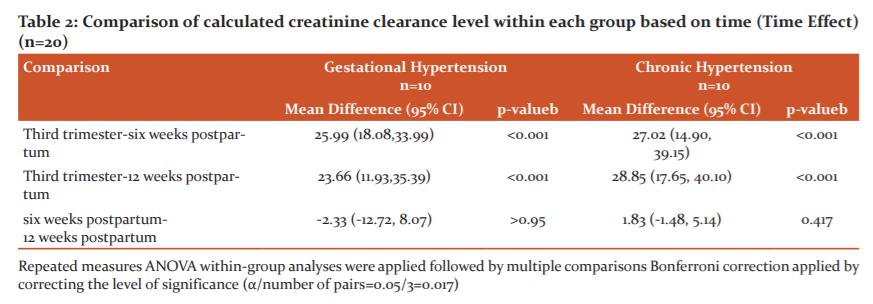
There was a declination of creatinine clearance in chronic hypertension participants from the last trimester of pregnancy to 2 months postpartum compared to gestational hypertension participants (Figure 1). The total mean difference from the third trimester to 12 weeks postpartum in chronic hypertension participants was 28.85 ml/min while for gestational hypertension participants were 23.66 ml/min. The calculated creatinine clearance still declined in chronic hypertension participants at 12 weeks postpartum by 1.83 ml/min, but it showed the increment of calculated creatinine clearance in gestational hypertension participants by 2.33 ml/min (Table 2).
Discussion
Maternal and foetal characteristics based on the type of hypertension
There was no significant difference in maternal parameters between groups except for a previous history of miscarriage. The findings were similar to a study conducted in Chicago where there was no difference in maternal characteristics between gestational hypertension and chronic hypertension.15 A cohort study of 33 856 singleton pregnancy reported that those with chronic hypertension had a higher risk of miscarriage by 2.89 odds compared to those without chronic hypertension.16
The previous study proposed that there was a relationship between small birth weight and the number of previous miscarriage(s).17 In the current study, the mean birth weight for chronic hypertension was 2.59 kg and 2.88 kg for gestational hypertension. The lower birth weight in chronic hypertension participants might reflect the significant history of miscarriage. Another study reported that women aged 35-39 years old increase the chance of getting miscarriage by 2.4 compared to women aged less than 35 years old.18 The current study showed that participants in chronic hypertension were older compared to gestational hypertension. So, age might be one of the factors that affect the previous miscarriage in chronic hypertension for the current study.
The trend of creatinine clearance level in the last trimester of pregnancy to postpartum
The level of calculated creatinine clearance declined from the third trimester to six weeks after delivery in gestational hypertension patients. The mean difference between these two measurements was 25.99 ml/min. But, there was only a slight increase of calculated creatinine clearance level from six weeks postpartum to 12 weeks postpartum with 2.33 ml/min. The mean level of calculated creatinine clearance in gestational hypertension participants declined from the third trimester to 12 weeks after delivery with 98.86 ml/min to 75.73 ml/min respectively.
There was a declination of calculated creatinine clearance from the third trimester to six weeks postpartum for both groups. It was recognised that the size of kidneys increases up to 30% during pregnancy because of vascular and interstitial spaces changes.6 Renal function changes starting before conception in reaction to hormonal deviations during the menstrual cycle.4 The increase of GFR can be noted at four and nine weeks gestation by 20% and 45% respectively.4 The physiologic adaptation that mostly can be seen in normal pregnancy is glomerular hyperfiltration. It will reduce the serum creatinine, so that increase the GFR level in pregnancy.6
Yelumalai et al. reported that the serum creatinine in normal pregnancy and six weeks postpartum was 50.5 µmol/L and 59.4 µmol/L respectively.19 GFR remains increase throughout pregnancy and then normalise at six to eight week of postpartum.6 Three studies reported the decline of creatinine clearance from pregnancy to postpartum and its restoration to normal level in the postpartum period.20 The study proposed that the level of creatinine clearance among gestational and chronic hypertension was rising throughout pregnancy.14,21
As for chronic hypertension women, the blood pressure declined until 12 weeks postpartum that one of the reasons associated with the decline of the calculated creatinine clearance. Many studies showed a direct relationship between renal function progression and blood pressure.22,23 It can be concluded that the severity of increase in levels of diastolic blood pressure was connected to the reduction in final creatinine clearance. Participants with chronic hypertension also received antihypertensive treatment during postpartum that may cause the reduction of calculated creatinine clearance after three months of delivery. It was also proven that the antihypertensive agent would increase the risk of increasing the serum creatinine by 1.26 odds compared to those who did not receive antihypertensive agent.24
The major limitations of this study was the small sample size due to the time constraint and obstacles. There was a limited number of the patient without underlying diseases who delivered from 1st December 2015 to 31st December 2016. In the beginning, the total number of patients available for the study setting for gestational hypertension and chronic hypertension was approximately 50 patients but due to the development of preeclampsia and superimposed preeclampsia after delivery, they were excluded from the study. There were also many hypertensive disorders at pregnancy who had diabetes and other diseases. From the study population, 20% developed preeclampsia or superimposed preeclampsia at delivery or postpartum and 40% had other diseases. There were no creatinine clearance results for patients after delivery so it was impossible to use another study design rather than a Prospective Cohort Study.
Conclusions
Chronic hypertension had more reduction of calculated creatinine clearance after postpartum compared to gestational hypertension participants. Blood pressure may affect the declination of creatinine clearance level in chronic hypertension participants. The women with previous hypertensive disorders during pregnancy should have a regular checkup especially on checking renal function test as it is one of the major causes of unintended of having a renal disease
Acknowledgement
The publication of the research was supported by Fundamental Research Grant Scheme (FRGS) under Malaysia’s Ministry of Higher Education (Grant number: R/FRGS/A0100/01605A/002/2018/00548).
Conflicts of interest: The study had no conflicts of interest.
FJ, AHSA, and ASA were responsible to look at, design the study and arrange for the research materials. MK conducted research, collected data, analysed and interpreted the data. All authors agreed on the final draft, provided logistics support, and involved in each part in finishing the manuscript.
Ethical approval
Approval was obtained from the Human Research Ethics Committee Universiti Sains Malaysia (reference number: USM/JEPem/15080277).
References:
1. Duley L. The global impact of pre-eclampsia and eclampsia. Semi Perin 2009;33(3):130-137.
2. Sibai B, G Dekker, M Kupferminc. Pre-eclampsia. Lancet 2005; 365(9461): 785-799.
3. Malhotra S, Yentis SM. Reports on Confidential Enquiries into Maternal Deaths: management strategies based on trends in maternal cardiac deaths over 30 years. Int J Obstet Anesth 2006 Jul;15(3):223-6.
4. Hussein W, Lafayette RA. Renal function in normal and disordered pregnancy. Curr Opin Nephrol Hypert 2014; 23(1):46.
5. Podymow TP. August. Hypertension in pregnancy. Adv Chron Kid Dis 2007;14(2):178-190.
6. Odutayo A, M Hladunewich. Obstetric nephrology: renal hemodynamic and metabolic physiology in normal pregnancy. Clin J Am Soc Nephrol 2012;7(12):2073-2080.
7. Fischer MJ. Chronic kidney disease and pregnancy: maternal and fetal outcomes. Adv Chron Kid Dis 2007; 14(2): 132-145.
8. Prakash J, Pandey LK, Singh AK, Kar B. Hypertension in Pregnancy : Hypertension Based Study. J Assoc Physic India 2006; 54: 273-278.
9. Johnson RJ, Segal MS, Srinivas T, Ejaz A, Mu W, Roncal C, et al. Essential hypertension, progressive renal disease, and uric acid: a pathogenetic link? J Am Soc Nephrol 2005; 16(7): 1909-1919.
10. Wang IK, Muo CH, Chang YC, Liang CC, Chang CT, Lin SY, et al. Association between hypertensive disorders during pregnancy and end-stage renal disease: a population-based study. Canadian Med Assoc J 2013; 185(3): 207-213.
11. Strevens H. Blood pressure, renal functional and structural changes, in normal and preeclamptic pregnancy. Helena Strevens, Department of Obstetrics and Gynecology, University Hospital, 2002;S-221 85 Lund, Sweden,.
12. Shlipak MG, Sarnak MJ, Katz R, Fried LF, Seliger SL, Newman AB, et al. Cystatin C and the risk of death and cardiovascular events among elderly persons. New Engl J Med 2005;352(20):2049-2060.
13. Hanratty R, Chonchol M, Havranek, EP, Powers JD, Dickinson LM, Ho PM, et al. Relationship between blood pressure and incident chronic kidney disease in hypertensive patients. Clin J Am Soc Nephrol 2011;6(11):2605-2611.
14. Taylor RN, Roberts JM, Gary Cunningham F, Lindheimer MD. Chesley's Hypertensive Disorders in Pregnancy. Academic Press, Elsevier, 4th Edition, 2014.
15. Cruz MO, W Gao, JU Hibbard. Obstetrical and perinatal outcomes among women with gestational hypertension, mild preeclampsia, and mild chronic hypertension. Am J Obstet Gynecol 2011;205(3):260.e1-260.e9.
16. Akolekar R, Bower S, Flack N, Bilardo CM, Nicolaides KH. Prediction of miscarriage and stillbirth at 11–13 weeks and the contribution of chorionic villus sampling. Prenat Diagn 2011;31(1):38-45.
17. Jivraj S, Anstie B, Cheong YC, Fairlie FM, Laird SM, Li TC. Obstetric and neonatal outcome in women with a history of recurrent miscarriage: a cohort study. Human Reprod 2001;16(1):102-106.
18. Cleary-Goldman J, Malone FD, Vidaver J, Ball RH, Nyberg DA, Comstock CH, et al. Impact of maternal age on obstetric outcome. Obstet Gynecol 2005;105(5,Part 1): 983-990.
19. Yelumalai S, Muniandy S, Omar SZ, Qvist R. Pregnancy-induced hypertension and preeclampsia: levels of angiogenic factors in Malaysian women. J Clin Biochem Nutr 2010;47(3):191-197.
20. Roberts JM, FG Cunningham, MD Lindheimer. Chesley's hypertensive disorders in pregnancy. Academic Press 2009;
21. Baert A, et al. Trends in contrast media. 2012: Springer Science & Business Media. 483.
22. Whelton PK, Perneger TV, He J, Klag MJ. The role of blood pressure as a risk factor for renal disease: a review of the epidemiologic evidence. J Human Hyperten 1996;10(10):683-689.
23. Wright Jr JT, Bakris G, Greene T. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial. JAMA 2002;288(19): 2421-2431.
24. Shulman NB, Ford CE, Hall WD, Blaufox MD, Simon D, Langford HG, et al. Prognostic value of serum creatinine and effect of treatment of hypertension on renal function. Results from the hypertension detection and follow-up program. The Hypertension Detection and Follow-up Program Cooperative Group. Hypertension 1989;13(5 Suppl): I80-193
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License