IJCRR - 8(2), January, 2016
Pages: 36-45
Print Article
Download XML Download PDF
EFFECTS OF AMBIENT AIR POLLUTION ON RESPIRATORY HEALTH OF CHILDREN: FINDINGS FROM A CROSS-SECTIONAL STUDY IN CHANDRAPUR, MAHARASHTRA, INDIA
Author: Uddhao Gawande, Suhas Kadam, Abhijit Khanvilkar, Gurudatt Potdar, Hrushikesh Salvitthal
Category: Healthcare
Abstract:Background: Outdoor air pollution and continuous exposure to ambient air pollutants like particulate matter are among the leading contributors to adverse respiratory health outcomes all over the world. This association between air pollution and the impairment of respiratory functions is evident from number of epidemiological studies. Health risk from particulate pollution is especially high for some risk groups such as children and elderly persons, and those with diseases of lungs. However, there are still many issues to be clarified before we know the real causal relationship between air pollution and health effects. Specific air pollutants have not been identified as causes of health effects. This specific study has been conducted with an objective to evaluate the effects of ambient air pollution on respiratory symptoms and diseases of children, in Chandrapur district of Maharashtra state in India. Methods: Comparative cross-sectional quantitative study was undertaken in the Chandrapur district with two geographical locations \? study and control between August-November 2013. The data included primary data collection from school children to assess the lung function among children, flow meters were used and readings were recorded.2000 school children were selected in this study. Epidemiological information was collected from them by administering structured tool (2000) and Peak Expiratory Flow Rate was measured through use of Flow Meter (2000).Data was analysed using frequency tables, crosstab analysis and chi-square test to show significance. Results: Statistically significant difference is observed in prevalence of dry cough, night cough and sneezing symptoms between study and control groups. Statistically significant difference is observed in prevalence of dry cough, night cough and sneezing between less than or equal to 5 km (5 km) distance from the industry. Within study group rhinitis showed statistically significant difference for distance less than 5Km and more than 5Km between home and industry by chi square test. Conclusion: There is a significant effect of ambient air pollution on respiratory symptoms of school-aged students with high prevalence of the symptoms in the study area which is the industrial area than the control area. Presence of multiple industries in or near the village is more harmful than the single industry. Additionally, it also shows that the presence of steel, cement and paper industry in or near a village has caused more ill-effects as compared to coal and thermal industry.
Keywords: Air pollution, Respiratory health, Disease, School children, Chandrapur, Maharashtra, India
Full Text:
INTRODUCTION
Ambient air pollution is one of the leading contributors to adverse respiratory health outcomes in industrial areas all over world and children are more susceptible to this pollution than the adults. The special vulnerability of children to air pollution exposure is related to several differences between children and the adults. The children are highly sensitive to the adverse effects of air pollution due to their rapidly growing lungs, incomplete immune and metabolic functions, patterns of ventilation and high levels of outdoor activity. (1) A large body of evidence from the Children’s Health Study (CHS) has documented that exposures to both regional ambient air and traffic-related pollutants are associated with increased asthma prevalence, new-onset asthma, risk of bronchitis and wheezing, deficits of lung function growth, and airway inflammation. The high levels of air pollution bring many challenges to public health.
To further ameliorate adverse health effects attributable to air pollution, many more toxic pollutants may require regulation and control of industrial emission sources may need to be strengthened. Individual interventions based on personal susceptibility may be needed to protect children’s health while control measures are being implemented. (2)Health risk from particulate pollution is especially high for some susceptible groups such as the children and the elderly persons, and those with diseases of the heart and lungs. (3) The study area, Chandrapur is a district in the north-eastern part of Maharashtra has large natural deposits of coal, limestone, high grade iron-ore, bauxite and chromite which have triggered the growth of industries in the district by the Maharashtra Industrial Developmental Corporation (MIDC).
There has been a tremendous growth in the number of coal, cement and steel industries in Chandrapur over the years which have contributed to the growing economy of the district and the state.(4,5)There are a total of 6000 small and big scale industries in Chandrapur. Chandrapur city is also called as City of Black Gold because of the large number of coal industries in and around the city. There are a total of 35 coal mines (out of which 7 are in the city), mostly open cast in the city and surrounding areas, over half a dozen coal washeries, one large paper mill, sponge iron units and several cement industries. The Chandrapur Super Thermal Power Station (CSTPS) is one of the biggest thermal power stations in Asia, which is currently generating 2340 MW of electricity.(6) Industrialization of such a scale has been responsible for very high levels of ambient air pollution in Chandrapur District.
According to the Ministry of Environment and Forests (MoEF), Chandrapur is the most polluted city in Maharashtra and the 4th most polluted industrial cluster in India among the 88 key industrial clusters.(7) In terms of Respirable Suspended Particulate Matter (RSPM) pollution, Chandrapur is the most polluted city in India. The ambient levels of SO2 in Chandrapur are the third highest in India, and the National Aeronautics and Space Administration (NASA) has already warned of acid rains in Chandrapur in the future.(8)Apart from its harmful effects on vegetation and water quality, high levels of air pollutants emitted from the industries have a significant effect on human health, not only among people working in these industries but also among people living in the vicinity of these industries.(9)High levels of PM10, SO2 and NOx have been associated with adverse respiratory health particularly those associated with airways diseases such as COPD and asthma, and cardiovascular health such as ischemic heart disease, hypertension, systemic inflammation and diabetes mellitus (DM).(10)
According to the Central Pollution Control Board (CPCB), levels of air pollution in Chandrapur district are in the critical zone raising serious concerns of adverse effects on human health. Several questions raised by Honourable Members of the Maharashtra Legislative Assembly during the legislative assembly meetings regarding concerns of worsening health of people living in Chandrapur due to industrial air pollution need to be addressed so that appropriate intervention strategies can be adopted and implemented in the future. Therefore, government decided to do a cross-sectional study to assess the health effects of ambient air pollution on the local residents of Chandrapur.
This study was commissioned by State Health Systems Resource Centre (SHSRC), Pune jointly with Prognosis Management and Research Consultants, Pune. This study tried to give the current health status children regards respiratory and cardio-vascular system. It also has compared it between the industrial and non-industrial areas of Chandrapur district. Further the results are compared with results of neighbouring district (Nagpur) and India as well.
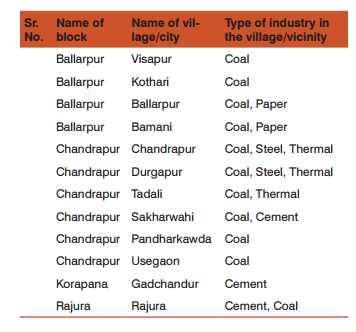
Objectives: This study of assessing health effects was focussed with following objectives – • To determine the effects of ambient air pollutants on respiratory health of children in Chandrapur • To determine prevalence of respiratory symptoms and diseases (Asthma, LRTI/ Pneumonia etc.) among children studying in schools in Chandrapur Study Design / Methodology: Comparative cross-sectional quantitative study was undertaken in the district with two geographical locations – study and control between August-November 2013. The study is jointly done by State Health Systems Resource Centre, (SHSRC) Pune and Prognosis Management and Research Consultants, Pune in the select blocks of the Chandrapur District (Ballarpur, Chandrapur, Korapana and Rajura). Study location was in the vicinity of industry and control location was more than 25 km from any of the industries. Quantitative data included primary data collection from school children to assess the lung function among children, flow meters were used and readings were recorded. The laboratory of the district hospital was used for testing. The informed consent was given by the parents through principal of the school.
Sampling: Five private and five government schools were randomly selected from study area and same number from control area. From each school, fifty students each of standard 2 and standard 8 were randomly selected. Simple random sampling was used to select the blocks, locations and schools from the study locations. Industrial (study) and non-industrial (control) areas were selected as explained: One Factory each from power plant, coal mines, cement, paper and steel industry was first identified on the basis of maximal population density within radius of 40 km from the factory in Chandrapur district. The selected regions were then subdivided into radius of 1-5 km, 5-10 km, 10-20 km, 20-30 km, 30-40 km and >40 km =was included in non-industrial area. Based on this criterion, the sample was divided in eleven villages in study area and three villages in control area. Also, these locations were confirmed on consultation with local health functionaries during meeting held before commencement of field work in Chandrapur. The summary below provides at a glance industrial blocks (areas) and village wise distribution of industries:
Huge amount of dust or particulate matter is generated in cleaning and milling sections in a rice mill.(13)However there is no mechanism to measure the amount of emitted particulate matter. Additionally the MPCB pollution monitoring site is not established at Mul block. Therefore effect of the air pollution caused due to rice mills on the health of people in this block cannot be measured. Sample Size: The sample size was determined for school children upon considering lowest prevalence of respiratory disease. Asthma being the lowest prevalent respiratory disease its respective prevalence value for children was taken as ‘P’ in sample size calculation. This also meant coverage of larger population and other diseases. Sample for children: Prevalence of asthma for this age group is 4.5% as per the ISAAC study. This is taken as p in the sample size formula.



Interviews and diagnostics of target population: We have selected 2000 school children. Epidemiological information was collected from them by administering structured tool (2000) and Peak Expiratory Flow Rate was measured through use of Flow Meter (2000). Human Resources: Appropriate human resources were deployed for implementing the study. These included public health specialists, clinical specialists, air pollution specialist, social scientists, and auxiliary nurse midwives.
Data collection Training of all the data collectors was conducted prior to commencement of data collection. Data was collected in the following manner: School children’s epidemiological data- A structured questionnaire was filled by a group of social scientists, by asking questions to students. Students were asked questions regarding their demographic details, clinical manifestations that is number of illness episodes in last one year, presence of illness at the time of study and presence of respiratory illness. Height and weight of students was measured.
Teachers’ help was taken for the questions such as attendance or performance of child. School children’s diagnostics- Flowmetries were conducted usingRMS Helios flowmeters by social scientists. Each child was given instructions on how to perform the flowmetry before the test. The test was carried out in standing position. Every child was asked to perform the test five times and the best reading was recorded. Data Entry and Analysis: Collected data was entered using epi-info software and then was exported to SPSS for statistical analysis. Appropriate statistical tools and tests were used to compare the results. The analysis included descriptive statistics, inferential statistics and application of Test of Significance.
RESULTS Finding of school children epidemiological data: School children in the age group 6-7 years and 13-14 years were selected with the purpose of observing effects of ambient air pollution at different age groups.
Clinical manifestation: Following tables present clinical manifestations amongst school children from study and control areas and also the association of clinical manifestations amongst school children from study with respect to distance of their home from nearest industry.
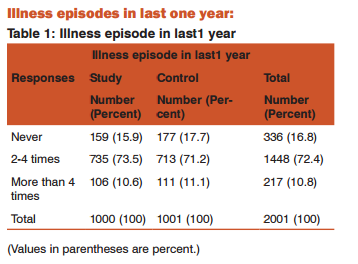
Table 1 shows that, more than 70% of children from both, study and control sites had an episode of illness 2-4 times in last 1 year. Also, more than 10% of children from both sites have more than 4 episodes of illness in last 1 year. Wheeze, productive cough, night cough and breathlessness are the indicative symptoms for asthma and COPD. Hence, these symptoms were asked along with other respiratory symptoms such as dry cough, sore throat etc. Following table 2 presents the presence of respiratory symptoms in study and control area as well as with respect to distance of home from nearest industry.
Presence of respiratory symptoms: Table 2 shows that, close to 30% of children had dry cough in study area, the percentage of which in control area was 21.3% Equal proportion (7.8%) of children in study and control area experienced productive cough in last 1 year. More than 22% of children in study area had night cough in last 1 year, as compared to 13.6 % children in control area more children in study area (17.8%) experienced continuous sneezing as compared to the children in control area (10.2%). More children in study area (6.8%) had sore throat as compared to the children in control area (3.3%).
More children in study area (6.1%) had presence of wheeze as compared to the children in control area (4.4%). More children in study area (6.7%) had chest pain as compared to the children in control area (3.3%)... More children in study area (3.2%) experienced breathlessness as compared to the children in control area (1.7%). More children in study area(2%) had asthma as compared to the children in control area(1.2%). Barring a couple of cases in control areas tuberculosis was not evident. Pneumonia was very low. Only one student in study area had pneumonia in last year. More than 30% of students residing less than 5 kms from the industry experienced dry cough as compared to students
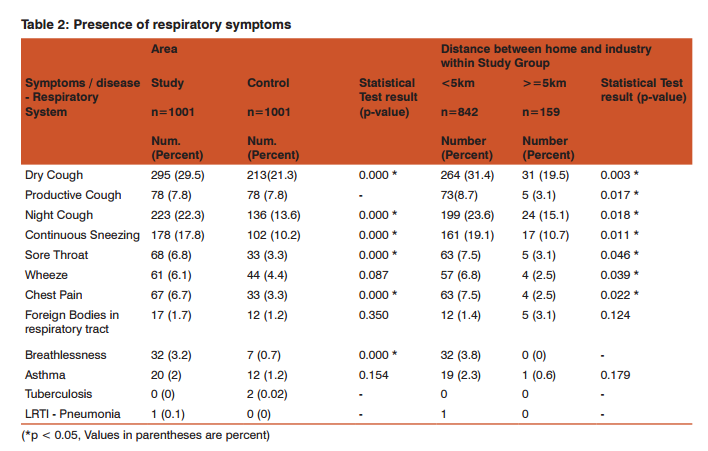
staying at a distance of more than 5 kms from an industry (19.5%). Amongst the students who experienced productive cough higher percentage (8.7%) were staying at less than 5 kms distance from nearest industry. More number of students were staying at less than 5 kms distance from nearest industry experienced night cough (23.6%) as compared to those students staying at a distance of more than 5 kms from industry (15.1%). Amongst the students who had continuous sneezing, more (19.7%) were staying at less than 5 kms distance from nearest industry. Amongst the students who experienced wheeze, maximum (6.8%) were staying at less than 5 kms distance from nearest industry. Amongst the students who had chest pain, higher proportion(7.5%) of these students were staying at less than 5 kms distance from nearest industry. Amongst the students who experienced sore throat maximum (7.5%) were staying at less than 5 kms distance from nearest industry.. , all the students who experienced breathlessness were staying at less than 5 kms distance from nearest industry. Amongst the students who had asthma, maximum were staying at less than 5 kms distance from nearest industry.
Statistically significant difference is observed in prevalence of following symptoms between study and control groups: • Dry Cough: 29.5% in Study and 21.3% in Control, p=0.000 Significant by Chi Square test • Night Cough: 22.3% in Study and 13.6% in Control, p=0.000 Significant by Chi Square test • Sneezing: 17.8% in Study and 10.2% in Control, p=0.000 Significant by Chi Square test Statistically significant difference is observed in prevalence of following symptoms between 5km distance • Dry Cough: 31.4% in 5 km, p=0.003 Significant by Chi Square test • Night Cough: 23.6% in 5 km, p=0.018 Significant by Chi Square test • Sneezing: 19.1% in 5 km, p=0.011 Significant by Chi Square test .
Village wise prevalence of symptoms The respiratory symptoms reported by school children in the study area were also assessed with respect to presence of industry in or near village.

From table 3, it can be seen that the prevalence of respiratory symptoms is higher in villages with multiple industries as compared to the villages with single industry. However in case of village having cement industry, the prevalence is higher irrespective of number of industries present in or near the village.
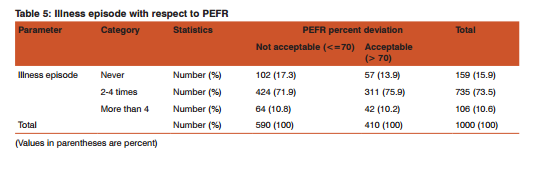
Finding of school children diagnostic test: Peak Expiratory flow rate(PEFR) was assessed with the help of flow meter in all school children in study and control area. (14) The percentage deviation of the recorded PEFR from expected PEFR was analysed with respect to study and control area. Table 4 present PEFR results amongst school children from study and control areas.
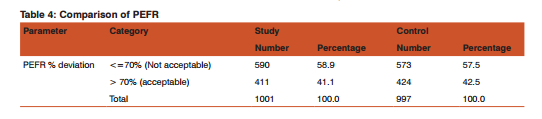
About 58.9 % students from study area had not acceptable PEFR% whereas 57.5% students from control area had not acceptable PEFR%. There is no significant difference observed in PEFR% result between Study and Control group (p-value by Chi-square= 0.130). This implies the lung function of children in these two areas is comparable.
PEFR results amongst school children from study area: Table 5 shows that, more than 80% students from study area having not acceptable PEFR% had more illness episodes.
alone and that the effects of air pollution on health needed to be ascertained further. In July 2001, the Bharatiya Adimjati Sevak Sangh along with the Collectors office in Chandrapur conducted a health survey of 3000 people from 5 study villages (villages in the vicinity of industries) and 2 control villages in Chandrapur(villages away from the industries). This study which was funded by the coal mine company (Western Coal Fields Limited) and executed by GMC Chandrapur and GMC Nagpur reported no significant variation between control and target population.(21)
CONCLUSION Exposure to a mixture of air pollutants associated with adverse respiratory health of the children living in the industrial areas of the district. Clinical manifestations: Presence of multiple industries in or near the village is more harmful than the single industry. Additionally, it also shows that the presence of steel, cement and paper industry in or near a village has caused more illeffects as compared to coal and thermal industry. School children: Statistically significant difference is observed in prevalence of following symptoms between study and control groups: • Dry Cough: 29.5% in Study and 21.3% in Control, p=0.000 Significant by Chi Square test • Night Cough: 22.3% in Study and 13.6% in Control, p=0.000 Significant by Chi Square test • Sneezing: 17.8% in Study and 10.2% in Control, p=0.000 Significant by Chi Square test Statistically significant difference is observed in prevalence of following symptoms between 5km distance • Dry Cough: 31.4% in 5 km, p=0.003 Significant by Chi Square test • Night Cough: 23.6% in 5 km, p=0.018 Significant by Chi Square test • Sneezing: 19.1% in 5 km, p=0.011 Significant by Chi Square test Within study group, following symptoms showed statistically significant difference for distance less than 5Km and more than 5Km between home and industry. • Rhinitis: 30.2% in less than 5Km and 13.4% in more than 5Km, p=0.004 Significant by Chi Square test.
Recommendations
1. Students under this study should be taken as cohort and periodically monitored over next 3 years to observe and record any deterioration in health and associated illness and performance at school
2. Strengthening of source emission monitoring is necessary.
3. Strengthening of air quality monitoring network- Levels of PM2.5, CO and CO2 gases should also be recorded along with the presently monitored SO2, NOx and RSPM as these gases are also equally harmful to health.
4. Proper mechanism for enforcement and compliance of regulations related to pollution should be built.
5. Bypass road should be built for truck transport, and also the transport of industrial products should be done in closed trucks.
6. Sentinel Surveillance Centres should be established by Public Health Department wherein, the equipment’s like Spirometer and Flow-meter used for the current study should be part of these Sentinel Centres. The Centres will act as Centres of Excellence. The role of these Sentinel Centres is proposed below.
Sentinel Surveillance Centres The foremost need of the hour is to establish Sentinel Surveillance Centres at the public health facilities where the MPCB monitoring sites are located i.e. Chandrapur SRO, Chandrapur MIDC, Tadali MIDC, Ghuggus, Ballarshahand Rajura. Thus, Centres should be established at following facilities- 1.General Hospital, Chandrapur, 2.Primary Health Centre, Durgapur, 3. Primary Health Centre, Tadali, 4. Primary Health Centre, Ghuggus, 5. Rural Hospital, Ballarshah and 6. Rural Hospital, Rajura. These Centresshall work as “Centre of Excellence” in the district. These Centres should impart promotive, preventive and curative services.
1. Target population: Population in the catchment area of 6 health facilities should be the target population. Cases identified in the study for respiratory symptom and diseases and cardio-vascular symptoms and diseases should be treated and followed up in these centres.
2. Local NGOs: Local NGOs should be involved in the activity and their help/ support should be taken for following up the cases.
3. Awareness creation and prevention measures: This centre should bring all 5 stakeholders together; namely: Public Health Department, MPCB, NGOs, Industries and Community. Every stakeholder will be enrolled in awareness activities. Community will be made aware about early signs of these symptoms and will be encouraged to take treatment on time.
4. Clinical Role: These Centres should provide treatment to all the cases that come with respiratory symptoms and diseases. I.e. dry cough, night cough, productive cough, sore throat, wheeze, sneezing like symptoms should be treated and monitored as they are precursors to the respiratory diseases Asthma and COPD. Similar, Cardiovascular symptoms and diseases will be treated and monitored here. I.e. hypertension, chest pain will
be treated and monitored as they are precursors to the cardiovascular diseases. Other diseases or symptoms which should be monitored are ophthalmic problems (redness of eyes, eye infections) and skin problems (itching, eczema). Regular supply of medicines for all these symptoms and diseases should be ensured. These centres should also maintain case-wise record of all these diseases and should make its use for planning and further improving health status. Moreover, these Centres should function as observation and monitoring mechanism for the health outcome of the people residing in the vicinity of industries with respect to changes in air pollution levels.
Although the association with known air pollutants is suggestive, a cross-sectional study cannot confirm a causal relationship and further studies are needed to determine the exposure-effect relationship between individualized air pollution exposure and various adverse respiratory effects. The sample from the current study should be taken as cohort for continued observation and monitoring; along with the cases of possible ill-effects of air pollution detected in all health facilities, including government hospitals and industry-run hospitals in the vicinity of industrial areas. Regular health check-up of these cases should be done in conjunction with pulmonary function tests, ECGs and blood tests if required.
Specific functions should include:
1. Capacity building of Doctors and paramedics • For detection of illnesses/diseases due to air pollution. For monitoring and reporting certain parameters and illnesses related to air pollution, For preventive measures to be taken by the people for these effects Process of reporting cases showing effects of air pollution
2. Follow up of participants in the study, showing unfavourable health effects of air pollution as well as cases reported by the health facilities in the nearby areas
3. Periodic check-up and investigations of this cohort for the effects of air pollution
4. Advice promotive and preventive measures through awareness such as use of cloth around mouth and nose, nutrition and hygiene, conversion of coal-chulhas to non-coal chulhas to patients showing pre-disease condition or minimal effects
Source of Funding: Please mention source of funding for this work (if any) – nil
Conflict of interest: Please declare conflict of interest (if any) – nil
ACKNOWLEDGEMENT
Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors / editors / publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
1. Gilliland FD, McConnell R, Peters J, Gong H. A theoretical basis for investigating ambient air pollution and children’s respiratory health. Environ Health Perspect [Internet]. 1999 Jun 1;107(Suppl 3):403-7. Available from: http://www.ehponline. org/ambra-doi-resolver/10.1289/ehp.99107s3403
2. Chen Z, Salam MT, Eckel SP, Breton C V, Gilliland FD. Chronic effects of air pollution on respiratory health in Southern California children: findings from the Southern California Children’s Health Study. J Thorac Dis. 2015;7(1):46-58.
3. Ulrich MMW, Alink GM, Kumarathasan P, Vincent R, Boere a JF, Cassee FR. Health effects and time course of particulate matter on the cardiopulmonary system in rats with lung inflammation. J Toxicol Environ Health A. 2002 Oct 12;65(20):1571-95.
4. Ministry of Micro S and ME. Brief Industrial Profile of Chandrapur District.
5. Western Coalfields Limited. An overview of industries in the state of Maharashtra.
6. Maharashtra Pollution Control Board. Environmental Status and Action Plan for Control of Pollution at Chandrapur [Internet]. Available from: http://mpcb.gov.in/images/pdf/action plan chandrapur1.pdf
7. The Times of India. Chanda fourth most polluted city in India. :1-2. Available from: http://timesofindia.indiatimes.com/city/nagpur/Chanda-fourth-most-polluted-city-in-India/articleshow/5392934.cmsreferral=PM
8. Central Pollution Control Board. Comprehensive Environmental Assessment of Industrial Clusters [Internet]. Central Pollution Control Board, Ministry of Environment and Forests; 2009. 1-28 p. Available from: http://cpcb.nic.in/divisionsofheadoffice/ess/NewItem_152_Final-Book_2.pdf
9. Maharashtra Pollution Control Board. CEPI Report. 2010.
10. Natural Resources Defense Council. Our children at risk. 1998;(June 1993):1-13.
11. Sharma AK, Siddiqui KA. Assessment of Air Quality for an Open Cast Coal Mining Area. Indian J Sci Res. 2010;1(2):47- 55.
12. Atimtay A, Chaudhary T. Air Pollution Due to Nox Emissions in an Iron-Steel Industry Region in South-Eastern Turkey and Emission Reduction Strategies. Middle East Tech Univ Environ Eng Dep 06531 Ankara [Internet]. Available from: http://www. umad.de/infos/cleanair13/pdf/full_152.pdf
13. Central Pollution Control Board. Comprehensive Industry Document on Pulse, Wheat, Rice Mills. 2008; (July):108. Available from: http://cpcb.nic.in/upload/NewItems/NewItem_132_ coind-pulsewheatricemills.pdf
14. Chowgule R V, Shetye VM, Parmar JR. Lung function tests in normal Indian children. Indian Pediatr. 1995; 32(2):185-91.
15. Jindal SK, Aggarwal AN, Gupta D, Agarwal R, Kumar R, Kaur T, et al. Indian Study on Epidemiology of Asthma, Respiratory Symptoms and Chronic Bronchitis in adults (INSEARCH). Int JTuberc Lung Dis [Internet]. 2012 Sep 1;16(9):1270-7. Available from: http://icmr.nic.in/final/INSEARCH_Full_Report.pdf
16. World Health Organization. Ambient (outdoor) air quality and health. 2014; 313:7. Available from: http://www.who.int/mediacentre/factsheets/fs313/en/#
18. Radomski A, Jurasz P, Alonso-Escolano D, Drews M, Morandi M, Malinski T, et al. Nanoparticle-induced platelet aggregation and vascular thrombosis. Br J Pharmacol [Internet]. 2005 Nov; 146(6):882-93. Available from: http://doi.wiley. Com/10.1038/sj.bjp.0706386
19. Seaton a, MacNee W, Donaldson K, Godden D. Particulate air pollution and acute health effects. Lancet [Internet]. 1995 Jan; 345(8943):176-8. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0140673695901736
20. Nemmar A, Hoylaerts MF, Hoet PHM, Nemery B. Possible mechanisms of the cardiovascular effects of inhaled particles: Systemic translocation and prothrombotic effects. Toxicology Letters [Internet]. 2004. p. 243-53. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0378427403005034
21. Government of India. State of Environment Report [Internet]. 2009. Available from: http://www.moef.nic.in/downloads/home/home-SoE-Report-2009.pdf
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License