IJCRR - 13(5), March, 2021
Pages: 132-140
Date of Publication: 03-Mar-2021
Print Article
Download XML Download PDF
The Effect of Superimposed Effect of Proprioceptive Sensory Stimulation Taping (Elastic Taping) and PNF on Function Improvement and Stiffness Reduction in Neurological Injury
Author: Jung-Ho Lee, Yong-Jin Jeon
Category: Healthcare
Abstract:Introduction: Stroke and subsequent neurological damage negatively impacts patients and their families. Most prominent manifestation of stroke if loss of sensory and motor capacities of patients. Objective: This study aims to determine the effect of elastic taping applied to the upper extremities before applying the proprioceptive neuromuscular facilitation (PNF) upper extremity pattern on the rehabilitation of upper extremity functions of stroke patients. Methods: The study groups (n=28) were divided using the random selection method into an experimental group consisting of 14 patients who applied taping before the treatment of PNF upper extremity pattern and a control group consisting of 14 patients who did not apply taping before the treatment of PNF upper extremity pattern. The PNF pattern used upper extremity D2 flexion, D1 flexion, D2 extension, D1 extension, and chopping patterns, and the elastic taping on the upper extremities, all of which were applied to the deltoid, supraspinatus, infraspinatus, pectoralis major, triceps brachii, and wrist extensor. To evaluate the improvement of the upper extremity functions after the intervention, the Korean Version of Modified Barthel Index (K-MBI), the Korean version of Fugl-Meyer assessment, and the Action Research Arm Test were used. Results: The study analysis results showed that there was a significant difference in the assessment results within groups as well as between groups. Conclusion: The PNF and elastic taping treatment applied to patients with stroke have positively improved the upper extremity functions due to the synergistic effect between two interventions.
Keywords: Rehabilitation, Nervous System, PNF, Taping, Function
Full Text:
INTRODUCTION
A stroke is a disease that is accompanied by various symptoms as a result of the loss of cerebral functions caused by cerebrovascular ischemia or bleeding.1 A stroke can incur various disabilities depending on the damage location and intensity in the brain. Most stroke patients experience degradation in maintaining posture, functional movements, sense of balance, and gait ability due to asymmetric body alignment. Neurological damage occurs after a stroke, which negatively impacts not only patients themselves but also patients’ families and society due to the aftereffects or complications. A stroke is a disease that should be urgently treated as a medical and social problem, as clinical symptoms of stroke, such as motor disturbance, sensory disturbance, decreased consciousness, dysphasia, and cognitive impairment can be found.2
In particular, patients with stroke have a functional disability performing the independent activities of daily living, due to motor control impairments caused by muscle strength weakening, abnormal muscle tone and abnormal movement patterns.3 This impairment is followed by the limitation of functional performance levels for activities such as walking, climbing stairs, and self-caring. Stroke leads to proprioceptive sensory impairments, and its lesion in the upper motor neuron degrades the body’s ability to balance, which worsens over time as stiffness occurs.4 Proprioception plays an important role in neuron-motor control and proprioceptors, which intervene in proprioception and are distributed in the muscles, joints, ligaments, tendons, and skin. It is divided into muscle receptors that are sensitive to mechanical stimuli, joint receptors, and skin receptors. Proprioception is information received from these three receptors. To explain this functionally, proprioception is information received at an unconscious level rather than a conscious level and is defined as the perception of posture, movements, or balance change concerning the body, as well as weight and resistance against specific objects.5
Most stroke patients experience functional motor disturbance in the upper extremities, and this disturbance lasts for a long period. In particular, if the control of voluntary muscles is lost due to motor disturbance, an imbalance between flexors and extensors occurs.6 As a result, stroke patients cannot sustain the weight of their upper extremities due to muscle paralysis in the shoulder, limiting the joint range of motion as well as incurring shoulder subluxation and rigidity, resulting in the severe reduction in upper extremity functions. The problems in the upper extremities occurring in stroke patients have a significant impact on the independent activities of daily living due to the reduction in control ability of the upper extremities as a result of rigidity and muscle strength weakening.7
The degradation in upper extremity functions varies depending on the region of the brain that was damaged, which requires constant management due to the disabilities caused by the damage. Thus, the important part of the rehabilitation in the upper extremities of stroke patients aims to improve the quality of life by increasing the remaining functions through the minimization of the disabilities. The motor disturbance in the upper extremities due to stroke is one of the most general aftereffects and has a significant impact on the performance of daily living activities.8 Despite intensive and various therapeutic approaches, the recovery of upper extremity functions of stroke patients is limited. Generally, the recovery of paralysis in the upper extremities is not better than that in the lower extremities because movements in the upper extremities in the affected side are difficult due to the contracture and non-use of the paralyzed extremities, muscle strength weakening, dysaesthesia, and the frequency of their use gradually decreasing.9,10
Besides, damage to proprioception occurs in stroke patients, and this damage delays the recovery of motor functions. Moreover, if the damage to proprioception continues in patients who achieve appropriate muscle strength recovery after stroke, performing daily living activities would be difficult for them.11 Proprioception is the unconscious information regarding the position and movement of the skin, muscles, tendons, and joints, which is regarded as the physical ability to deliver the body a sense of position and interpret information. Proprioception is utilized as the basic information of balance and paresthesia, and maintains the correct posture through the feedback and feedforward mechanism and achieves the proper body movements. If the damage to proprioception continues, patients will excessively depend on visual information during daily activities, which further delays the recovery of proprioception. Thus, it is important to evaluate and train proprioception correctly in the rehabilitation process of stroke patients.12
Proprioceptors that contribute to proprioception in the muscles and tendons react sensitively to the muscle length and muscle tone via muscle spindles and tendon organs of the Golgi body, thereby playing an important role in recognizing the movement and position of joints.13 Proprioceptors distributed in the joints are mostly found in articular capsules and ligaments. They react in the entire range of joint movements and provide proprioceptive sensory information that helps correct and control joint movements.14
To have normal daily activities and improvements on the quality of life of hemiplegic patients due to stroke, efforts are needed to recover the performance of daily activities, muscle activities, upper extremity functions, and gait ability to the level before the outbreak of stroke through the recovery of physiological functions in the upper and lower extremities in the affected side, alleviation of weight-bearing asymmetry, and improvement of postural stability.15 For hemiplegic patients, exercises to develop the central nervous system (CNS), such as proprioceptive neuromuscular facilitation (PNF), have been applied for general functional recovery.16,17
Although methods to increase the functional activities of the upper extremities and trunk strengthening exercises through PNF upper extremity patterns have been widely employed in clinical fields, few studies have been conducted on the effect of taping with a positive impact on the increase of muscle strength and muscle re-education before applying the PNF pattern about the upper extremities.18-21 Thus, this study aims to determine the effect of elastic taping applied to the upper extremities before PNF upper extremity pattern treatment on the rehabilitation of upper extremity functions of stroke patients, thereby providing foundational data to improve the activities of daily living in stroke patients.
MATERIALS AND METHODS
Subjects
This study selected 28 stroke patients who were treated in the hospital. The subjects who participated in this study were fully informed of the purpose of the study and the methods and gave their written consent to voluntarily participate. The study groups were divided using the random selection method into an experimental group consisting of 14 patients who applied taping before the treatment of PNF upper extremity pattern, and a control group consisting of 14 patients who did not apply to tape before the treatment of PNF upper extremity pattern. The subjects voluntarily participated in the study after being fully informed of its purpose and contents, experimental procedures, and stability. They also submitted written participation consent before the experiment. All experimental procedures were performed following the Declaration of Helsinki.
The selection criteria of the study subjects were hemiplegic patients who were diagnosed with stroke six months to two years ago, patients who had more than 24 points in the Korean version of the Mini-Mental State Examination (MMSE-K), patients without congenital deformity, patients without respiratory functional problems due to respiratory and cardiovascular diseases, patients without orthopaedic problems that may affect the study, and patients who could follow the instructions of the researcher. This study excluded patients who were participating in regular exercises or other exercise programs, patients with cerebellar diseases, patients with other diseases that may affect the upper extremity activities, and patients who were taking medicine to reduce spasticity.
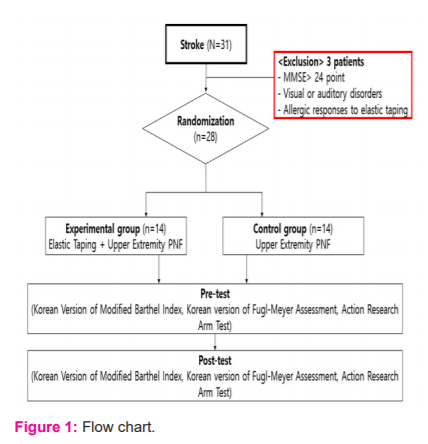
Both the experimental and control groups in this study took the treatment using the PNF upper extremity patterns during the neurodevelopmental treatment. For the experimental group, elastic taping was applied to the upper extremities before the PNF treatment. The control group was treated using the PNF upper extremity patterns without applying taping to the upper extremities for 30 min. For the assessment in this study, prior assessments were conducted before the therapeutic intervention, and then post-assessments were conducted after the last treatment. All groups had a total of 20 therapeutic interventions, five times a week for four weeks as shown in Figure 1.
Treatments
Elastic Taping
To apply the taping therapy to the upper extremities, taping for shoulder stability and taping for suppression of flexor muscles in the upper extremities were used. The elastic taping for shoulder stability was applied to the deltoid, supraspinatus, infraspinatus, and pectoralis major, and the taping for suppression of the flexor in the upper extremities was applied to the triceps brachii and wrist extensor.
For the anterior part of the deltoid, the elastic tape was applied from the tuberosity of the humerus up to the coracoid process while extending the upper extremity to the back and slightly abducting. For the posterior part of the deltoid, taping was applied to the distal 1/3 of the spine of the scapula while placing the patients’ hand at the shoulder of the opposite side. The supraspinatus taping was attached in the direction of the greater tuberosity of the humerus on the affected side to the supraspinous fossa in the scapula. The upper part of the infraspinatus taping was taped from the medial bottom of the spine of the scapula, and the lower part was taped from the angulus inferior scapulae and attached to the upper lateral part of the humerus while having the patients’ handhold the scapular region on the opposite side; thereby lifting the scapular region on the side of the tape.
The pectoralis major was taped from the 1/3 of the anterior humerus, which was separated from the deltoid while maintaining the external rotation and extension of the shoulder joint a little, and both the horizontal abduction in the shoulder joint and elbow joint were bent at 90°. The upper tape was attached to the sternoclavicular joint, and the lower tape was attached to the side of the papilla and wrapped around the sternal area of the pectoralis major. The triceps brachii was taped from the elbow joint attached to the lateral side of the scapula while maintaining the horizontal adduction of the shoulder joint at 120° and flexion of the elbow joint at 90° for the medial side. For the lateral side, the tape was attached to the lateral side slightly from the centre of the shoulder after the shoulder joint was lower at 70°. The wrist extensor was taped from the volar wrist on the affected side to extend the wrist joint, and the tape was attached to both the medial and lateral sides of the humeral epicondyle.
Proprioceptive Neuromuscular Facilitation (PNF)
Among the several types of proprioceptive neuromuscular facilitation was used as general physical therapy for both groups in this study. PNF treatment was applied to all patients using all five patterns below.
1) Upper extremity D2 flexion (Shoulder extension/adduction/internal rotation pattern): Subjects laid down in a supine hook lying position in which their hip and knee joints were flexed. In this position, the arm on the affected side, which was about to perform the exercise, was positioned at the 11 o'clock position, and the arm on the unaffected side was comfortably placed beside the trunk, and then shoulder flexion-abduction-lateral rotation occurred in the 7 o'clock direction of the patient, according to our direction.
2) Upper extremity D1 flexion (Shoulder extension/abduction/internal rotation pattern): Subjects laid down in a supine hook lying position in which their hip and knee joints were flexed. In this position, the arm on the affected side, which was about to perform the exercise, was positioned at the 1 o'clock position, and the arm on the unaffected side was comfortably placed beside the trunk. Then, shoulder flexion-adduction-lateral rotation occurred in the 5 o'clock direction of the patient, according to our direction.
3) Upper extremity D2 extension (Shoulder flexion/abduction/lateral rotation): Subjects laid down in a supine hook lying position in which their hip and knee joints were flexed. In this position, the arm on the affected side, which was about to perform the exercise, was positioned at the 7 o'clock position, and the arm on the unaffected side was comfortably placed beside the trunk. Then, shoulder extension-adduction-lateral rotation occurred in the 11 o'clock direction of the patient, according to our direction.
4) Upper extremity D1 extension (Shoulder flexion/adduction/lateral rotation): Subjects laid down in a supine hook lying position in which their hip and knee joints were flexed. In this position, the arm on the affected side, which was about to perform the exercise, was positioned at the 5 o'clock position, and the arm on the unaffected side was comfortably placed beside the trunk. Then, shoulder extension-adduction-lateral rotation occurred in the 1 o'clock direction of the patient, according to the researcher's direction.
5) Upper extremity chopping pattern (Chopping pattern): In the supine hook lying position, the leading arm on the affected side of the subjects performed shoulder joint flexion/adduction/external rotation, the scapula was in anterior elevation, the elbow joint was in extension-supination, and the wrist was in flexion-radial deviation. The trailing arm on the unaffected side performed chopping (shoulder joint extension/abduction/internal rotation, the scapula posterior depression, elbow joint extension-pronation, and wrist extension-ulnar deviation) while holding the wrist on the affected side and having the shoulder joint of the arm on the unaffected side in a flexion/abduction/external rotation state, according to the instruction of the researcher.
Each of these patterns was applied 10 times and a three minutes rest was given between patterns.
Assessment Methods
Korean Version of Modified Barthel Index (K-MBI)
In this study, the daily living activities of stroke patients were assessed using the Korean Version of the Modified Barthel Index (K-MBI). The composition of the K-MBI for activity assessment if the task could not be performed at all was set to step 1 (0 point), and if the task could be done completely independently, it was set to step 5. Thus, the better the patient’s independence in completing tasks, the higher the step was with an increasing number of points for each step. The K-MBI consisted of 10 items: personal hygiene, bathing, feeding, toilet transfer, stair climbing, dressing, bowel control, bladder control, ambulation, and chair/bed transfers, and the total score that could be reached was 100 points.
Korean version of Fugl-Meyer Assessment (K-FMA)
The Korean version of Fugl-Meyer Assessment (K-FMA) is a method used to quantitatively assess the functional recovery of stroke patients based on the recovery steps of motor functions after stroke. It consists of the upper extremity (66 points), lower extremity (34 points), balance (14 points), sensation (24 points), passive joint motion (44 points), and joint pain (44 points). Thus, it comprises six domains, and the total possible score is 226 points. For each item, zero to two points are scored, and the higher the score is, the better the motor control is. This study evaluated only the wrist (10 points) and hand (14 points), which are the distal portion items in the FMA to assess the motor performance ability in the upper extremity.
Action Research Arm Test (ARAT)
The Action Research Arm Test (ARAT) is an evaluative measure used to assess the functions of the upper extremities. This test consists of 19 items, and the total possible score is 57 points. Item scores are summed to create four sub-scale scores: grasp (18 points), grip (12 points), pinch (18 points), and gross motor (9 points). Prior tests were conducted before the therapeutic intervention in all of the above assessments, and the post-tests were conducted after the final therapeutic intervention.
Data Analysis
SPSS version 18.0 was used for the statistics of this study, and the mean ± standard deviation was described through descriptive statistics. To determine the difference between groups, an independent sample t-test and paired sample t-test were conducted to compare the results within groups before and after the intervention. The significance level of all statistical data analyses was set at α < 0.05.
RESULTS
The K-MBI score had a statistically significant difference before and after the experiment in both the experimental and control groups (P < 0.05). The comparison of the difference in the therapeutic effects, according to the therapeutic intervention, showed that the experimental group had more statistically significant differences than the control group (P < 0.05) (Figure 2).
The K-FMA wrist score had a statistically significant difference before and after the experiment in both the experimental and control groups (P < 0.05). The comparison of the differences in the therapeutic effects, according to the therapeutic intervention, showed no statistically significant difference between the experimental and control groups (P > 0.05) (Figure 3). However, the FMA hand score had a statistically significant difference before and after the experiment only in the experimental group (P < 0.05), and the comparison of the difference in the therapeutic effects, according to the therapeutic intervention, showed no statistically significant difference between the experimental and control groups (P > 0.05) (Figure 4).
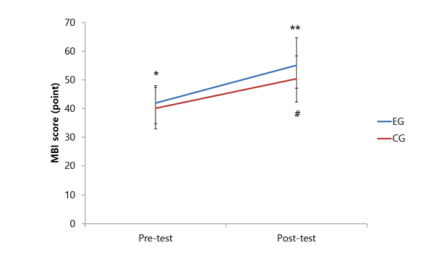
Figure 2: Comparison of MBI wrist score between groups. *p<0.05, **p<0.01 within the experimental group, #p<0.05 between groups. MBI, Modified Barthel index

Figure 3: Comparison of FMA wrist score between groups. *p<0.05, **p<0.01, within the experimental group. Data is presented as Mean±SD. FMA: Korean version of Fugl-Meyer assessment
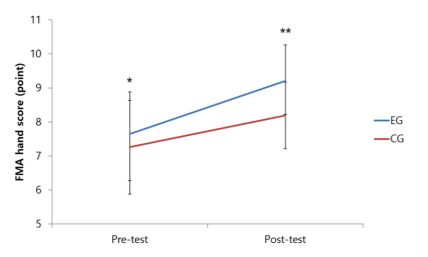
Figure 4: Comparison of FMA hand score between groups. *p<0.05, **p<0.01, within the experimental group. Data is presented as Mean±SD. FMA: Korean version of Fugl-Meyer assessment
The ARAT score had a statistically significant difference before and after the experiment in both the experimental and control groups (P < 0.05). The comparison of difference in the therapeutic effects, according to the therapeutic intervention, showed that the experimental group had more statistically significant differences than the control group (P < 0.05) (Figure 5).
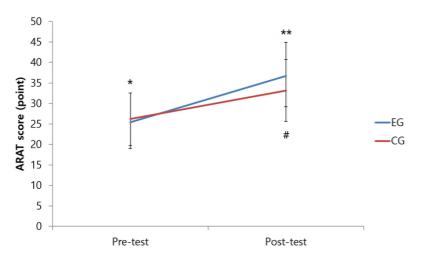
Figure 5: Comparison of ARAT hand score between groups. *p<0.05, **p<0.01, within the experimental group. Data is presented as Mean±SD. ARAT: Action research arm test
DISCUSSION
The elastic tape has similar elasticity to that of human skin. The principle and effect of taping therapy affect the skin, proprioception, muscles, fascia, and joints. Taping increases the circulation of blood and lymph fluid via a skin lift-up action. After applying the taping therapy, taping lifts the different layers of skin, which relaxes fascia, thereby encouraging blood flow and lymph drainage in the tissue. This can also decrease oedema and increase the re-absorption of substances that induce pain by improving the recovery of the damaged portion of the body.22
Taping acts on the skin to deliver the constant stimuli to the sensory nerves present in the skin, and these neurological signals are sent to higher centres in the CNS through the sensory nerves in the spinal cord. The blocking of pain through the stimuli of taping can be explained by the gate control theory. Because taping can transfer stimuli at a faster rate than the nociceptor that receives and feels the pain, it can suppress the signal transduction by closing the gate.23
The muscle spindle reflex, which is one of the functions of taping therapy acting on muscles, can recover the weakened functions of muscles. Muscle tension can be increased by assisting the muscle contraction and its direction using the tape's unique elasticity, and taping simulates the Golgi tendon to suppress the over-tension in the muscle and tendon, thereby helping the generation of optimal tension in the muscle. The proper tension in muscles can play an important role as a mechanism that controls posture and maintains balance. If the muscle portion with pain is not treated for a long time, compensation occurs in the other surrounding muscles, which induces secondary damage or leads to constant chronic pain. Thus, applying tape can be effective not only to correct muscle functions but also to prevent secondary damage.24,25
The application of taping therapy can treat joint damage by assisting or strengthening muscle activities. Joint degeneration occurs because excessive mechanical stress is put on a specific area without distributing the physical body load as the joints deviate. The abnormal load can wear off cartilage through the above series of the processes, and additional stress due to the damaged cartilage can occur again, which creates a vicious cycle. Joint damage can be prevented by stopping this vicious cycle by entering the process of recovery. Thus, joints can act in a normal position once the muscles are recovered to a normal state, and the joint range of motion can increase to improve the circulation of blood and lymph fluid, thereby preventing and delaying degenerative joints.26
As mentioned above, the effects of taping therapy can be summarized in the sense that taping therapy can reduce the pressure on joints during exercises and increase the circulation of blood and lymph fluid, which improves and enhances the motor functions of muscles. The application of taping therapy is also an intervention that helps stroke patient’s exhibit near-normal muscle performance. It is a therapeutic approach used to enable normal physical activities by attaching the elastic and adhesive tape to a portion of the human body along the direction of the affected muscle and fascia or motor points. Taping therapy is also used to prevent further damage and protect damaged tissues and brings many positive effects in various areas, such as clinical and sports medicine.27
There are two types of taping: nonelastic and elastic taping. Non-elastic taping largely aims to limit joint working force by fastening joints and pressurizing somebody portion. It can provide rigid assistance and support, but it has a drawback in that it is difficult to use. Besides, it can create creases on the tape due to an irregular surface of the physical body when applied. Thus, many exercises are needed for non-elastic taping to apply the non-elastic tape smoothly and efficiently. The non-elastic tape is a wrap made of fabric. It can be used solely for assistance or it can be applied together with white tape. It can provide appropriate assistance and support at a relatively inexpensive price compared to other types of tape. Thus, non-elastic taping is applied mainly for fastening and protection around the damaged portion of the body and can be usefully employed when the budget is small.28
Elastic tapes can control changes in length and elasticity, which can be extended according to the movements around the application portion. It is also made of fabric and has an advantage in that it can be variably applied to all physical body portions. In particular, when there are concerns about causing a neurovascular disorder due to excessive pressure on blood vessels or nerves by using non-elastic tape on portions where muscle contraction and relaxation are large as a result of too many muscles, elastic tapes are preferred to non-elastic tapes.29
Proprioception plays an important role in stabilizing joints. The muscle receptor plays a role as a converter to change the mechanical load into afferent stimulation in a series of processes that deliver neural information from the nerve terminal to the CNS, and the converted afferent information is integrated into the upper motor programs for accurate motor control, thus providing dynamic joint stability by generating muscle contraction and reflex. There have been previous studies conducted on proprioception. Afferent nerves of patients with hemiplegia due to stroke were removed, and the proprioception senses were lost for a long period. As a result, they employed compensatory strategies or learned incorrect motor methods. Because proprioception plays an important role in reducing the functional instability or pre-damage of joints, exercises to improve proprioception have been clinically applied many times. These types of exercises can improve balance and postural control abilities, which facilitates functional activities.30,31
PNF is a therapeutic exercise method that combines a facilitation technique that induces physical body functions, improvement of neuromuscular, and motor reactions with functional diagonal movement patterns. PNF can be used to improve muscle strength and endurance, such as stability, mobility facilitation, neuromuscular control, and coordinated movements. It can also be used to strengthen weak muscle groups by facilitating strong muscle groups using diagonal movement patterns through the stimuli of many senses to facilitate or strengthen motor reactions and recover functions. PNF can be used in all steps of rehabilitation, from early steps where isometric exercises can be applicable, to steps where patients can resist and move at faster speeds. Currently, it has been widely applied in sports medicine to treat damage to the CNS and peripheral nervous system and orthopaedic and neurosurgical diseases.32
PNF is largely divided into exteroceptor and proprioceptor stimuli and employs a basic procedure of patterns, timing, and irradiation. The exteroceptor stimuli provide a hint for a therapist to apply resistance to the appropriate muscle groups and in the direction where the patient would like to move. The contact points are located on possible agonist muscles or insertion of tendons and are adjusted based on the patient response and control level. The resistance in PNF when stimulating proprioceptors refers to the resistance in the three-dimensional direction and the amount of resistance should be proper to allow for patient movements.33
The PNF movement patterns can be divided into upper extremity, lower extremity, trunk, head, and temporomandibular patterns. These patterns create various patterns through the axes where main movements occur. When using each of the patterns clinically, a single pattern may have numerous changes if we apply rhythmic initiation, rhythmic stabilization, repeated contraction, the timing for emphasis, the dynamic reversal of antagonist, slow reversals, reversals of agonist and antagonist, contract-relax, hold-relax, and a combination of isotonic. The spiral and diagonal movement patterns in PNF are quite similar to movements occurring in functional activities, and these patterns create various patterns through the axes where main movements occur. Thus, it is necessary to set up which functions are needed to be improved and which muscles and joints need to be targeted before the PNF application.34
PNF can activate muscles on the affected side by applying to the upper and lower extremities on the unaffected side when muscle strength of upper and lower extremities on the affected side is weak or not formed well enough at the early onset of stroke. PNF can strengthen trunks using the scapula, pelvis, neck, and four limbs. Particularly, when PNF is used by holding the other hand of the affected, and moving both hands together, the trunks are strengthened. This pattern is introduced as a chopping and lifting pattern. The chopping pattern can stimulate the external oblique abdominis and rectus abdominis in the leading direction, and the internal oblique abdominis in the trailing direction. The lifting pattern can stimulate the entire extensor in the neck and back as well as the multifidus and rotatores in the trailing side, thereby strengthening the abdominal muscles and trunk extensors.35
The chopping technique is a training method used to facilitate weight shifting to both the lower extremities using the potential of the upper extremities, which was conducted to increase trunk stability through strengthening abdominal muscles. In this technique, the bodyweight moves in the direction of the lower extremities on the affected side while extending the flexed elbow joint, and patients themselves can experience how much their body should be shifted. Then, the isotonic combination technique can be applied to increase abdominal tension and weight shift. The therapist performed approximation (compression) to the knee joint of the patients, thereby performing information input for the proprioceptor action as well as increasing the stability of the lower extremities. The combination technique of isotonic in PNF refers to a technique that combines concentric, eccentric, and static contractions in the agonist's muscles without relaxation. In particular, eccentric contraction allows firing from the motor unit whose threshold is higher, and then the motor unit recruitment is selectively added. Thus, eccentric contraction is effective in extending soft tissue.36,37
The trunk and upper and lower extremities in human movements act together as a form of complete synergic muscles, and irradiation occurs from stronger to weaker muscles through the resistance of the patterns that strengthen the upper and lower extremities or trunk. A study on the electromyogram of PNF arm patterns reported that diagonal movements using arms among PNF techniques improved the functional activities of the upper extremities and stabilized the trunk muscles. Another study reported that activating the pectoralis major muscle and serratus anterior muscle, which was accessory respiratory muscles, influenced the increase in the activity of respiratory muscles.38,39
CONCLUSION
The present study applied PNF therapeutic and taping techniques together, which were both widely used in clinical fields as therapeutic interventions for improving proprioception. The study results showed that the experimental group, who applied PNF and elastic taping that could lead to improvements in proprioception improved functional activities, had significantly higher results than the control group. This result was obtained because of the synergistic effect of two interventions (PNF and taping) that maximized the proprioception stimuli. For future studies, the synergistic effect between therapeutic interventions on improving the interventions by stimulating the abilities of factors concerning patient functions will be investigated.
The limitations of this study were the small sample size, and the taping method that was applied was not sufficient enough to inhibit and stimulate all the functions in the upper extremities. We also did not conduct a study on non-elastic taping, which had positive effects on stability improvement, and applied only PNF treatment to improve proprioception. Thus, the study results cannot be generalized because we did not compare our results with other therapeutic interventions. The results of this study expect that more studies will be conducted on prolonged and synergistic effects between various exercises that improve proprioception based on quantitative evaluation methods targeting many other diseases.
ACKNOWLEDGMENTS: This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No-2019R1F1A1057731).
Conflict of Interest: NIL
Source of Funding: National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No-2019R1F1A1057731).
References:
-
Koh SH, Park HH. Neurogenesis in stroke recovery. Transl Stroke Res 2017;8(1):3-13.
-
Winters C, Kwakkel G, van Wegen EE, Nijland RH, Veerbeek JM, Meskers CG. Moving stroke rehabilitation forward: the need to change research. Neuro Rehabilitation 2018;43(1):19-30.
-
Knight-Greenfield A, Nario JJ, Gupta A. Causes of acute stroke: a patterned approach. Radiol Clin North Am 2019;57(6):1093.
-
Findlater SE, Dukelow SP. Upper extremity proprioception after stroke: bridging the gap between neuroscience and rehabilitation. J Motor Behav 2017;49(1):27-34.
-
Delhaye BP, Long KH, Bensmaia SJ. The neural basis of touch and proprioception in primate cortex. Compreh Physiol 2011;8(4):1575-602.
-
Kim JS, Caplan LR, Wong KS (eds): Intracranial Atherosclerosis: Pathophysiology, Diagnosis and Treatment. Front Neurol Neurosci 2016;40:58-71.
-
Etoom M, Hawamdeh M, Hawamdeh Z, Alwardat M, Giordani L, Bacciu S, Scarpini C, Foti C. Constraint-induced movement therapy as a rehabilitation intervention for upper extremity in stroke patients: systematic review and meta-analysis. Int J Rehabilit Res 2016;39(3):197-210.
-
Coutts SB. Preventing unnecessary disability after stroke in Scotland. Lancet 2019 Oct 5;394(10205):1225-1226.
-
Choi JH, Pile-Spellman J. Reperfusion changes after stroke and practical approaches for neuroprotection. Neuroimaging Clin 2018;28(4):663-682.
-
Klamroth-Marganska V. Stroke rehabilitation: Therapy robots and assistive devices. In Sex-Specific Analysis of Cardiovascular Function 2018:579-587.
-
Jung KM, Choi JD. The Effects of Active Shoulder Exercise with a Sling Suspension System on Shoulder Subluxation, Proprioception, and Upper Extremity Function in Patients with Acute Stroke. Int Med J Exp Clin Res 2019;25:4849.
-
Ghai S, Driller M, Ghai I. Effects of joint stabilizers on proprioception and stability: a systematic review and meta-analysis. Phys Therapy Sport 2017;25:65-75.
-
Aiello BR, Hardy AR, Westneat MW, Hale ME. Fins as mechanosensors for movement and touch-related behaviors. Integr Compar Biol 2018;58(5):844-859.
-
Ager AL, Roy JS, Roos M, Belley AF, Cools A, Hébert LJ. Shoulder proprioception: how is it measured and is it reliable? A systematic review. J Hand Therapy 2017;30(2):221-231.
-
Cassidy JM, Cramer SC. Spontaneous and therapeutic-induced mechanisms of functional recovery after stroke. Transl Stroke Res 2017;8(1):33-46.
-
de Oliveira KC, de Souza LA, Emilio MM, da Cunha LF, Lorena DM, Bertoncello D. Overflow using proprioceptive neuromuscular facilitation in post-stroke hemiplegics: A preliminary study. J Bodywork Movem Therap 2019;23(2):399-404.
-
Birinci T, Razak Ozdincler A, Altun S, Kural C. A structured exercise programme combined with proprioceptive neuromuscular facilitation stretching or static stretching in posttraumatic stiffness of the elbow: a randomized controlled trial. Clin Rehabilit 2019;33(2):241-252.
-
Sung YB, Lee JC, Kim K. Effects of taping and proprioceptive neuromuscular facilitation for stance phase duration of stroke patients. J Phys Therapy Sci 2017;29(11):2031-2034.
-
Lee SH. Related Factors of Health Behavior Compliance among Cardiac Rehabilitation Patients. Int J IT-based Public Health Mgmt 2019;6(1):73–82.
-
Park YK. The Special Education Teachers’ Perception on Independent Living Skills of Students with Intellectual Disabilities. Int J IT-based Public Health Mgmt 2019;6(1);65–72.
-
Chae MJ. The effect of simulation-based SBAR education program for nursing students. Int J IT-based Public Health Mgmt 2019;6(1):53–58.
-
Jassi FJ, Del Antônio T, Moraes R, George SZ, Chaves TC. Effects of functional taping compared with sham taping and minimal intervention on pain intensity and static postural control for patients with non-specific chronic low back pain: a randomised clinical trial protocol. Physiotherapy 2017;103(2):154-9.
-
Park YD, Park YJ, Park SS, Lee HL, Moon HH, Kim MK. Effects of taping therapy for carpal space expansion on electrophysiological change in patients with carpal tunnel syndrome. J Exerc Rehabilit 2017 Jun;13(3):359.
-
Shinozaki K, Nito M, Kobayashi S, Hayashi M, Miyasaka T, Hashizume W, Shindo M, Naito A. Monosynaptic facilitation of group I afferents between brachioradialis and extensor carpi radialis in humans. Neurosci Res 2017;114:30-34.
-
Lyle MA, Nichols TR. Evaluating intermuscular Golgi tendon organ feedback with twitch contractions. J Physiol 2019;597(17):4627-4642.
-
Nayanti AP, Prabowo T, Sari DM. The Effects of Kinesio Taping and Quadriceps Muscle Strengthening Exercise on Quadriceps Muscle Strength and Functional Status in Knee Osteoarthritis. J Med Health 2020;2(5).
-
Kim BR, Kang TW. The effects of proprioceptive neuromuscular facilitation lower-leg taping and treadmill training on mobility in patients with stroke. Int J Rehabilit Res 2018;41(4):343-348.
-
Kim M, Yoo K. Effect of Ankle Taping Type and Jump Height on Balance during Jump Landing in Chronic Ankle Instability. J Int Acad Phys Ther Res 2020;11(2):2077-2089.
-
Matheus JP, Zille RR, Matheus LB, Lemos TV, Carregaro RL, Shimano AC. Comparison of the mechanical properties of therapeutic elastic tapes used in sports and clinical practice. Phys Ther Sport 2017;24:74-78.
-
Röijezon U, Clark NC, Treleaven J. Proprioception in musculoskeletal rehabilitation. Part 1: Basic science and principles of assessment and clinical interventions. Manual Ther 2015;20(3):368-377.
-
Clark NC, Röijezon U, Treleaven J. Proprioception in musculoskeletal rehabilitation. Part 2: Clinical assessment and intervention. Manual Ther 2015;20(3):378-387.
-
Mirek E, Filip M, Banaszkiewicz K, Rudzi?ska M, Szymura J, Pasiut S, et al. The effects of physiotherapy with PNF concept on gait and balance of patients with Huntington's disease–pilot study. Neurologia i neurochirurgia polska. 2015;49(6):354-347.
-
Gunning E, Uszynski MK. Effectiveness of the proprioceptive neuromuscular facilitation method on gait parameters in patients with stroke: a systematic review. Arch Phys Med Rehabilit 2019;100(5):980-986.
-
Ribeiro TS, Silva WH, de Alencar Caldas VV, Silva DL, Cavalcanti FA, Lindquist AR. Effects of a training program based on the proprioceptive neuromuscular facilitation method on post-stroke motor recovery: a preliminary study. J Bodywork Movement Therap 2014;18(4):526-532.
-
Jones K, Forward M. Examining the Patterns of PNF in the Upper Limb during Normal Walking. Physiotherapy 2002;88(4):236-237.
-
Khamwong P, Pirunsan U, Paungmali A. A prophylactic effect of proprioceptive neuromuscular facilitation (PNF) stretching on symptoms of muscle damage induced by eccentric exercise of the wrist extensors. J Bodywork Movement Therap 2011;15(4):507-16.
-
Pin A, Filho S. Proprioceptive neuromuscular facilitation – PNF influence in the change of rectus femoris fiber view through surface electromyography and analogic dynamometry. Physiotherapy 2015;101:e1213–e1214.
-
Lee JH, Sung YB, Lee DH. The Rehabilitation Effect of PNF after Applying Upper Extremity Taping on Patients with Central Nervous System Injuries. Int J IT-Based Public Health Mgmt 2020;7(2):1-6.
-
Bertinchamp U. Facilitazione propriocettiva neuromuscolare: concetto PNF (Kabat-Knott-Voss). EMC-Medicina Riabilitativa 2017;24(4):1-2.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License