IJCRR - 8(2), January, 2016
Pages: 46-56
Print Article
Download XML Download PDF
EVALUATION OF SUPPORT SERVICES NEEDED FOR PEOPLE LIVING WITH HIV (PLWH) ATTENDING RETRO CLINIC, TERTIARY CARE HOSPITAL AND ART PLUS CENTER, KARNATAKA, INDIA
Author: Mohammad Haghighatpanah, Ateendra Jha, Jeni Mary Joy, Rajesh Radhakrishnan, Danturulu Muralidhar Varma
Category: Healthcare
Abstract:Introduction: Human Immunodeficiency Virus (HIV) that reasons Acquired Immunodeficiency Syndrome (AIDS) has become one of the world's most alarming health-related problem. In developing countries like India AIDS have not only impact on physical health but also have retarding impact on Social and Psychological status of patients. People living with HIV/AIDS(PLWHA) may lose career, income, and even friends and family members as significant resources of assistance and support. The quality and organization of medical care for HIV-infected patients in any setting inevitably reflect the functioning of the health services in general. Aim: To evaluate support services needed for people living with HIV(PLWH) using validate questionnaire. Methodology: Validated survey questionnaire was used to evaluate the support services needed for HIV positive patients at Retro Clinic at Kasturba Hospital, (RCKH) Manipal and ART Plus center Udupi( ARTPCU ). We used both qualitative and quantitative research methodologies, including questionnaires and interviews of 120 patients receiving ART. Result: A total of 120 HIV patients were enrolled in the study, we found that 102(85.0%) got tested for HIV on Doctor's suggestion while 18(15%) got tested by their own will. In RCKH (87.0%) waiting time was about 30-60 minutes while in ARTPCU (92.4%) it was less than 30 minutes. Most of the patients at either of the centers received counseling (76.7%) and were satisfied (94.2%). Economic support was available in ARTPCU but not in RCKH. Majority (56.7%) of the patients were on HAART since 1-5 years while only four (3.3%) were under one year of HAART. 30(55.6%) and 23 (24.8%) patients from RCKH and ARTPCU center respectively had their performance capacity affected and most of them (86.8%) reported tiredness. Forgetfulness and stigma (44.4% each) and cost (1.9%) were the reasons for the dose skipped and therapy break. Conclusion: There was no significant difference in the patient satisfaction at both the centers. Services provided at both of the centers were comparatively same, except for the extra facility of comorbid treatment in RCKH and economic support, free drug distribution and consultation in ARTCU.
Keywords: Acquired immunodeficiency syndrome, Human immunodeficiency virus, People living with HIV, ART plus centre, Patient services
Full Text:
INTRODUCTION
Human Immunodeficiency Virus (HIV) that reasons Acquired Immunodeficiency Syndrome (AIDS) has become one of the world’s most alarming health-related problem. In developing countries like India AIDS have not only an impact on physical health but also have retarding impact on Social and Psychological status of patients. Social stigma will be experienced not just among the illiterates or poorly developed community however can also be found in welldeveloped and educated society. People living with HIV/ AIDS(PLWHA) may lose career, income, and even friends and family members as significant resources of assistance and support.
AIDs is hitting adults in their most economically productive years and removing the very people who could be responding to crisis. Through its impacts on the labor force, households and enterprises. One way in which HIV and AIDS affect the economic system is by decreasing the labor supply through increased death rate and illness. Among those who are able to work, productivity is likely to decline as a result of HIV-related illness. PLWHA encounter several challenges with regards to the medical management of their illness and social stigma and psychosocial issues that are associated with HIV infection. It is manifested in prejudice, discounting, discrediting and discrimination directed at people perceived to have HIV, along with the groups and communities to which they are associated.
With development of antiretroviral therapy (ART) and quality care that increases life expectancy in patients, improvement of the quality of life in PLWHA is important. Social support as an aspect of psychological adjustment can improve psychological and physical health outcomes, self-care behaviors, increasing motivation for treatment and also prevention of transmission of infection during HIV/AIDS disease. Prevention and care are now seen as interrelated. Since resources are always limited, especially in developing countries, strategies need to be developed to provide an acceptable standard of care at an affordable price. The quality and organization of medical care for HIV-infected patients in any setting inevitably reflect the functioning of the health services in general.
The epidemiologic characteristics of HIV infection vary according to geographic region and rely upon the mode of transmission, cultural factors and governmental prevention efforts and resources. The mortality rate related to HIV in Asia was estimated to be 2, 50,000 [2,10,000-2,90,000] in 2013.Most countries aspiring to expand treatment access, set themselves a goal of providing antiretroviral treatment to around 80 percent of those in need. With current global treatment coverage at 65 percent, this treatment target has not yet been met on a global scale.
Nevertheless, a number of countries have achieved or are near achieving universal access by 2015.1 In India National Aids Control Organisation (NACO) is the body responsible for formulating policy and implementing programs for the prevention and control of the HIV epidemic in India. Improved antiretroviral treatment access reduces AIDS mortality and lowers HIV incidence by reducing the viral load at the individual/community level.2
MATERIALS AND METHODS
Study was conducted in Retro clinic, Kasturba Hospital (RCKH) Manipal and ART Plus Center Udupi (ARTPCU). All HIV- infected outpatients of either sex who were on antiretroviral therapy and agreed for survey questionnaire interview were included. While HIV-infected patients with traditional or alternate medicines alone or HIV- infected patients who refused for a survey questionnaire interview were excluded from study. Total number to PLWH interviewed were 120, including 54 from RCKH and 66 ARTPCU.
The study was carried out as per the protocol approved by Institutional Review Board/Ethical Committee of each of the health facilities granted approval for the study. Based on the study criteria, the study procedures have been explained and informed consent was taken from the patients. Validated survey questionnaire was used to evaluate the support services needed for HIV positive patients at RCKH, Manipal and ARTPCU. We used both qualitative and quantitative research methodologies, including questionnaires and interviews of 120 patients receiving ART.
Demographic details, information on socio-demographic factors, psychological factors, social habits, time of diagnosis of HIV, health care system and healthcare professionalrelated factors, HAART-related factors, knowledge and belief related to HAART, and reasons for lack of adherence was documented. Although the survey questionnaire was printed in English and Kannada, the interview was conducted in English, Hindi or Kannada languages for convenience and understanding of the respondents. Agreed patients for survey questionnaire was interviewed and asked to recall and report their answers for support services needed for better HIV treatment and HIV care. Survey questionnaire consist of questions with single answer, or with multiple possible answers.
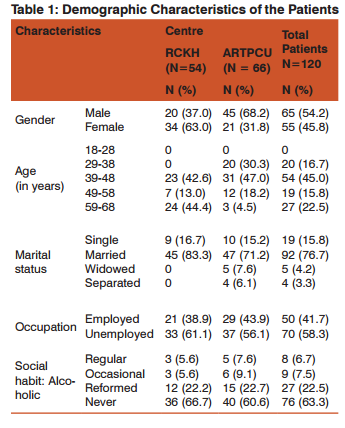
RESULT Socio-Demographic Characteristics A total of 120 HIV patients were enrolled in the study, out of which 54 were from RCKH and 66 from ARTPCU. Out of 54 RCKH patients, 20 (37%) were male and 34 (63%) were female while out of 66 patients from ARTPCU, 45 (68.2%) were male and 21 (31.8%) were female. Out of 120, majority (45%) were in the age group 39-48 years and (15.8%) were in the age group 49-58 years. Both in RCKH and ARTPCU, most of the patients were married, 83.3% (N=45) and 71.2% (N=47) respectively. Unemployed patients were more both in RCKH and ARTPCU, 61.1% (N=33) and 56.1% (N=37) respectively. From 120 patients, 110 (91.7%) were HAART experienced, which includes 50(92.6%) and 60 (90.9%)
study subject from RCKH and ARTPCU respectively. 93.4% of the total patients enrolled were literate, out of which most of the patients of RCKH had collage level education while ARTPCU had a higher number of patients with secondarylevel education. Socio-Demographic details of the patients are shown in the Table 1.
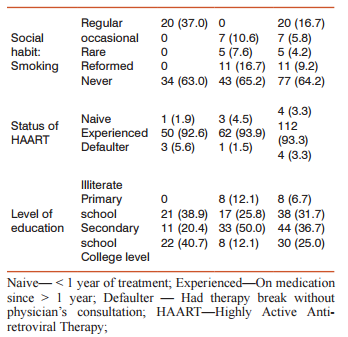
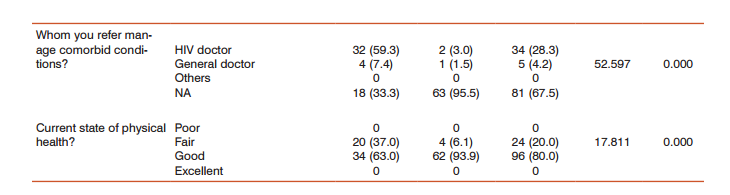
Disease And Health Related Services In disease and Health-related services out of 120 patients, 102(85.0%) got tested for HIV on Doctor’s suggestion while 18(15%) got tested by their own will. 108 patients got tested due to their illness out of which 53(98.1%) and 55(83.3%) patients were from RCKH and ARTPCU respectively. 63% of RCKH and 93.9% of ARTPCU and 37 % of RCKH and 6.1% of ARTPCU patients have good and fair physical health respectively as shown in the Table 2.
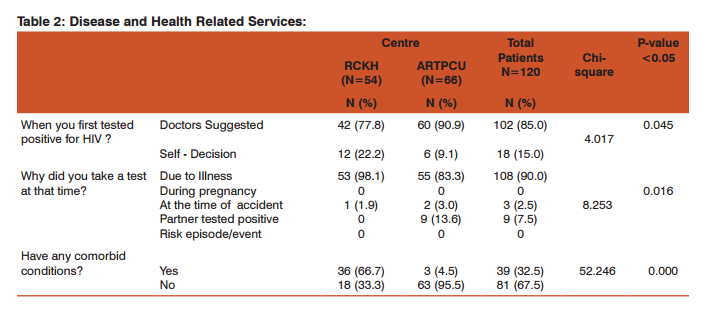
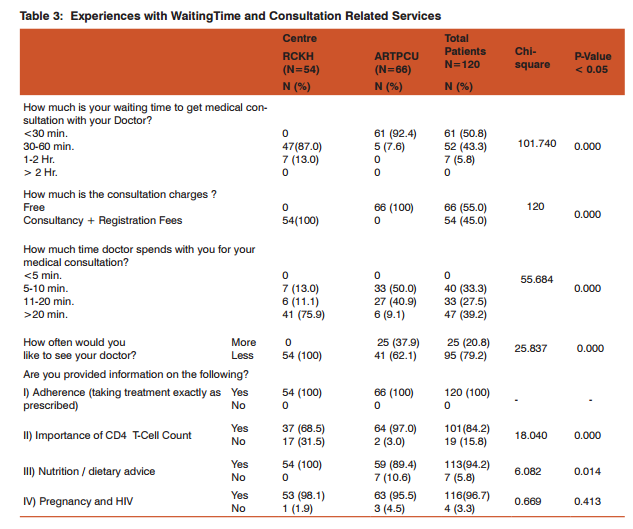
Experiences with Waiting Times and Consultation Related Services In RCKH (87.0%) waiting time was about 30-60 minutes while in ARTPCU (92.4%) it was less than 30 minutes. In ARTPCU there was no consultation charge while in RCKH patients were charged. 75.9% of RCKH patients reported consultation time more than 20 minutes while 90.9 % of ARTPCU patients reported 5- 20 minutes. Most of the patients (79.2%) did not like to make frequent visits for follow up. All the patients had privacy during discussion with doctor and Most of the patients at either of the centres received counseling (76.7%) and were satisfied (94.2%). The details are summarized in the Table 3.
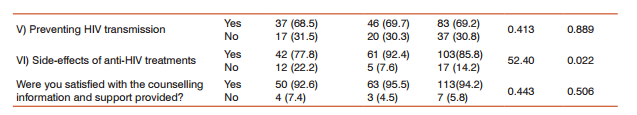
Highly Active Anti-Retroviral Therapy (HAART) Related Services Majority (56.7%) of the patients were on HAART since 1 to 5 years while only four (3.3%) were under one year of HAART. Out of 120 patients, 98.1% of RCKH and 98.5% of ARTPCU patients got their antiretroviral prescription filled for one month. 75.9% of RCKH and all from ARTPCU centre did not know either they are on monotherapy or combination therapy. 86.7% of total patients from both the centres, reported improvement in their health after starting HAART. About 17.5% of the total subjects experienced the side effects of the antiretroviral treatment and managed the same by consulting their respective HIV doctors (Table 4).
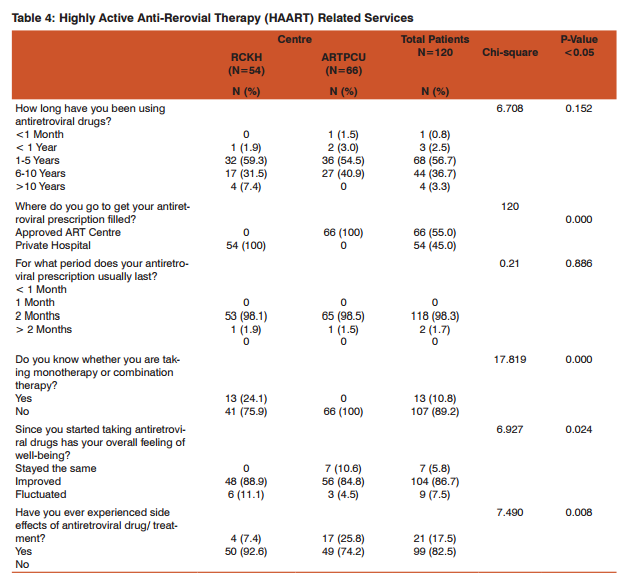
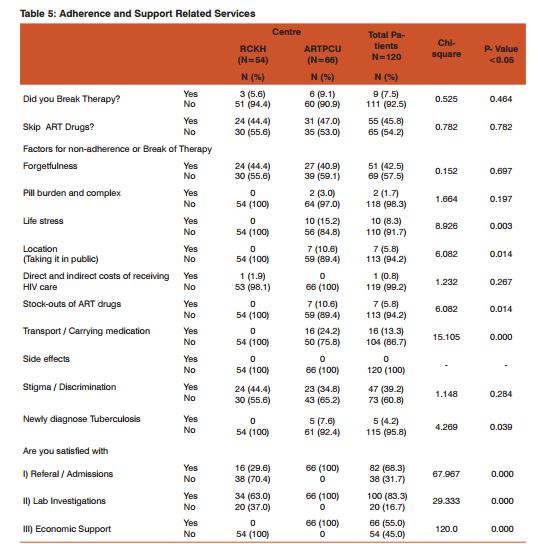
Adherence and Support Related Services Out of 54 RCKH patients, 3 had a therapy break and 24 had skipped the dose. Forgetfulness and stigma (44.4% each) and cost (1.9%) were the reasons for the dose skipped and therapy break. Out of 66 ARTPCU patients, 6 had a therapy break and 31 had skipped the dose. Forgetfulness (40.9%), was the major reason for the dose skipped and tuberculosis (7.6%) was the reason for the break of therapy. All the patients of ARTPCU were satisfied with the services like admission, lab investigation and economic support while patients from RCKH reported some un-satisfaction. Economic support was available in ARTPCU but not in RCKH.(Table 5)
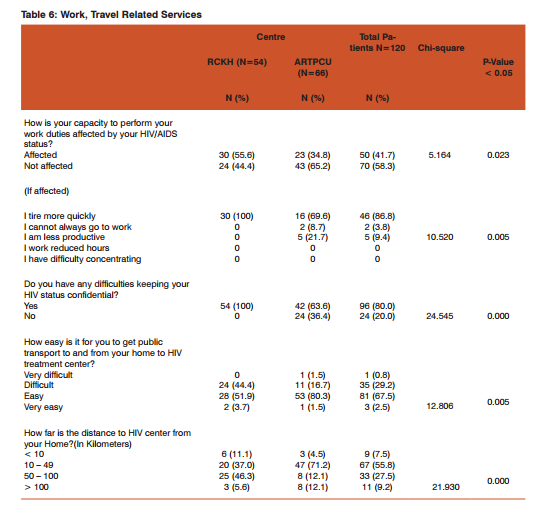
Work, Travel and Food Related Services 30(55.6%) and 23 (24.8%) patients from RCKH and ARTPCU respectively had their performance capacity affected and most of them (86.8%) reported tiredness. 80% of the total subjects participated had difficulty in keeping their HIV status confidential. Patients from both of the centres found it easy to get public transport to their HIV centres. Majority of the patients from RCKH and ARTPCU were 50-100 km and 10-49 km far from HIV centre respectively (Table 6).
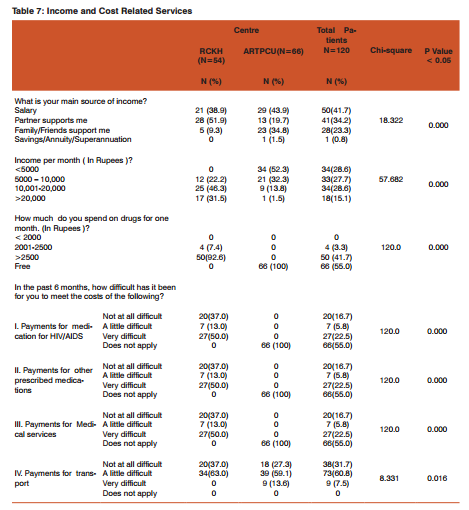
Income and Cost Related Services 21 (38.9%) and 29 (43.9%) patients from RCKH and ARTPCU respectively, had salary as their main source of income. 84.6% of ARTPCU and all patients of RCKH had income per month up to Rs.10,000 and Rs.5000-20,000 or more respectively. 50 (92.6%) of RCKH patients spent more than Rs.2500 on the drugs and patients of ARTPCU had received the free drug.(Table 7)
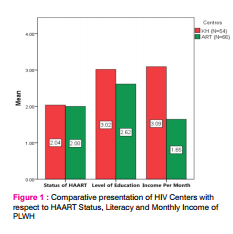
Comparative Presentation of HIV Centers Patients with higher level of education (Mean value:3.02) and higher income level (Mean value:3.09) selected RCKH to receive treatment and patient with a low income level mostly preferred to get treatment from ARTCU and HAART experienced patients were almost equally distributed in both centers as shown in Figure 1.
DISCUSSION Scaling up the access to antiretroviral treatment is not only desirable for individual patients with HIV and AIDS but also for consolidating the success of prevention and control programs in developing countries.3 Consequently expanding access to treatment has the potential to assist countries in achieving Millennium Development Goal (MDG) 6.4 This potential could be accentuated by providing quality antiretroviral treatment services in all health facilities (Government and Private Sector). The services provided to the PLWH include clinical care (treatment) and clinical support services (laboratory, pharmacy and counseling).
The choice of an HIV treatment depends on the factors such as respect to confidentiality, sensitivity toward patient needs, geographical closer, patient’s income and overall cost of the treatment. A total of 120 patients diagnosed with HIV were included in the study. In our study, RCKH showed female predominance and ARTPCU showed male predominance. Most of our patients were HAART experienced compared to naïve patients which was supported by similar study carried out by Osungbade KO. et al.3
Our experience of survey questionnaire for support services demonstrated literate patients took shorter time for giving their feedback compared to illiterate patients, the reason being illiterate patients require many explanations related to HIV disease and its management. While assessing disease and health survey questionnaire, we found that most of the patients were tested initially for HIV screening due to other illnesses as routine health check-up as per doctors’ advice. Our study results showed no significant difference at either of the centers for response regarding HIV disease, its treatment, transmission and prevention. These findings were in accordance with findings of Project Nasah, where they highlighted the importance of knowledge regarding a relationship to drug resistance and treatment failure.5
During the interview, we found that most of the HAART experienced patients reported good health condition after initiating HAART. We found that the patients of ARTPCU presented with HIV disease, mostly without comorbid conditions while RCKH patients presented with HIV disease mostly with comorbid conditions like mental disorders, cardiovascular disorders, and neurological diseases. This is because of the fact that most of the RCKH patients, preferred first to consult doctors for their comorbid conditions at Kasturba Hospital and if suspected for HIV, patients were asked for HIV screening, further confirmed for HIV positive, they would be directed to RCKH for their treatment. One of the limitation which we found for patients who were enrolled at both the centers was that they had no private insurance for PLWHA. These findings of our study, strongly support the need of health insurance.
Our findings are supported by the study done by Gupta I et al.6 Some standalone health insurance providers like Star Health and Allied Insurance offer such insurance.7,8 Related to medical consultation with a clinician, our survey revealed that in ARTCU waiting time was less than one hour but in case of RCKH, it was almost up to two hours. This may be because Kasturba Hospital is a tertiary care hospital so the doctors are involved in the ward rounds during morning hours. Privacy during discussion with doctor was maintained at either of the centers. In ARTCU doctors spent about 5 minutes to 20 minutes with patients while in case of RCKH this time varied from 10 to 20 minutes or more.
Majority of the patients did not prefer frequent visits to HIV Treatment Centre. The reason may be that HIV / AIDS has a social stigma so they prefer fewer visits to prevent the disclosure of their illness. In our study, Almost all the patient received the information regarding adherence to HAART, resistance and side effects of antiviral drug, CD4-T cell count, nutrition. Pregnancy associated information in HIV was also conveyed. This information encouraged the patients to hope for better quality of life. All the patients of ARTCU were satisfied with the other services like referral, medical checkups, lab investigations and economic support while we found some dissatisfaction for services in case of RCKH patients.
Our findings were in accordance to PLHIV satisfaction survey, Midline Assessment Report 2012 -13.9 There is no economic support for the patients of RCKH while ARTPCU patients received financial support every month at the rate of Rs.0.80 /- per kilometer for their travel fare. Only few patients opted to obtain drugs from community pharmacy. During the survey, we realized that patients did not prefer to get medication near their residency to maintain the confidentiality of their disease or sickness. Majority of the patients from either of the centers were HAART experienced (taking medication from about 1 to 10 years).
All patients got their HAART filled at the approved ART center and hospital pharmacy at ARTCU and RCKH respectively. Patients collected the drugs at a monthly basis. Few of RCKH patients were aware of the type of undergoing treatment (monotherapy / combination therapy). Majority of the patients did not experience side effects. Those who experienced side effects preferred to visit HIV doctors for their treatment. Most of the patients had no history of therapy break, but few were non adherent to the therapy. During the interview, we came to know that forgetfulness and stigma were the main reasons for the skipping of dose, while tuberculosis was the main reason for the therapy break. Study done by Fatiregun AA. et al also suggest the stigma and forgetfulness are the major reason for non-adherence to ART.10 Despite of social stigma and discrimination, patients had support from their family and friends. During the interview, a majority of (58.3%) reported that their daily duties were not affected by their illness which is supported by the report given by Blalock AC. et al which significantly showed higher incidence of overall quality of life among PLWH.11 Despite of awareness in society, still there is stigma of disease and discrimination with PLWH.
In our study, patients faced difficulties in keeping their illness confidential. Our findings were supported by the report given by Fatiregun AA. et al.10 In relation to the distance between home and HIV treatment centers(10 Km to 100 Km) most of the patients reported easy availability of public transport. Salary was the main source of income for the employed patients but the rest had economic support from their partner, family and friends. RCKH patients had good economic background while in ARTCU majority had an income maximum up to only Rs. 10,000 per month.
Patients of ARTCU got their drugs free of cost while RCKH had to pay Rs. 2000 to Rs. 2500 or more for one month treatment. Patients of RCKH reported economical difficulty in payments for medication for HIV/AIDS, other prescribed medications and Medical services while in ARTCU these were not applicable due to free availability of drugs and services. In the cross-sectional study done by Sangowawa A et al revealed that youth with HIV in Ibadan are experiencing various economic problems.12
CONCLUSION The study on the evaluation of the support services needed for patients living with HIV(PLWH) was done in RCKH and ARTCPU. In this study, overall satisfaction of patients at ARTCU and RCKH was same. Patients were aware regarding disease, its treatment and prevention at either of the centers. At ARTCU, patients got economical support as their travel fare while at RCKH patient reported economic difficulties. Patients at RCKH also got treatment for any comorbidity / other problems, but in ARTCU such as facilities were not available. Patients with higher level of education (Mean value:3.02) and higher income level (Mean value:3.09) selected RCKH to receive treatment and patient with low income level mostly preferred to get treatment from ARTCU. However, there was no significant difference in the patient satisfaction at both the centers. Services provided at both of the centers were comparatively same, except for the extra facility of comorbid treatment in RCKH and economic support, free drug distribution and consultation in ARTCU.
Competing Interests The authors declare no conflicts of interest.
ACKNOWLEDGMENTS The authors thank the staff of Department of Medicine, Kasturba Hospital, Manipal University Manipal College of pharmaceutical sciences, Manipal University for their assistance and cooperation during the study period.
References:
1. Organization WHO. Global update on HIV treatment 2013: results, impact and opportunities. 2013.; [Online] Available from: URL: www.who.int/iris/bitstream/10665/85326/1/97892415057 34_eng.pdf
2. NACO (2014) ‘Annual Report 2013-14’; [Online] Available from: URL: http://www.naco.gov.in/upload/2014%20mslns/ NACO_English%202013-14.pdf
3. Osungbade KO, Shaahu VN, Owoaje EE, Adedokun BO. Patients’ Satisfaction with Quality of Anti-Retroviral Services in Central Nigeria: Implications for Strengthening Private Health Services. Journal of Preventive Medicine. 2013;1(3):11-8.
4. United Nations Millennium Development Goals, retrieved 21 September 2013 [Online] Available from: URL: http://www. un.org/millenniumgoals/pdf/report-2013/mdg-report-2013- english.pdf
5. Project Nasah. HIV treatment information and other needs among African people with HIV resident in England. 2003.; [Online] Available from: URL: http://sigmaresearch.org.uk/ files/report2003a.pdf
6. Gupta I, Trivedi M. Willingness to pay for health insurance among HIV-positive patients in India. Appl Health Econ Health Policy. 2014 Dec;12(6):601-10 .
7. The Times of India. Coming soon: Life insurance policy for HIV/AIDS patients - The Times of India [Internet]. 2013 [cited 31 March 2015]. Available from: http://timesofindia.indiatimes. com/india/Coming-soon-Life-insurance-policy-for-HIV/AIDSpatients/articleshow/24558788.cms
8. Starhealth.in. Star NetPlus Insurance |HIV Positive Insurance | HIV Care Plan [Internet]. 2015 [cited 31 March 2015]. Available from: http://www.starhealth.in/starnetplus.php
9. PLHIV satisfaction survey, Midline Assessment Report 2012 -13 [Online] Available from: URL: http://gfatm.indiannursingcouncil.org/PLHIVsatisfactionSurvey 2013.pdf
10. Olowookere SA, Fatiregun AA, Akinyemi JO, Bamgboye AE, Osagbemi GK. Prevalence and determinants of nonadherence to highly active antiretroviral therapy among people living with HIV/AIDS in Ibadan, Nigeria. J Infect DevCtries. 2008 Oct 1;2(5):369-72.
11. Blalock AC, McDaniel JS, Farber EW. Effect of employment on quality of life and psychological functioning in patients with HIV/AIDS. Psychosomatics. 2002 Sep-Oct;43(5):400-4 .
12. Sangowawa A, Owoaje E. Experiences of discrimination among youth with HIV/AIDS in Ibadan, Nigeria. Journal of Public Health in Africa. 2012;3(1):10.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License