IJCRR - 13(7), April, 2021
Pages: 16-19
Date of Publication: 12-Apr-2021
Print Article
Download XML Download PDF
To Evaluate the Sleep Pattern in Children with and without Developmental Co-Ordination Disorder
Author: Sujatha Baskaran, Jagatheesan Alagesan, Pooja K, Thirumal S
Category: Healthcare
Abstract:Background: The sleep pattern about developmental coordination disorder has been studied less. Objective: To evaluate the Sleep Pattern in Children With and Without Developmental Coordination Disorder. Methods: The Study designed as an Observational Study, Study setting done at Schools in the Chennai district and the sam�pling method is the Conventional sampling method. The sample size is 14 School going children. Boys and girls between 9-14 years, Children without musculoskeletal disorders and Children who scored 15-57 in the DCD 07 questionnaire were included. Subject with a history of respiratory illness, Subjects with existing cardiovascular disease, Subjects who are already in the treat�ment program, Subjects with neurological and sensory impairment and Subjects with any congenital deficit were excluded. The material required is DCD07 Questionnaire, BOT-02 and the Children sleep habit questionnaire. Results: On comparing sleep habit in DCD children with non-DCD children, the results of the current study shows the significant p-value < 0.0001 and t- value 27.46. Conclusion: The incidence and prevalence of DCD to be higher in boys than in girls, this child exhibits poor sleep habits when compared to children without DCD. This study suggests that parents of DCD children must be made aware of the condition and this should be treated earlier and other psychosocial problems should be addressed at the earliest.
Keywords: Sleep pattern, DCD, School children, Questionnaire, DSMV
Full Text:
INTRODUCTION
In general, many clinical conditions may Impact motor skills such as epileptic syndromes, autism spectrum disorders, Attention Deficit Hyperactivity Disorder (ADHD), primary headache, learning disorders, and obesity. Whereas, when motor coordination is primarily impaired, Developmental Coordination Disorder (DCD) may be identified.1
Developmental coordination disorder is characterized by significant difficulty in the development of motor skill in the absence of obvious sensory or neurological impairment. Children with DCD struggle to perform everyday movement tasks requiring fine manipulation, eye-hand coordination and balance and agility.2 Sleep disturbance is common in groups of children with other neurodevelopmental disorders and psychiatric disturbances, such as anxiety and depression.2,3
Previous studies have estimated that the prevalence of sleep disturbance in typically developing children is in the range of 20-40% conversely, the prevalence of sleep disturbance in children with developmental disorders, such as Pervasive developmental disorder (PDD) and Attention deficit hyperactivity disorder (ADHD), has been reported to the two to three-fold higher.1
Many children with DCD perform poorly at school despite average intellectual ability and may fail to achieve their academic potential. A range of socio-economical problems has also been reported, including low self-esteem, high anxiety and poor peer relations. Emotional and behavioural problems are seen in populations of children with a range of other developmental disorder, which suggests that the link impaired motor function may not be direct.2
The current study has compared the sleep pattern of typically developing children with developmental coordination disorder, evaluated rate of sleep disturbance are continuously reported in children with the range of medical and psychiatric conditions and developmental disorder.2 The children sleep habit questionnaire (CSHQ) has been used in several countries to assess children sleep patterns and sleep problems as reported by parents.1
Thus many of the adverse effects may be rectified by addressing sleep disturbances, to enhance the overall functioning of the child and family. The children sleep habit questionnaire has high validity and reliability, specifically designed for school-aged (9 years to 14 years) children, the design of children sleep habit questionnaire is based on common clinical symptom presentations of the most prevalent pediatric international classification of sleep disorders diagnoses.5
The BOT-02 tool of motor proficiency is a standardized, norm-referenced measure used by the physical therapist in the clinic and school practice settings. The BOT-02 tool is an individually administered measure of fine and gross motor skills of children 9 through 14 years of age. It is intended for use by practitioners and researchers as a discriminative and evaluative measure to characterize motor performance, specifically in the areas of fine motor control, manual coordination, body coordination, strength and agility.6 The aim is to evaluate the sleep pattern in children with and without developmental coordination disorder.6,7
MATERIALS AND METHOD
The Study designed as an Observational Study, Study setting done at Schools in the Chennai district and the sampling method is the Conventional sampling method. The sample size is 14 School going children. Boys and girls between 9-14 years, Children without musculoskeletal disorders and Children who scored 15-57 in the Developmental coordination disorder 2007 DCD 07 questionnaire were included. Subject with a history of respiratory illness, Subjects with existing cardiovascular disease, Subjects who are already in the treatment program, Subjects with neurological and sensory impairment and Subjects with any congenital deficit were excluded. Materials required are developmental coordination disorder 07 questionnaires, BOT-02 and children sleep habit questionnaire.
A total of 414 school-going children were screened after obtaining permission from the school heads, detailed study procedure was being explained to the parents, teachers and children. Written informed consent was obtained from the parent or guardian. Children were allocated in two groups. Group A consisted of 14 children with developmental coordination disorder, who scored 15-57 in the DCD-07 Questionnaire and Group B consisted of 14 children without Development coordination disorder.
The outcome measure used in the study is, Diagnostic and Statistically Manual of Mental disorder (DSM V) has four criteria to rule out Development coordination disorder and they are,
Criteria-A: The acquisition and execution of coordinated motor skills are substantially below the expected given the individual chronological age and opportunity for skill learning and use. Difficulties are manifested as clumsiness (e.g., dropping or bumping into objects) as well as slowness and inaccuracy of performance of motor skills (e.g., catching an object, using scissors or cutlery, handwriting, riding a bike or participating in sports.)
Criteria-B: The motor skills deficit in criterion A significantly and persistently interferes with activities of daily living appropriate to chronological age (e.g., self-care and self-maintenance) and affects academic/ school productivity, prevocational and vocational activities, leisure and play.
Criteria-C: The onset of symptoms is in the early developmental period.
Criteria-D: The motor skills deficits are not better explained by intellectual disability (intellectual developmental disorder) or visual impairment and are not attributable to a neurologic condition affecting movement (e.g., cerebral palsy, muscular dystrophy, degenerative disorder).
To fulfil the Criteria- A of DSM V, The Bruininks- Oseretsky test of motor performance 2 (BOT 2) tool was also used to assess the motor function of children with DCD. Scores greater than 25 indicates well about average (WAA) motor function, 20 to 24 indicates above average (AA) motor function, 11 to 19 indicates the average motor function, 6 to 10 indicates below average (A) motor function, and less than 5 indicates well below average (WBA) motor function respectively.
To fulfil Criteria-C of DSM V, the parental interview was conducted by the researcher about the onset of developmental symptoms of other children.
To fulfil Criteria- D of DSM V every child with probable DCD was assessed by the physician to rule out any other major illness and neurological disorder.
RESULTS
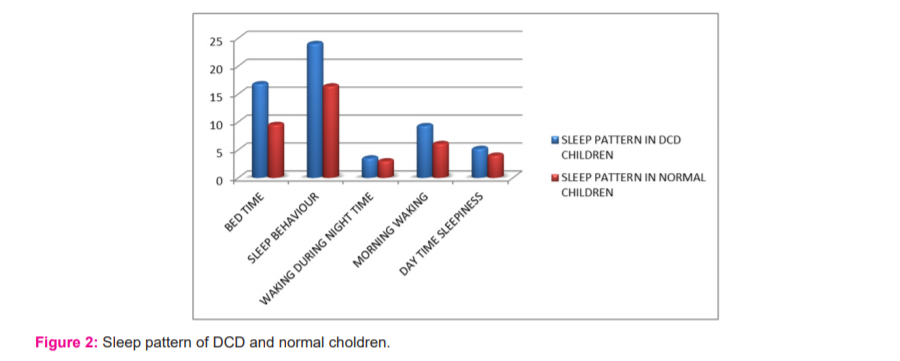
The number of subjects screened for this study was 414 out of which 14 (4.8%) subjects were found to be under DCD criteria. In gender distribution among the 14 subjects, 9(64.3%) were boys and 5(35.7%) were girls who have DCD. According to the data collected, the DCD children have an increased sleep pattern compared to the normal children, you have a normal sleep pattern. Based on the children sleep habit questionnaire the mean values of individual subscales were calculated. DCD children showed 28.7% (16.79) at bedtime, 41.1% (24) in sleep behaviour, 5.4% (9.29) in morning waking and 8.9% (5.21) in Day time sleepiness. On comparing sleep habit in DCD children with non-DCD children, the results of the current study show a significant p-value <0.0001 and t- value 27.46 (Table 1).
DISCUSSION
In this current study after the screening process, 20 of the children have been identified as children with DCD. In gender distribution among the entire subjects, 14 were boys (70%) and 6 were girls (30%). The total prevalence of DCD in the present study is 4.8%. Out of 20 subjects, 6 were dropouts and 14 were included in the study. According to the analyses of the children sleep habit questionnaire the sleep habit of DCD children is high compared to the normal children, and they exhibited poorer sleep quality when compared to children without DCD( Figure 1,2).5,6
Based on the children sleep habit questionnaire the individual subscale for DCD children had mean values of 28.7% (16.79) in bedtime, 41.1% (24) in sleep behaviour, 5.4% (9.29) in morning waking and 8.9% (5.21) in Day time sleepiness. As per the result of the children sleep habit questionnaire category, the sleep habit is higher in children with DCD.8,9 The present cross-sectional school-based survey indicates that poor sleep quality in children with developmental disorders may affect academic performance. Physicians need to be aware of age-related differences in the sleep problems exhibited by children with developmental disorders, and further studies are needed to explore, further associations between sleep quality and school behavioural as well as academic, performance. The high rates of reported sleep disturbance seen in the current study, along with what is known about the links between impaired sleep and impaired day time functioning.7,10,11 Raise the possibility that, for the children with DCD, sleep disturbance could be playing some role in the development or maintenance of the socio-economical problems from which they have been described to suffer.12,13
In 2012 Barnett et al. has explored the possible relationship between DCD and sleep, highlighting that subscale scores indicated particular problems with bedtime resistance, parasomnias and daytime sleepiness, and no di?erence between the groups for sleep onset delay, sleep duration, night waking, and sleep-disordered breathing, suggesting that sleep patterns of children with DCD may be of clinical relevance. In general, the close relationship between sleep and motor skills is well known.14,15
CONCLUSION
According to the study, the prevalence of DCD among school children is 4.8%. The incidence and prevalence of DCD to be higher in boys than in girls, this child exhibits poor sleep habits when compared to children without DCD. This study suggests that parents of DCD children must be made aware of the condition and this should be treated earlier and other psychosocial problems should be addressed at the earliest.
Acknowledgement: We thank all the participants, school teachers, parents, our institution and our team for helping us to complete this study.
Funding: Nil
Conflict of interest: No conflict of interest.
References:
1. LeBourgeois MK, Hale L, Chang AM, Akacem LD, Montgomery-Downs HE, Buxton OM. Digital media and sleep in childhood and adolescence, Pediatrics 2017;140(2):S92-6.
2. Gringras P, Green D, Wright B, Rush C, Sparrowhawk M, Pratt K, et al. Weighted blankets and sleep in autistic children - A randomized controlled trial. Pediatrics 2014;134(2):298-306.
3. Cattane N, Richetto J, Cattaneo A. Prenatal exposure to environmental insults and enhanced risk of developing Schizophrenia and Autism Spectrum Disorder: focus on biological pathways and epigenetic mechanisms. Neurosci Biobehav Rev 2018;4:123-126.
4. McLeod KR, Langevin LM, Goodyear BG, Dewey D. Functional connectivity of neural motor networks is disrupted in children with developmental coordination disorder and attention-deficit/hyperactivity disorder. NeuroImage Clin 2014;4:566-575.
5. Schoemaker MM, Niemeijer AS, Reynders K, Smits-Engelsman BC. Effectiveness of neuromotor task training for children with developmental coordination disorder: a pilot study. Neural Plast 2003;10.
6. Missiuna C, Moll S, King S, King G, Law M. A trajectory of troubles: parents impressions of the impact of developmental coordination disorder. Phys Occup Ther Pediatr 2007;27(1):81-101.
7. Polatajko HJ, fox M, Missiuna C. An international consensus on children with developmental coordination disorder. Can J Occup Ther 1995;62:3-6.
8. Henderson SE, Sugden DA, Barnett AL. Movement Assessment Battery for Children, 2nd edn. London: Pearson, 2007.
9. Schoemaker MM, flapper B, Verheij NP, Wilson BN, Reinders-Messelink HA, de Kloet A. Evaluation of the developmental coordination disorder questionnaire (DCDQ) as a screening instrument. Dev Med Child Neurol 2006;48(8):668-673.
10. Magalhães LC, Missiuna C, Wong S. Terminology used in research reports of developmental coordination disorder. Dev Med Child Neurol 2006;48(1):937-941.
11. Mandich AD, Polatajko HJ, Rodger S. Rites of passage: understanding participation of children with developmental coordination disorder. Human Movement Sci 2003;22(4-5):583-595.
12. Magalhães LC, Missiuna C, Wong S. Terminology used in research reports of developmental coordination disorder. Dev Med Child Neurol 2006;48(1):937-941.
13. Wilson BN, Kaplan BJ, Crawford SG, Campbell A, Dewey D. Reliability and validity of a parent questionnaire on childhood motor skills. Am J OccupTher 2000; 54(5):484-493.
14. Terzano M, Parrino L, Smerieri A, Carli F, Nobili L, Donadio S, et al. CAP and arousals are involved in the homeostatic and ultradian sleep processes. J Sleep Res 2005;14:359-368.
15. Biotteau M, Péran P, Vayssière N, Tallet J, Albaret JM. Neural changes associated to procedural learning and automatization process in Developmental Coordination Disorder and/or Developmental Dyslexia. Eur J Paediatr Neurol 2017;21(2):286-299.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License