IJCRR - 13(7), April, 2021
Pages: 124-131
Date of Publication: 12-Apr-2021
Print Article
Download XML Download PDF
Transactional Model of eGovernance: Empirical Evidence from the Healthcare Sector of India
Author: Sumeet Gill, Priya Vij
Category: Healthcare
Abstract:Introduction: A vast array of ICT based eGovernance initiatives are being put into practice in the healthcare sector in India to facilitate the populace and other stakeholders. However, a structural and strong healthcare management system postulates the development of an updated governance model. Objectives: The paper proposes to develop a Transactional Model governance model for the healthcare sector to augment the efficiency and social influence of eGovernance web portals. Methods: Twelve dimensions, extracted based on extensive literature review, models, NeSDA and UNDESA methodology and through Exploratory and Confirmatory Factor Analysis (EFA and CFA) have been used. Responses of 600 doctors, healthcare staff and patients have been collected through an in-depth interview and observation checklist. Structural Equation Modeling (SEM) has been applied to develop and propose a transactional model of governance after statistical testing. Results: The outcome depicts a significant positive impact of identified dimensions on Intention to Use and Service Quality construct of healthcare-related eGovernance services which ultimately improves efficiency thereby leading to social influence. Conclusion: The paper proposes an integrated and efficient governance model framework to enhance the social influence of eGovernance services in the healthcare sector. The promising outcome evinced that the proposed framework may serve as a roadmap for policy and decision-makers
Keywords: eGovernance, Efficiency, Corruption, Mismanagement, Resources, Social influence
Full Text:
INTRODUCTION
The coherent elevation and adoption of Information Communication Technology (ICT) driven eGovernance applications in the healthcare sector has transformed the mode of contact, connect and transact between hospitals, administrators, doctors, healthcare supporting staff and patients. The synthesis of the utility of ICT based eGovernance in the healthcare sector in India started with Mission Mode Projects (MMPs) of the National e-Governance Plan (NeGP) initially via using traditional communication technology viz. Electronic Media (Community Radio, and telephone), and gradually elevated to use of state-of-the-art technology viz. Video and Teleconferencing (Telehealth, Tele-medicine and Tele-referrals, online video consultations); Internet?enabled Web-based centres (Information kiosks, common service centres, eOffice, eHospital, voice web etc.); and Cloud-based eHealth and hospital administrative services. The NeGP 2.0, eKranti, and Digital India movement facilitates services like Aadhar based online registration, appointments, payments, access to diagnostic reports, real-time tracking of data and registrations, efficient information management, patient monitoring, medical education and communication, Vaccine Tracker, eRakt Kosh); Online Medical Counseling and Admissions, online continuous medical education courses through webinars and live streaming; Swasth Bharat (Disease, Lifestyle, First Aid), NHP Indradhanush; eHMIS, Ayushman Bharat – Health and Wellness Centre (HWC) portal, Integrated Disease Surveillance Programme (IDSP) Portal, Mera Aspataal – patient Feedback mechanism and many more.1
The thrust of the National Health Policy (NAP) supported by the Digital India initiative is on augmenting the eGovernance revolution by offering medical facilities through the web, mobile, and cloud (MeghRaj) accessible to the populace equitably round the clock.2 Ministry of Health and Family Welfare (MoHFW), Government of India is endorsing eHealth to develop an efficient, evidence-based, ethical healthcare system that shall encourage, educate, and empower patients and other stakeholders through information dissemination thereby improving public healthcare delivery.1 However, the current COVID 19 pandemic situation raised a serious question about our health machinery.
Over the years governments and bureaucrats considered healthcare only as a medical subject and ignored the acute need for a structured health management system for the second largest populated country. India ranked 145 as per Global Healthcare Access and Quality (HAQ) index, ranks lower than Bangladesh, Sri Lanka, Bhutan and Sudan and also slipped to 150th rank in healthcare and survival as per World Economic Forum (WEF).3,4 Health staff always remain under stress due to scarcity of infrastructural and human resource i.e. one government doctor on 10,189 residents, one government bed on 2,046 residents and one government hospital on 90,343 residents.5
On the other hand, the Supreme Court of India has termed patient care as ''deplorable” and ''pathetic”, as patients are running from pillar to post to get admission to hospitals, whereas a large number of beds are lying vacant in the hospitals.6 The problem is not merely inadequate resources i.e. infrastructure and human, but also mismanagement of health institutions. Furthermore, not much attention is being paid to ethical issues related to the adoption of technology and the safety of personal and sensitive information related to patients.8 Besides, the most serious ethical crisis i.e. corruption in the healthcare sector is poorly addressed and doctors and hospital staff are key actors behind the same.7,8 20% of health costs in the country is due to corruption and there is corruption in healthcare education as well.9 The Organisation for Economic Co-operation and Development (OECD) estimates that 45 % of global citizens believe that the health sector is corrupt or very corrupt. Insufficient regulatory oversight and lack of transparency in governance breed corruption and reduce the quality of healthcare services.10
Apart from issues related to infrastructural, human resources, mismanagement, poor GDP allocation4 and inadequate attention towards governance11 are responsible for the pathetic situation of healthcare in India. The outcome of various research studies has established a significant correlation between poor governance and mismanaged public healthcare services across countries.12 The gaps are visible between the ground realities and the policies framed to address them.
Many strategies exist for making the healthcare environment conducive, viz. adequate funding to the public healthcare system, remunerating health care workers adequately, ensuring social accountability, etc. but eGovernance is the most vital and cost-effective strategy for the national healthcare system to work optimally.10 The induction of web, mobile and cloud-based portals in native languages has enhanced the popularity of healthcare-related eGovernance services among all and the healthcare sector steadily advanced from the eGovernance transactional phase to transformational phase i.e. participation of end-users in decision and policymaking and implementation.10
With the proliferation of information channels, the expectations of the patients related to the accessibility of public health services in a convenient, integrated, transparent, and cost-effective manner have been boosted. However, the complexity of the eGovernance in the healthcare sector has enhanced with time. The contrary research outcomes and amplified implementation challenges encouraged researchers, governing institutions and research labs towards the development of an eGovernance model viz. “DeLone and McLean IS Success Model (DandM Model), Technology Acceptance (TAM) model, Theory of Planned Behavior (TPB), Gartner's Four Stage Model, Layne and Lee Four-Stage Model, Heeks Design Reality Gap Model, Theory of Reasoned Action (TRA), Structuration Model of Technology (SMT), United Nations Five-Stage Web Presence Measurement Model, Diffusion of Innovation (DOI), Unified Theory of Acceptance and Use of Technology (UTAUT), and Theory of Planned Behavior (TPB), Heeks Onion Ring Model, EGOVSAT model” and many more to enhance the competence of the eGovernance initiatives. However, a significant gap in the expansion of existing theoretical and technology-oriented models conceptually and practically is evident in research outcomes.13 Further, the enormous failure rate of eGovernance initiatives supported by research gaps necessitates rapid and consistent horizontal and vertical assessment from the stakeholders’ perspective.
National e-Governance Service Delivery Assessment 2019 (NeSDA) assessed eGovernance services portals of six sectors (Finance, Labour & Employment, Education, Local Government & Utilities, Social Welfare, Agriculture, Health and Environment) based on seven key constructs i.e. Accessibility, Ease of use, End service delivery, Integrated service delivery, Content Availability, Information security & privacy, and Status & Request tracking, based upon Online Service Index (OSI) of UNDESA eGovernment Survey in 2019 and published survey outcome in February 2020.14 The low level of stakeholders’ satisfaction evinced in the survey particularly related to health sector demands for development of an integrated model and with this in view, the present paper proposes to develop a transactional model of eGovernance for healthcare sector from stakeholders’ perspective, with emphasis on enhancing efficiency and social influence of eGovernance web portal.
MATERIALS AND METHODS
The process of model development encompasses various phases, exploring the dimensions of eGovernance using EFA by collecting responses from 600 doctors, healthcare staff and patients through in-depth interview related to twelve dimensions i.e. “Performance Expectancy, Compatibility, Job Fit, Facilitating Conditions, Intention to Use, Ease of Use, Competence, Reliability, Usefulness, Responsiveness, Product Portfolio, and Security dimensions” extracted based on extensive literature review, models, NeSDA and UNDESA survey methodology. The extracted dimensions and their relationship were affirmed using CFA.
The healthcare staff involved in governance projects serving at Central and State-funded Post Graduate Institutions of Medical Sciences (PGIMS) and patients were considered as sample unit and 600 respondents were selected based on Judgment sampling. The doctors and healthcare staff having more than three years of experience in eGovernance activities and patients possessing Smartphone with hands-on knowledge, ready to interact and participate were included in the study.
The respondents were contacted through Snowball Approach and responses were recorded on Likert Seven Point Summative Scale (SD (1) to SA (7)) through an in-depth interview and observation checklist. The data were tabulated and statistically analyzed using open source software “Jamovi” Version 0.9.5.12 and EFA, CFA, SEM was applied. The respondents were apprised regarding the objectives of the research before starting the interview. Further, the respondents were assured that their identity shall not be revealed.
RESULTS AND DISCUSSION
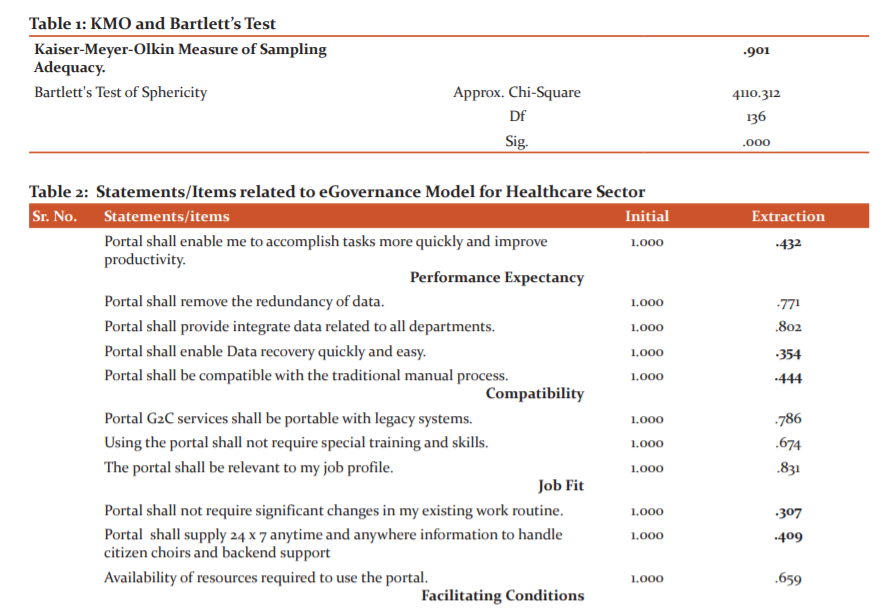
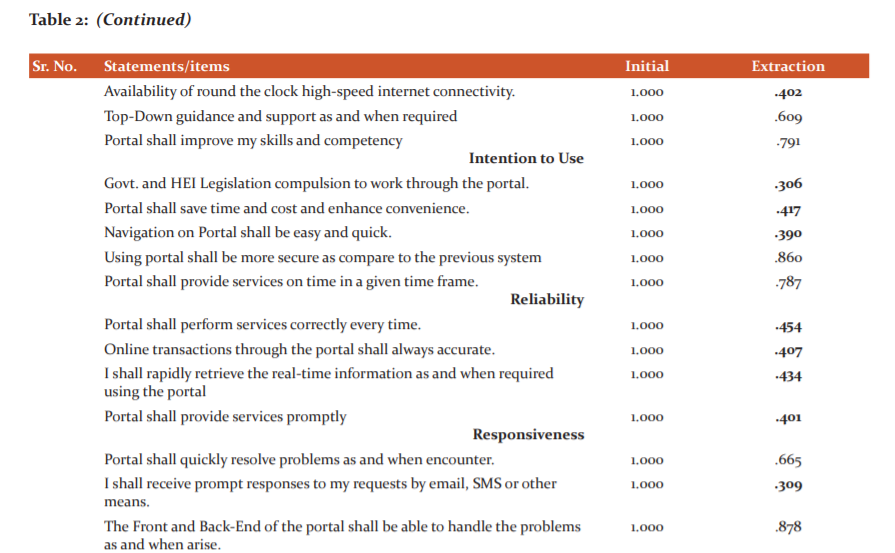
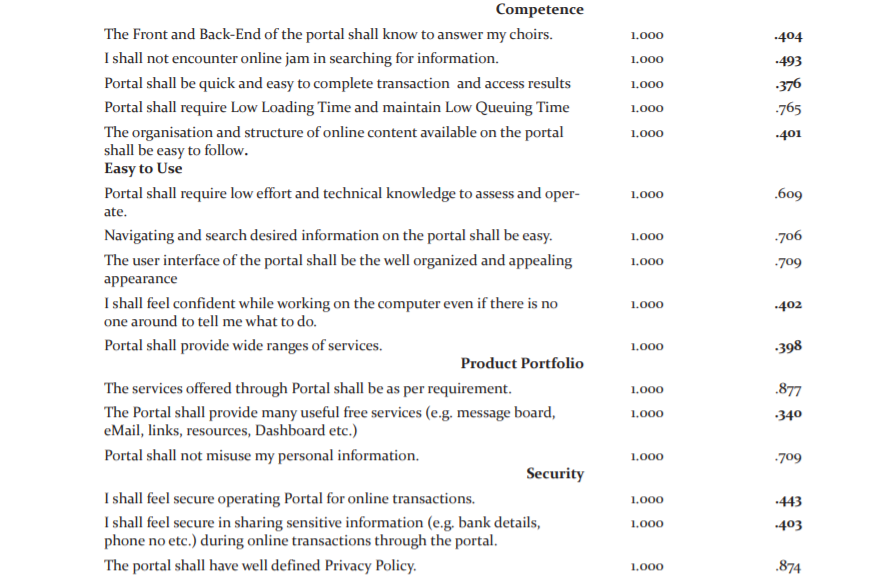
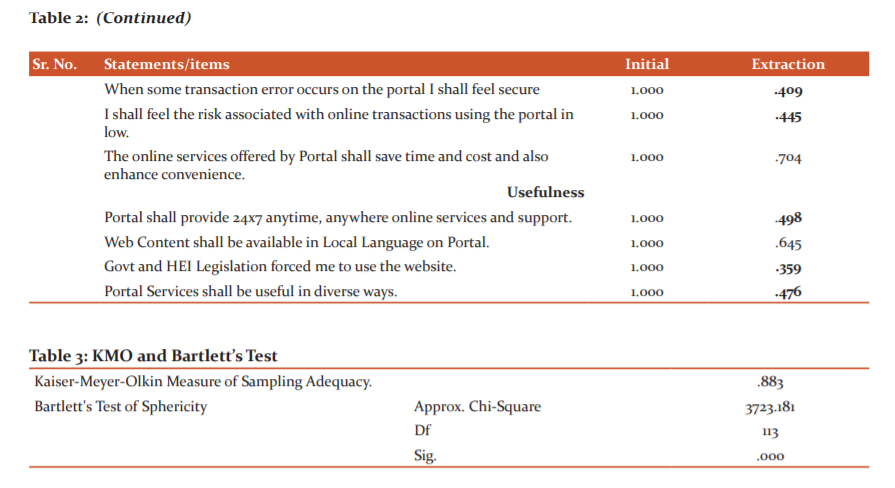
The value of the Kaiser-Meyer-Olkin (KMO) test of Sampling Adequacy was 0.907 and the P Value of Bartlett’s Test of Sphericity was less than 0.05, which endorse the application of EFA (Tables 1 and 2). The principle Components Analysis (PCA) method was applied to execute EFA. All extracted factors having Eigenvalue >1 were retained for further analysis.
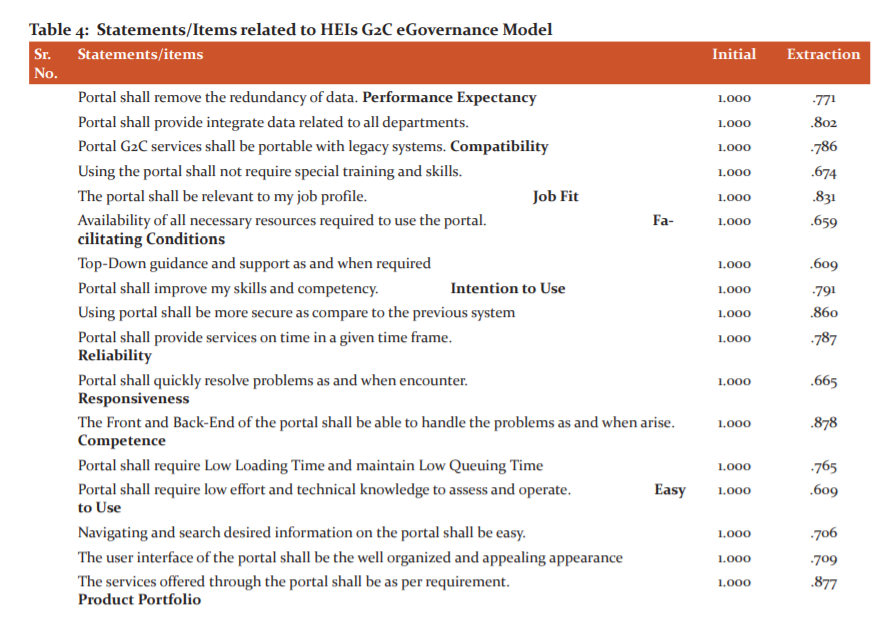
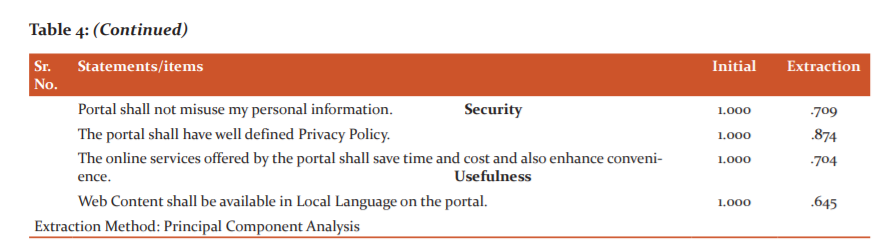
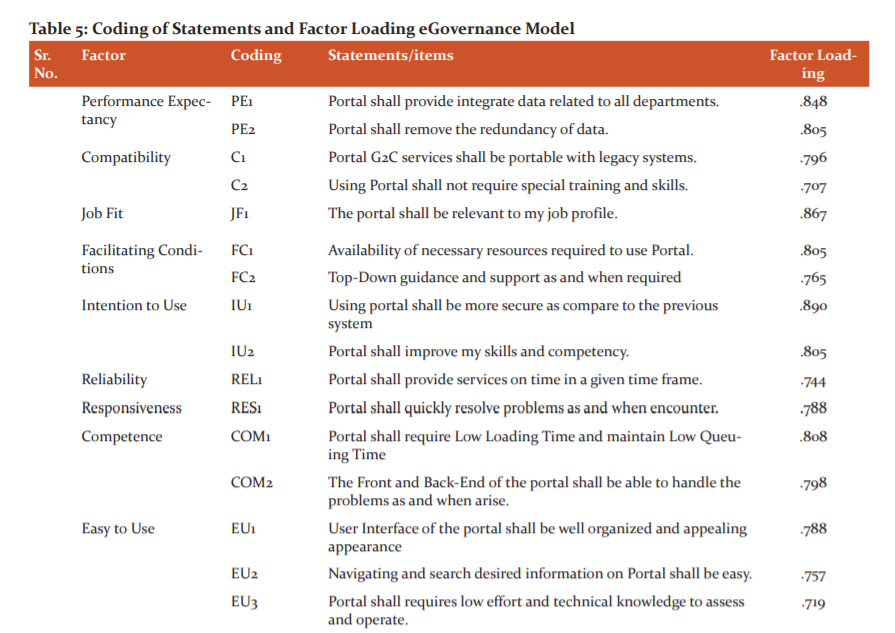
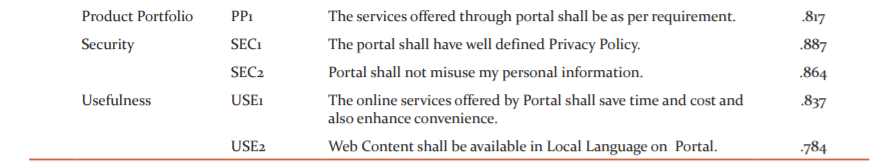
Tables 3 and 4 explained extraction of 28 statements due to communality value less than 0.50, data adequacy and existence of relationship among the 21 remaining statements on which final EFA was applied. The cumulative percentage of variance was 70.546 that inferring 70 per cent of eGovernance portal efficiency is explained by these twelve dimensions. Further, CFA was applied for overall construct validation and statements falling in each of the factors derived from EFA were tabulated in Table 5.
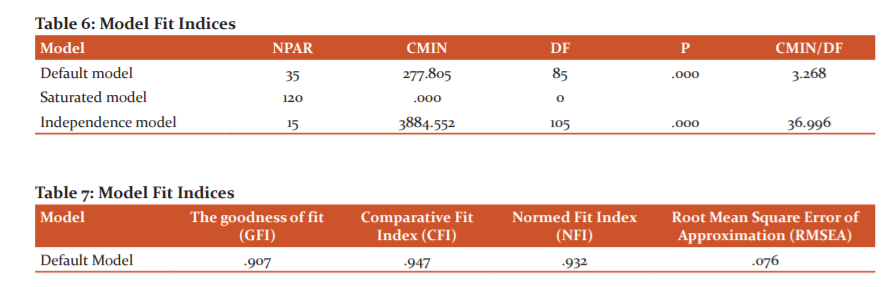
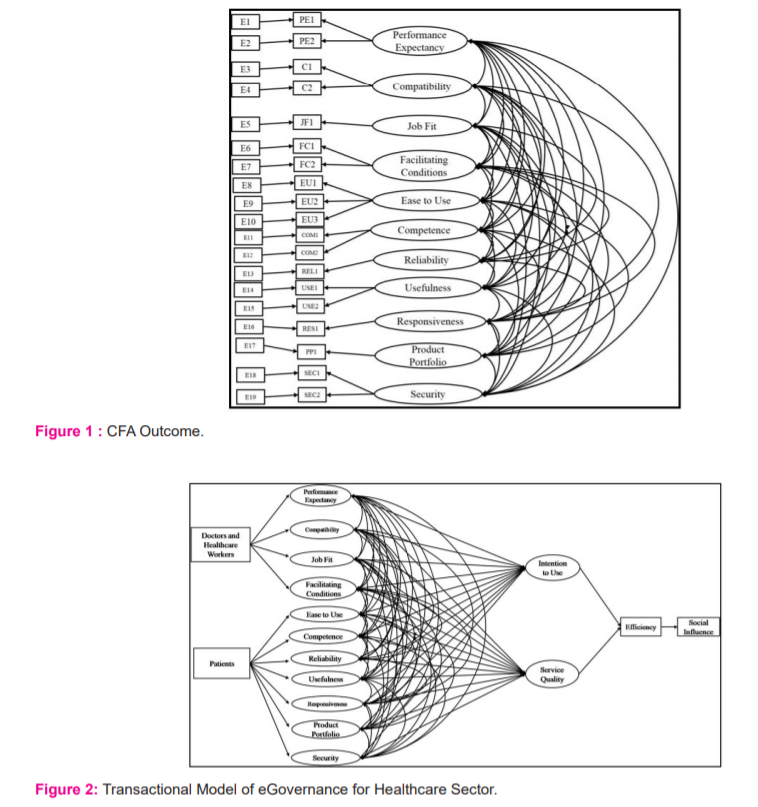
CFA was applied on twelve dimensions and model fit indices/summary (Table 6) and GFI, CFI, NFI and RMSEA values tabulated in Table 7. CFI value of 0.9 and above testifies strong unidimensionality; GFI value of more than 0.9 shows the best fit of the model, and value of RMSEA 0.079 also makes the model acceptable. The relationships between the statements and factors were strong and significant (Figure 1). All the relevant assumptions of SEM were satisfied and the transactional model of eGovernance for the healthcare sector proposed in Figure 2.
CONCLUSIONS
The outcome depicts the significant positive impact of “Performance Expectancy”, “Compatibility”, “Job Fit”, “Facilitating Conditions”, “Ease of Use”, “Competence”, “Reliability”, “Usefulness”, “Responsiveness”, “Product Portfolio”, and “Security” on Intention to Use and Service Quality constructs of eGovernance which ultimately improves the efficiency of the eGovernance in the healthcare sector and efficiency leads to positive social influence. The proposed transactional model of governance will guide the policymakers to focus on identified constructs to enhance and maintain efficiency and social influence. The suggested model may be tested after integrating it with new constructs based on empirical outcomes for an update. However, the masses will not be benefited unless administrative, social and political measures ensure equitable access to all.
ACKNOWLEDGEMENT
The authors acknowledge the help of the open source society for providing software’s access required for statistical analysis. The authors acknowledge the immense help received from the scholars whose articles are cited and included in references to this manuscript. The authors are also grateful to authors/editors/publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
Source of Funding: Self Funded
Conflict of Interest: Non
References:
-
Phanish C. e-Governance in Indian Healthcare Building a Stronger Nation. eHealth The Enterprise of Healthcare. 2017; https://ehealth.eletsonline.com/2017/07/e-governance-in-indian-healthcare-building-a-stronger-nation/
-
e-Health India, NHP Admin. 2017. https://www.nhp.gov.in/e-health-india_mty
-
Vinay A. COVID-19 – Mismanagement and urgent need for Indian Medical Services. The Northline [Internet]. 2020 July. http://www.thenorthlines.com/covid-19-mismanagement-and-urgent-need-for-indian-medical-services/
-
Medical Dialogues Bureau. India Slips To 150th Rank In Healthcare: World Economic Forum. Medical Dialogues [Internet]. 2019 Dec 17. Available from: https://medicaldialogues.in/india-slips-to-150th-rank-in-healthcare-world-economic-forum?infinitescroll=1
-
Sanchita S. India’s public health system in crisis: Too many patients, not enough doctors. Hindustan Times [Internet] 2017 August 29. Available from: https://www.hindustantimes.com/india-news/public-health-system-in-crisis-too-many-patients-not-enough-doctors/story-39XAtFSWGfO0e4qRKcd8fO.html
-
Sumit S. Delhi govt hospitals a spectacle of mismanagement (IANS Investigation) (Delhi Health Emergency-II). Outlook [Internet]. 2020 June 13. https://www.outlookindia.com/newsscroll/delhi-govt-hospitals-a-spectacle-of-mismanagement-ians-investigation-delhi-health-emergencyii/1865342
-
Sanjay K. Health care is among the most corrupt services in India. BMJ 2003;4(10):326-37.
-
Subrata C. Corruption in healthcare and medicine: Why should physicians and bioethicists care and what should they do? Indian J Med Ethics 2013;10(3):153-159.
-
Corruption blamed for healthcare sector woes. The Hindu [Internet]. 2019. https://www.thehindu.com/news/cities/kozhikode/corruption-blamed-for-healthcare-sector-woes/article26361494.ece
-
Crossing the Global Quality Chasm: Improving Health Care Worldwide. National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Board on Global Health; Committee on Improving the Quality of Health Care Globally. Washington (DC): National Academies Press (US); 2018. https://www.ncbi.nlm.nih.gov/books/NBK535646/
-
Chandrasekhar CP, Jayati G. Covid-19: Why is India faring worse than its neighbours?. Business Line [Internet]. 2020 August 11. https://www.thehindubusinessline.com/opinion/columns/c-p-chandrasekhar/covid-19-why-is-india-faring-worse-than-its-neighbours/article32318486.ece
-
Maureen L. Governance and Corruption in Public Health Care Systems. Center for Global Development. 2006. Working Paper Number 78. http://www1.worldbank.org/publicsector/anticorrupt/Corruption%20WP_78.pdf
-
Anita V, Smriti S, Deboshree G. Impact of E-Governance Practices on Agriculture Sector of India. CASS Studies. 2019; 3(1), 294-307. http://heb-nic.in/cass/admin/freePDF/kji8rwvj50kbxuba8lwc.pdf
-
Alawneh A., Al-Refai H., Batiha K. Measuring user satisfaction from eGovernment services: lessons from Jordan. Government Information Quarterly. 2013; 30(3), 277–288. DOI:https://doi.org/10.1016/j.giq.2013.03.001
-
Department of administrative reforms and public grievances (India). National e-Governance Service Delivery Assessment 2019, e-Governance Landscape – India’s Transformative Journey. New Delhi: Department of administrative reforms and public grievances, Ministry of personal grievances and pensions, Government of India; 2020. https://www.nesdaportal.in/NeSDA_2019_Final_Report.pdf
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License