IJCRR - 8(3), February, 2016
Pages: 07-10
Date of Publication: 11-Feb-2016
Print Article
Download XML Download PDF
EMERGENCY PERIPARTUM HYSTERECTOMY: INCIDENCE, INDICATIONS AND FETOMATERNAL OUTCOME IN A TERTIARY CARE HOSPITAL
Author: Saima Wani, Perveena Fareed, Yasmeena Gull, Neha Mahajan
Category: Healthcare
Abstract:Objectives: The objectives of this study were to determine the incidence, maternal characteristics, indications and the maternal and perinatal outcome of emergency peripartum hysterectomies done in the Department of Obstetrics and Gynecology Government Medical College Srinagar. Study Design: This was a retrospective descriptive study done from January 2011-December 2013 over a three year period. Results: The incidence of peripartum hysterectomy during the study period was 1.46/1000 deliveries. The frequent age group was 31-35 years. The main indication of peripartum hysterectomy was life threatening hemorrhage due to uterine rupture (23), uterine atony (22), placenta accrete (18), placental abruption (16), placenta previa (13), broad ligament hematoma (7), retained placenta, Secondary postpartum hemorrhage and uterine fibroid (1 each) 81.37% hysterectomies were total and 16.63% were subtotal. The average pre- and intraoperative blood loss was 2.5 Lt +0.6. All patients needed blood transfusion. All patients received Perioperative antibiotics. Intraoperative complications developed in 15 patients which were bladder injury (5), Adnexial bleeding (5) and broad ligament hematoma (4). 69.6% patients needed intensive care. The common post operative complications were febrile morbidity (15.68%), wound sepsis (10.78%), pneumonia (8.82%), coagulopathy (5.88%), Cuff cellulitis and vesicovaginal fistula (1.96% each). The stillbirth rate was 303/1000. Most stillbirths occurred in uterine rupture (61.29%) followed by placental abruption (25.80%). Maternal mortality rate was 117/1000 live births. The average hospital stay was 13+4days. Conclusion: Emergency peripartum hysterectomy has significant effect on fetomaternal morbidity and mortality. Hence antenatal identification of high risk patients and proper management of second and third stage of labor and emergency preparedness are important in decreasing the rate of peripartum hysterectomy and improving the outcome.
Keywords: Emergency peripartum hysterectomy, Uterine rupture, Placenta accrete and uterine atony
Full Text:
INTRODUCTION
Emergency peripartum hysterectomy (EPH) is one of the life saving procedure performed after vaginal delivery or caesarean section or in immediate postpartum period done for intractable haemorrhage.1 The most common indication of EPH being severe uterine hemorrhage that cannot be controlled by conservative measures.2 Hemorrhage may be due to abnormal placentation like placenta accrete, atonic uterus, uterine rupture, uterine fibroid and coagulopathy.2,3,4 India the reported peripartum hysterectomy rate is 2.6 per 1000 live births.5 In United States, the rate is between 1.2 and 2.7 per 1000 births. 6,7 However the peripartum hysterectomy rate is lower in European countries( 0.2 per 1000 births in Norway8 and 0.3 per 1000 births in Ireland).9 Peripartum hysterectomy is associated with severe blood loss, risk of transfusion, intraoperative complications and significant postoperative morbidity and mortality. Maternal mortality rate with EPH ranges from 0-30%.10
MATERIALS AND METHODS This retrospective descriptive study was carried in the Department of Obstetrics and Gynecology GMC Srinagar from January 2011-December 2013. Ethical clearance was taken from ethical committee. All the patients who underwent Emergency peripartum hysterectomy were identified from operative room, labor room and intensive care unit record book. Peripartum hysterectomy was defined as hysterectomy performed after 24 weeks of gestation at the time of delivery or within 42 days of delivery. Hysterectomies done before 24 weeks gestation for any reason were excluded from the study. The total number of deliveries during that period was also identified. Medical record sheets of above patients were analyzed in detail. The age, parity, indication for hysterectomy, blood loss, type of hysterectomy, intraoperative and postoperative complications, blood transfusion, fetomaternal outcome, duration of hospital stay and need for Intensive care were noted. Records of blood loss included blood loss before and during surgery.
Febrile morbidity was defined as a temperature of 38o C or more on any two consecutive days excluding first 24 hrs. Wound infection was defined as the presence of any two of the following: purulent discharge/obvious cellulitis, elevated temperature and positive wound culture. Data obtained was analyzed with the SPSS 10.0 for windows.
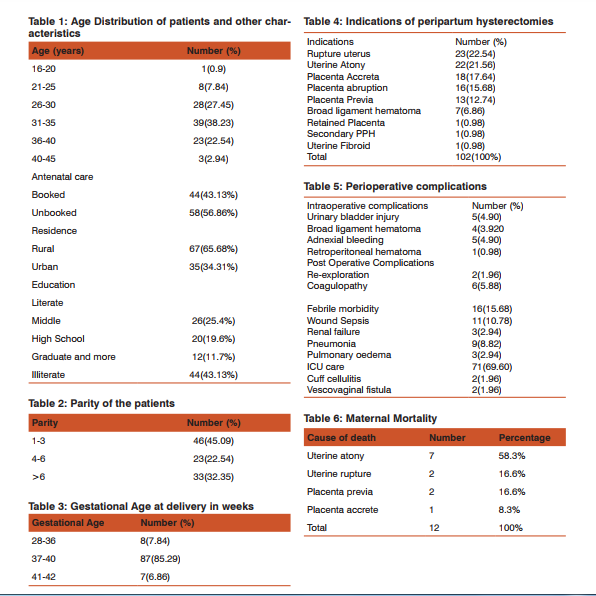
RESULTS There were 102 peripartum hysterectomies performed during this three year period from January 2011- December 2013. During this same period there were a total of 69742 deliveries. The peripartum hysterectomy rate was therefore 1.46/1000 deliveries. The age of patients ranged from 16-45 years. (Table 1). The highest number of patients was in the 31-35 yr age group followed by 26-30 yr group. The parity of patients ranged from 1-6 (Table 2). The highest frequency was in those from Para 1-3 followed by women more than Para 6. The gestational age of patients ranged from 28-42 weeks. Most common gestational age was 37-40 weeks followed by 28-36 weeks. The indication of peripartum hysterectomy was hemorrhage due to rupture uterus; uterine atony; placenta accrete; placental abruption; placenta previa; broad ligament hematoma; secondary postpartum hemorrhage, retained placenta and uterine fibroid (1 each). Conservative methods were tried in patients with atonic uterus before the final decision of hysterectomy.
The conservative methods include use of Oxytocics, Systematic devascularisation and uterine tamponade. 83(81.37%) of the hysterectomies were total and 19 (16.63%) were subtotal. Estimated blood loss ranged from 1-5 Lt with a mean of 2.5+0.9. All patients received Perioperative antibiotics. Blood transfusion was needed in all patients (100%). Intraoperative complication occurred in 15 patients. These were urinary bladder injury (5), broad ligament hematoma (4), Adnexial bleeding (5), and retroperitoneal hematoma (1). 71(69%) patients needed ICU care.
Two patients needed reexploration and 6 had coagulopathy. Postoperatively 16 patients developed febrile morbidity, 17 had wound infection, 2 developed Vesicovaginal fistula. The maternal mortality rate was 117/1000. The maternal mortality was distributed as under (Table 6).There were 71 live births and 31 still births. The still birth rate was 303/1000 births.19 stillbirths occurred in uterine rupture, 8 occurred in placental abruption and 4 in uterine atony. The mean duration of hospital stay was 13+4days with a range of 8-45days.
DISCUSSION This was a retrospective descriptive study conducted in the Department of Obstetrics and Gynecology, GMC Srinagar from January 2011-December 2013. Peripartum hemorrhage is a major cause of maternal morbidity and mortality and emergency hysterectomy is a means of controlling life threatening hemorrhage. In the study period the hysterectomy rate was 1.46/1000 deliveries. This rate is comparable (1.2/1000) to rates observed by Sebitloane et al.11 Similar peripartum hysterectomy rate was observed by Nasrat et al.12 The highest frequency of patients was in age group 31-35 years. Similar observations were made by Kwame-Aryee et al.13 The major indications of peripartum hysterectomy were uterine rupture followed by uterine atony.
This is consistent with findings by Shava J et al.14Nasrat et al had uterine atony as major cause followed by uterine rupture.12 83(81.37%) hysterectomies were total and 19(16.63%) were subtotal. It has been suggested that performing emergency total hysterectomies is unnecessary.15 Advocates of total hysterectomy have suggested the long term complications of vaginal discharge, vaginal bleeding and need for cervical cytology as reason for performing total hysterectomy. Emergency peripartum hysterectomy has high complications because of increased blood supply to the pelvic organs dur- ing pregnancy and distorted pelvic anatomy due to gravid uterus.16 Twenty three (22.54%) of patients had complications with some patient having more than one complication. Similar observations were made by Zorlu et al,17 Kwame-Aryee et al 13 and Sebitloane et al.11As majority of the complications are due to hemorrhage and injury to urinary tract, the obstetrician should be assertive in making early decision of hysterectomy before the patient exsanguinates, reduce operative time by clamping and the uterine pedicles off first till uterine arteries are secured, then proceed with suturing and tying the pedicles and be familiar with pelvic anatomy.
The still birth rate was 303/1000 births with 19(61.29%) deaths in uterine rupture and 25.8% in placental abruption. The still birth rate is similar to rates by Sebitloane et al.11and Adanu et al.18 Maternal mortality rate was 117/1000 in the study. Uterine atony accounted for 58.3%, uterine rupture and placenta previa for 16.6% each. The mortality rate was higher than observed in some studies.17,19 Kwame-Aryee et al 13had maternal mortality rate of 12.9%. About 1/3rd of cases of peripartum hysterectomies were performed in patients who were thought to be low risk for the procedure. Residents should be made aware of the risk factors and be technically exposed to this procedure by encouraging them to assist in difficult hysterectomies.
Use of live videotapes may compliment this exposure in teaching institutions. Patients at risk of peripartum hysterectomy should be identified and counseled regarding delivery in a hospital that has blood bank facility, backup of experienced obstetricians and availability of intensive care unit. As caesarean section is a risk factor for hysterectomy, its rate should be reduced and trial of vaginal birth after caesarean section should be given to patients.
CONCLUSION Emergency peripartum hysterectomy has significant effect on fetomaternal morbidity and mortality. Hence antenatal identification of high risk patients and proper management of second and third stage of labor and emergency preparedness are important in decreasing the rate of peripartum hysterectomy and improving the outcome.
ACKNOWLEDGEMENT Authors acknowledge the immense help received from the scholars whose articles are cited and included in references of this manuscript. The authors are also grateful to authors/ editors/ publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
References:
1. Plauche WC, Grunch FG, Bourgeouis MO. Hysterectomy at the time of caesarean section: analysis of 108 cases. Obstet Gynecol.1981; 58:459-64.
2. Sellhas-CS Gilbert S, Landon MB, Verner MW, Leveno KJ, hauth JC, et al. Eunice Kennedy Shriver institutes of health and human development maternal-fetal medicine units network. The frequency and complication rates of hysterectomy accompanying caesarean delivery. Obstet Gynecol 2009; 114:224-9.
3. Zwart JJ, Dijik PD, Van Roosmalen J. Peripartum hysterectomy and arterial embolization for major obstetric haemorrhage: A nationwide cohort study in the Netherlands. Am J Obstet Gynecol 2010;202:150.
4. Rachaga S, Sivanesaratnam. Caesarean hysterectomy: a review of 21 cases in the university hospital, Kaula Lumpur. Eur J Obstet Gynecol Reprod Biol. 1984; 16:321-6.
5. Anita K, Kavitta WW. Emergency Obstetric hysterectomy. J Obstet Gynecol India 2005; 55:132-4.
6. Kastner ES, Figueroa R, Garry D, Naulik D. Emergency peripartum hysterectomy; experience at a community teaching hoslital. Obstet Gynecol 2002; 99: 971-5.
7. Stance LM, Schrimmer OB, Paul RM, Mishell DR. Emergency peripartum hysterectomy and associated risk factors. Am J Obstet Gynecol 1993; 168:879-83.
8. Engleson IB, Albrechsen S, Iverson OF. Peripartum hysterectomy- incidence and maternal morbidity. Acta Obstet Gynecol Scand 2001; 80:409-12.
9. Langdana M, Geary W, Haw D, Kean F. Peripartum hysterectomy in the 1990: a new lesson. J Obstet Gynecol 2001; 21:121-3.
10. Bodelon C, Bernabe Ortiz A, Schiff MA, Reed SD. Factors associated with peripartum hysterectomy. Obstet Gynecol 2009; 114:115.
11. Sebitloane MH, Moodley J. Emergency peripartum hysterectomy. East Afr J 2001;78(2):70-74.
12. Nasrat HA. Near-miss obstetric morbidity in inner city hospital in Saudi Arabia. East Mediterr Hlth J 1999;5 (4):712-726.
13. Kwame-Aryee R. A, Kwakye A, K, Seffah J.D. Peripartum hysterectomies at the Korle-BU teaching hospital; A review of 182 cases. Ghana Medical journal. 2007; 41:133-38.
14. Shava J, Masihleho GE, Mazibuko MD. Peripartum hysterectomy at Ga-Rankuwa hospital: A two and a half year review. Cent Afr J Med 1996; 42:25-28.
15. Heij HA, Te Velde ER, Cairns JM. Management of rupture of the gravid uterus. Trop Doct 1985; 15:127-31.
16. Barclay DL. Caesarean hysterectomy at the charity hospital in New Orleans-1000 consecutive operations. Clin Obstet gynecol 1969; 12:635-637.
17. Zorlu CG, Turan C, Isik AZ, Danisman N, Mungan T, Gokmen O. Emergency hysterectomy in modern practice. Changing clinical perspective in time. Acta Obstet Gynecol Scand 1998; 77:186-190.
18. Adanu RMK, Obed SA. Rupture uterus: A seven year review of cases from Accra, Ghana. J Obstet Gynecol Can 2003; 25:225- 230.
19. Gonsoulin W, Kennedy RT, Guirdy KH. Elective versus emergency caesarean hysterectomy cases in a residency programme setting: A review of 129 cases from 1984-1988. Am J Obstet Gynecol 1991; 65:91-94.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License