IJCRR - 13(7), April, 2021
Pages: 167-171
Date of Publication: 12-Apr-2021
Print Article
Download XML Download PDF
Functional Outcomes in Trans Femoral Amputees using Indigenously Developed Safe Gait Prosthetic Knee Joint
Author: Veerendra K. Shandilya, Parth Devmurari, Ashwinikumar V. Shandilya, Lata D. Parmar
Category: Healthcare
Abstract:Introduction: India has a large young population with limb loss, especially from low economic strata, trauma being the major cause, suddenly takes a toll on the finances of the amputees. A low-cost endo-skeletal prosthetic knee joint, named 'Safe Gait' has been designed and developed, with a mechanism of free knee joint with swing assist and a lock that can be operated at will and with ease by a patient at any point of time and terrain. Objective: The present study aims to assess the TFA using SGPKJ on the functional outcomes and compare to the patients wearing other imported prosthetic knee joint (OIPKJ) like polycentric knee joint, hydraulic knee joint, etc. It was hypothesized that SGPKJ would provide stability and mobility at a very low cost and thus could be an option for non-affording TFA. Methods: This was an 'Open-label' study. The participants who satisfied the inclusion criteria were divided into two groups based on their prosthetic options, they were compared on functional measures like single limb stance time in a sec, Time Up and Go Test, & Six Minutes' Walk Test. Results: Show single-limb stance as 1.39 sec & 1.48 sec; Gait speed as 1.37 m/sec & 141m/sec in Safe Gait Prosthetic Knee Joint and Other Imported Prosthetic Knee Joint resp. There was no statistically significant difference between the two groups in other parameters viz. TUG & 6MWT. Conclusion: The participants with SGPKJ were found to be compatible with mobility and stability on various locomotor tests.
Keywords: Functional outcomes, Six-minute walk test, Time up and go test, Transfemoral amputation, Prosthetic knee joints, Lower extremities amputations
Full Text:
Introduction
It is stated that 200-500 million major amputations each year are performed worldwide and 85% of these are lower extremities amputations (LEA).1 According to the sample survey of India 2011, approximately 2.2% of the population is living with a disability. That comes to around a 2.2million people living with disabilities. Limb loss is a life-changing event that can be overwhelming. Amputation (limb loss) is one of the commonly seen disabilities in our country.
Trauma being the major cause, with young amputees in India, it has been observed that most of these youth belong to the lower strata of the society and face a hard time coping up with the mainstream. The prosthetic technology in recent years has grown by leap & bounds. The most advanced prosthesis incorporates advanced gadgets like microprocessors; these are available with exorbitant costs.2,3 Most endo-skeletal prosthetic knee joints available in India are imported and are expensive. The most common & economical prostheses – Jaipur foot Prostheses- are fitted & distributed in camps free of cost. These above-knee prostheses have an Exoskeletal system with a pair of Orthotic drop lock for all its prosthetic fittings, this results in a stiff knee gait.4
There are three major groups in which the transfemoral amputees (TFA) prosthesis have been classified, viz. Passive, damping & powered.5 Worldwide endo-skeletal Prosthetic knee joints supplied are either free/ functional or with a locking mechanism, amputees do not have the option to self-lock or unlock the prosthetic knee. In India, on uneven inclined terrain as the prosthetic knee axis moves anteriorly and will tend to buckle, for stability needs on varied terrain conditions, overcrowded/rush situations, health issues, etc. locking option must be available to the TFA. Further, the design has to be such that not only is the cost of the prosthesis very low, but also the recurring expenditure of maintenance becomes much lower than at present. An endo-skeletal prosthetic knee joint was thus designed & developed keeping in mind the above factors and has been named as ‘SAFE GAIT.’
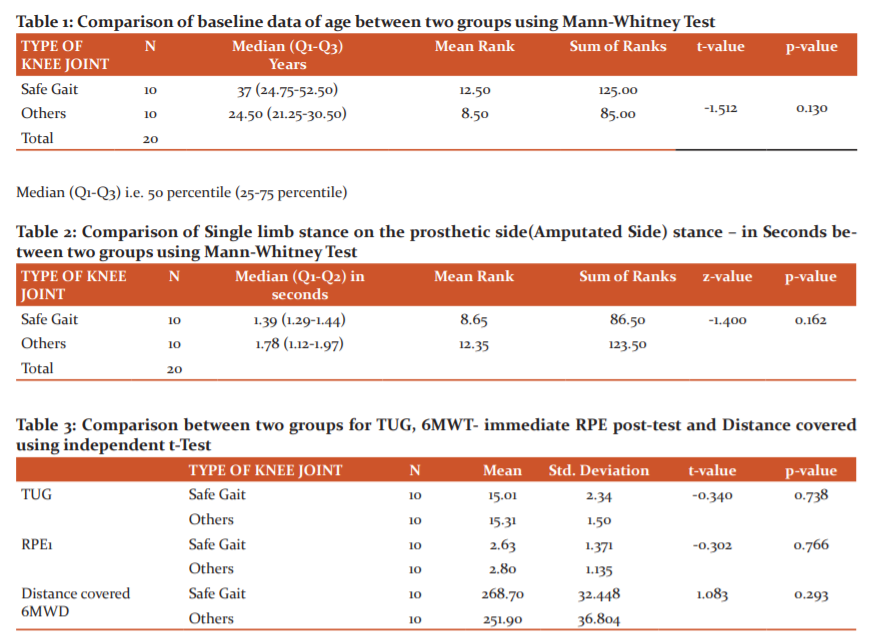
Design considerations for Safe Gait Prosthetic Knee Joint
Stainless Steel material was chosen for the manufacture of the knee joint because:
1. Titanium is costly and would take the cost too high.
2. Stainless steel would make the Knee Joint rust-proof (free of corrosion) and durable.
3. An investment casting has been done on the joint to make it cost-effective manufacturing.
4. Since there are no standard tests on knee joint testing available in the country, a prototype was manufactured with Stainless Steel 304 and a compression load test was done at ERDA (Energy Research Development Agency – an authentic autonomous body in the field of testing)
Technical Features
-
The Knee axis is behind (posterior) for stability
-
Extension assist is done with an elastic cord which is easily interchangeable and tension can be adjusted for the swing phase.
-
The lock mechanism works with a spring-loaded plunger, when the knob is shifted; it immediately locks the knee (in full extension)
-
Load Limit - 120 KGs, UNB 12.9
-
Knee Flexion Range – 125 degree (approx.)
-
Height (Knee centre – upper edge) - 22m
-
Optional height (Knee-Centre with special coupling) -12mm
-
Universal socket assembly features (which could be fitted to any prosthetic component manufacturer’s assembly system) - 30mm pylon tube fitting (Figure 1). The cost of the knee joint is only Rs. 2000/-this pilot study was planned to assess this safe gait prosthetic knee joint (SGPKJ) in trans femoral amputees (TFA) using simple functional tools. It was important to assess a single limb stance along with other functional tests like the ‘Timed Up and Go Test (TUG) and Six Minutes' Walk test (6MWT). The Time Up Go test is used to assess individuals' function in balance, transfer, walking, and turning around.6 Robert Gailey in 20027 is the first researcher to find 6MWT practical for measuring functional capabilities and endurance. 6MWT is also said to demonstrate good to excellent test-retest reliability as a measure of functional capacity in the population with lower limb amputees.
The present pilot study aimed to assess the TFA using SGPKJ on the functional outcomes as mentioned and this was compared to the patients wearing other imported prosthetic knee joint (OIPKJ) like polycentric knee joint, hydraulic knee joint, etc. It was hypothesized that SGPKJ would provide stability and mobility at a very low cost and thus could be an option for non-affording TFA.
MATERIALS AND METHODS
Study Design: Open-label study, Registered with CTRI
Procedure
After the institutional ethical clearance was obtained, the referred patients were approached. They were explained about the study and the prosthetic options available. All those patients agreeing to participate in the study were requested for written informed consent, they were provided with the written information sheet explaining the study. Following this, they were screened for inclusion & exclusion and Demographic data and education information with contact numbers were taken.
Patients were divided into two groups based on: -
-
On the economy (Price, fitting cost, annual maintenance cost)
-
Function with the prosthesis
-
Stability while weight-bearing with the prosthesis
-
Quality of life with the prosthesis
Inclusion criteria
-
Above-knee amputees
-
Age 16 years and above
-
Having unilateral TFA
-
Being able to read, write and understand & communicate
Exclusion criteria
-
Amputees with upper extremity amputations
-
Trans-tibial /partial foot amputees
-
Psychiatric disorders, hearing impaired and visually impaired persons with amputations.
-
Other neuromuscular problems, acute illness or chronic illness, and renal dialysis.
-
Mentally challenged persons with amputations
Comparison
GROUP A (1) - case (with ? safe gait prosthetic knee joint)
GROUP B (2) - patients fitted with other imported prosthetic knee joints
The simple outcome measures were used as follows:
-
Single limb stance time in secs
-
TUG
-
6MWT
The above procedures were performed as described below:
Single limb stance time was checked for a prosthetic limb. Eligible subjects were asked to stand with shoes on the prosthetic limb, with the normal limb raised allowed to touch the wall with the tip of a finger. For the test, standard procedure was followed i.e. each participant was asked to look at a point on the wall in front. The duration for which the participant was able to stand on his prosthetic limb with the other limb raised off the floor was timed and recorded. The test was terminated if the participant used his arms, moved his raised foot in an attempt to stabilize himself or shifted/rotated on his prosthetic leg/foot on the ground. The procedure was repeated 3 times, and the average of the 3 trials was recorded. In our study, we asked subjects to perform the test with the eyes open and ‘Gait belt’ in the parallel bar to ensure safety.
The TUG test required the subjects to rise from a chair, walk 3 meters at a comfortable pace to a marked place on the floor, turn around at the mark, and walk back to the starting point and return to sitting in the chair. The test's score is the time he/she takes to complete the test. This test assesses time taken in four components i.e. raising from sitting, walking, turning, and sitting back.
A six-minute walk test (6MWT) was performed as per guideline. At the outset, subjects were instructed to walk between starting and endpoints at a normal pace with their prosthesis in a marked 30 meters long corridor. Before the commencement of the test, the subjects were asked to sit comfortably for 10 minutes at least, following which vital parameters such as Pulse rate (PR), Respiratory rate (RR), and Rate of perceived exertion (RPE) were recorded. Vital parameters were taken before the test, post immediate, and 2 minutes after. The test was performed at a quiet and well-ventilated place so that commands at regular intervals could be audible to subjects. The test was carried out at room temperature and all necessary precautions like standby emergency services, test supervision by a senior therapist, and availability of a chair at a short distance were taken care of.
Statistical analysis
The data so collected were entered into Microsoft Excel for analysis. TUG, RPE, and 6MWT are assumed to be normal and are reported as mean (SD) whereas the age of patients and single-limb stance are assumed non-normal and hence are reported as median (IQR). An Independent t-test is used to compare TUG, RPE, and 6MWT between two types of knee joints whereas age and single-limb stance are compared using the Mann Whitney test. The significance level is set at 5% throughout the study.
Results
Total participants were 20 and all had similar comfortable ischial containment socket fittings with silicone socket having pin lock suspension and multi-axial foot with standard pylon; with 10 subjects fitted with SGPKJ all males & 10 subjects OIPKJ4- Polycentric knee joint, 3- four-bar linkage knee joint, 2- Stance control single-axis knee joint,1- Hydraulic knee joint. OIPKJ group had 8 males and 2 females.
Single limb stance – 1.393 sec. & 1.488 sec in SGPKJ & OIPKJ resp.
TUG – Average was 15.93 & 15.80 of SGPKJ and OIPKJ group
6MWT- Average RPE immediate posttest was 2.53 & 2.80 of SGPKJ and OIPKJ group
SPO2- varied between 96 -97.55
DISTANCE WALKED- was 268.70 m and 251.90 m for SGPKJ and OIPKJ group resp.
GAIT SPEED- 1.37m/s in the SGPKJ and 1.41m/s in the OIPKJ.
Discussion
Loss of limb is a huge trauma, physically, psychologically, and financially. It is known worldwide that lower limb amputations are common as compared to upper limbs. Transfemoral (above knee) amputations result in a greater loss of mobility and function due to the absence of knee and ankle-foot.8 Designers and innovators have focused their attention on developing prosthetic knee joints to provide near-normal functions. However, few designs have been successful.8 There is also not enough data on various functional / performance parameters despite several designs presented.9 In India, very few prosthetic knee designs have been developed. The Safe Gait Prosthetic Knee Joint designed and developed has been tested in the present study by comparing it with the Other Imported Prosthetic Knee Joints on various functional parameters using locomotor tests.
Single-limb stance <30 seconds with an assistive device is considered unsteady and graded as 0, but if the amputee can stand for 30 seconds with the support it was graded as 1; only if the single stance is unassisted >30seconds it is 2 or stable.7
In this pilot study, the two groups of the same age (Table 1) were compared, almost all were males (Figure 2), there was no statistically significant difference in the single-limb stance on the prosthetic limb unsupported between the two groups (Table 2) the patients did well if allowed to stand with minimal support or with a walking aid. This shows that the SGPKJ was also providing similar stability as was provided by the imported knee joints. A successful knee joint is expected to provide stability in the stance phase for adequate step and stride in gait thus helping the amputee to walk faster.9
The stability of the prosthetic knee is provided by design and alignment and this is essential to prevent the knee from buckling especially on uneven terrain as is common in our country.9 Gait speed in the present study was also found to be 1.37m/s in the SGPKJ and 1.41m/s in the OIPKJ. According to the author Caroline 2016, ≤0.44m/s was indicative of non-community ambulator and states traumatic amputee as having gait speed of 1.3m/s.10
With regards to TUG, literature reports range from 7.2 to 102 seconds and maybe slower for geriatric people with TFA.10 In the present study there was no significant difference between the groups for TUG (Table3). The TUG ranged from 13.68 to 20.19. Although it is well above the age-matched normal. The TUG reported by authors 2016 for the prosthetic users is 12.5 (9-20.8).10
With regards to 6MWT also, the two groups were not found statistically different. The average 6MWD was 262.7m with SGPKJ and 254.5m with OIPKJ. This distance is much lesser compared to the age-matched normal. Caroline 201610 reported 6MWD in prosthetic users as 274 (156-371). The vital parameters i.e. pulse rate, respiratory rat (Figure 3) and RPE (Table 3) measured were also not significantly different between the two groups. According to the literature, 6MWT is reported to vary from 4 to 858m in cohorts with LLA. The LLA’s with the inability to walk >200m nonstop are predicted to be inefficient community ambulator.10
To improve QOL, functional mobility, and develop functional independence following LLA, it is vital to undergo physiotherapy and rehabilitation as soon as possible.11 The above functional locomotor tests help identify the level of independence in the LLA and if found impaired could be targeted for improvement and modification by adopting various rehabilitation strategies like gait retraining, improve strength and balance, use of mobility aids, etc.10
Trauma is the major cause of young amputees in India however, India being the diabetes capital, diabetic foot ulcers are a high-risk factor apart from PVD for nontraumatic LEA. This indigenously developed SGPKJ would provide the option for millions in our country, as it is not only cost-effective, providing the ability to walk free at will but also have locking unlocking made easy for stability and mobility resulting in incompatibility on functional outcomes.12
Conclusion
The most advanced gadgets like microprocessors cannot be competed with. However, SGPKJ indigenously made, found to be statistically compatible with OIPKJ available on the mobility and stability tests, provides hope of affordable option to millions in our country.
Acknowledgement: Authors acknowledge the ‘Rehabs Clinic’ and ‘Sumandeep Vidyapeeth’. The authors also acknowledge the immense help received from the scholars whose articles are cited and included in references to this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
Conflict of Interests: Authors declare NIL conflicts of interests. No financial support received.
References:
-
Creylman V, Knippels I, Janssen P, Biesbrouck E, Lechler K, Peeraer L. Assessment of transfemoral amputees using a passive microprocessor-controlled knee versus an active powered microprocessor-controlled knee for level walking. Biomed Engi 2016;15(3):142.
-
Gailey RS, Roach KE, Applegate EB, Cho B, Cunniffe B, Licht S, et al. The amputee mobility predictor: an instrument to assess determinants of the lower-limb amputee's ability to ambulate. Arch Phys Med Rehab 2002;83(5):613-627.
-
Uchytil J, Janda?ka D, Farana R, Zahradník D, Rosicky J, Janura M. Kinematics of gait using bionic and hydraulic knee joints in transfemoral amputees. Acta Gymnica 2017;47(3):130-137.
-
Mahida H, Mahida D. Jaipur Foot: An Attempt to Replicate Jaipur Model in Surat City. NJCM India 2015;6:289-291.
-
Fu H, Zhang X, Wang X, Yang R, Li J, Wang L, et al. A novel prosthetic knee joint with a parallel spring and damping mechanism. Int J Adv Robo Syst 2016;13(4):1729881416658174.
-
Levin AZ. Functional outcome following amputation. Top Geriatr Rehabil 2004;20:253–261.
-
Gailey RS, Roach KE, Applegate EB, Cho B, Cunniffe B, Licht S, et al. The amputee mobility predictor: an instrument to assess determinants of the lower-limb amputee's ability to ambulate. Arch Phys Med Rehab 2002;83(5):613-62
-
Wilson AB, BSME J. Recent advances in above-knee prosthetics. Artif Limbs 1968;12(2):1-27.
-
Silver-Thorn MB, Glaister CL. Functional stability of transfemoral amputee gait using the 3R80 and Total Knee 2000 prosthetic knee units. JPO 2009;21(1):18-31
-
Roffman CE, Buchanan J, Allison GT. Locomotor performance during the rehabilitation of people with lower-limb amputation and prosthetic nonuse 12 months after discharge. Phys Ther 2016;96:985–994.
-
Ülger Ö, Y?ld?r?m ?ahan T, Çelik SE. A systematic literature review of physiotherapy and rehabilitation approaches to lower-limb amputation. Physiother Theory Pract 2018;34:821–834.
-
Nanjappa BA, Karthik P, Aroul TT, Smile SR. Risk factors for lower extremity amputation in patients with diabetic foot ulcers. Int J Curr Res Rev 2012;4(6):30-36.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License