IJCRR - 13(3), February, 2021
Pages: 103-107
Date of Publication: 03-Feb-2021
Print Article
Download XML Download PDF
Incidence of Hearing Loss in COVID-19 Patients: A COVID Hospital-based Study in the Eastern Part of India
Author: Santosh Kumar Swain, Somya Ranjan Pani
Category: Healthcare
Abstract:Background: The coronavirus disease 2019(COVID-19) is an acute respiratory disease caused by a novel coronavirus(SARS CoV-2). Clinically COVID-19 presented with respiratory illness and also death is a possible outcome. Hearing loss is an interesting clinical outcome associated with COVID-19 infections. Objective: This study is designed to analyze the incidence of hearing loss in COVID-19 patients after discharge from the COVID-19 hospital. Methods: Twenty-eight patients of COVID-19 discharged from COVID hospital presenting with hearing loss participated in this study. The age ranges from 16 years to 52 years. Patients those had hearing loss before admission to COVID hospital were excluded from this study. All these patients underwent pure tone audiometry, tympanometry and Otoacoustic emission study. Results: Out of 28 patients, 18 (64.28%) were male and 10 (35.71%) were female with male to female ratio of 1.8:1. The age ranges of the participants were 16 to 52 years. Twenty-two patients presented with unilateral hearing loss and six presented with bilateral hearing loss. Out of 28 patients, 24 (85.71%) were presented with sensorineural hearing loss (SNHL) and 4 (14.28%) presented with conductive hearing loss. Out of the 28 patient 21 patients (75%) presented with unilateral hearing loss whereas 17 (60.71%) showed sudden-onset hearing loss. Conclusion: Hearing loss in COVID-19 has not received much attention by the medical professionals.COVID-19 infection could have deleterious effects on the inner ear specifically on the hair cells of the cochlea despite patients are asymptomatic. The proper understanding of the mechanisms behind hearing loss in COVID-19 infections needs further research.
Keywords: Hearing loss, COVID-19, Sudden sensorineural hearing loss, Cochlear function
Full Text:
INTRODUCTION
Hearing loss has an important role in communication and interaction, causing an invisible handicap of the affected person and psychological solitary confinement. World health organization (WHO) has estimated that approximately 360 million people with disabling hearing loss in the world which proved that more than half of the persons with hearing loss can be prevented by early diagnosis and treatment.1 The symptomatology of the COVID-19 may appear in 2 to 14 days after the exposure.2 The clinical symptoms include cough, throat pain, fever, fatigue, loss of taste and smell and few patients also present with gastrointestinal symptoms. The elderly persons or patients with co-morbidity systemic diseases are susceptible to infections and serious outcome which may be associated with acute respiratory distress syndrome (ARDS) and cytokine storm.2,3 The link between the COVID-19 infection and hearing loss makes intuitive sense, given the neuropathic manifestations of the inner ear and auditory nerve leading to sensorineural hearing loss. Although certain viral infections cause hearing loss, there is still unknown whether COVID-19 infections lead to auditory dysfunction or not. Here this study is relating to the impact or incidence of the novel coronavirus infection on the auditory system.
MATERIALS AND METHODS
This prospective study was conducted at a tertiary care teaching hospital attaching with five COVID hospital of 1200 COVID patients. The study was done during the period between March 2020 to August 2020. This study was approved by the Institutional ethical committee (IEC) with reference number IMS/SOA/23/26.02.2020. Informed consent was obtained from the patients those participated in this study. The audiological symptoms were searched from 472 patients at COVID-19 hospital. Out of the 472 patients, 28 (5.93%) were presented with hearing loss. There were suggested to consult the otolaryngology outpatient department after discharge/cure after the treatment or staying for 10 days at COVID hospital. The patients those were complaining about hearing loss after discharge from COVID hospital attended the outpatient department of the otorhinolaryngology included in this study. Patients were declared COVID-19 positive by real-time polymerase (RT-PCR) testing. All the patients those participated in this study were tested positive RT-PCR for SARS-CoV-2 before admission to the COVID hospital. COVID-19 patients with a history of ototoxic drugs like oral hydroxychloroquine and aspirin taken previously were excluded from this study. Patients those with hearing loss before SARS-CoV-2 infection were excluded from this study. Patients with a history of noise exposure, age-related hearing loss, measles, mumps, rubella, meningitis, syphilis, hypertension, thyroid diseases and kidney diseases before COVID-19 infections also were excluded from this study. Proper history taking and otological examinations including tuning fork tests were done in all the participants before audiological testing. All the participating patients underwent pure tone audiometry testing, tympanometry and Otoacoustic emissions (OAE) which were done by an audiologist in a soundproof room. The pure tone audiometry was performed with all safety protocols for COVID-19 pandemic. Pure tone audiometry findings were done with frequency at 250, 500, 100, 2000, 4000 and 8000Hz using Telephonics TDH39 earphones. The audiometric assessment was conducted in a sound-treated room, using GSI 61 clinical audiometer. The average value for the hearing threshold at 500Hz, 1000Hz and 2000Hz was calculated. The pure tone average greater than 25 decibels was considered as hearing loss. Tympanometry was carried out with help of the am plaid 775 middle ear analyzer to rule out middle ear pathology. Before performing the pure tone audiometry, tuning fork tests were done by using 256,512 and 1024 Hz. Transient evoked otoacoustic emissions (TEOAEs) were recorded in all participating patients with help of the Madsen Capella Analyzer. The stimuli in TEOAEs were a nonlinear click of about 80 dB peak SPL in the ear canal. The spectrum analyzer was stimulated as 4ms after the presentation of the stimuli for avoiding the ringing of the input stimuli and the temporal window was set at 20ms.
RESULTS
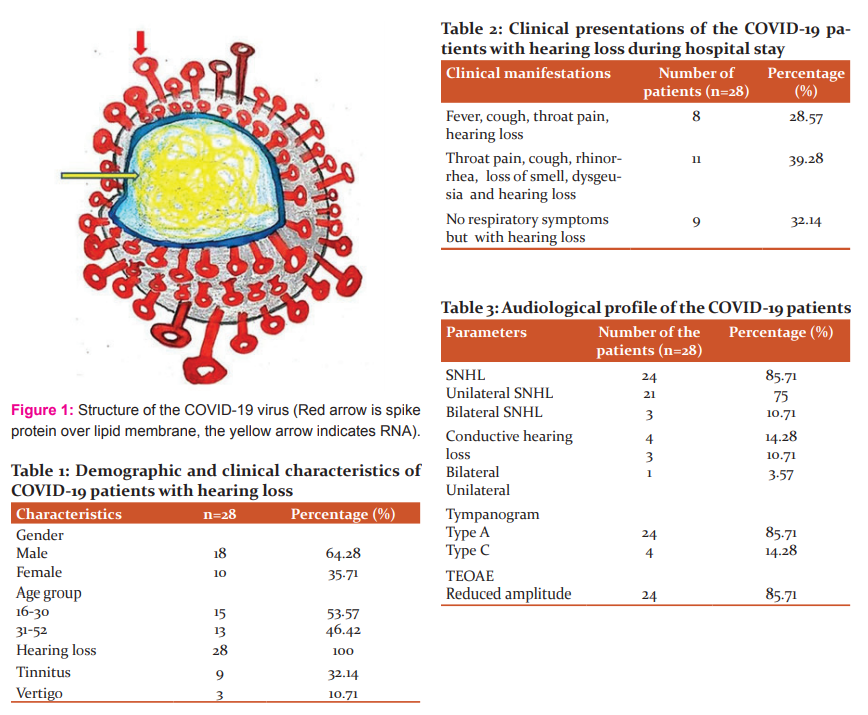
In this prospective study, 28 patients presented with hearing loss out of the 452 COVID-19 patients. Twenty-eight patients participated in this study for further audiological assessment at the otolaryngology department. Out of the 28 patients, 18 (64.28%) were male and 10 (35.71%) were female with male to female ratio of 1.8:1 (Table 1). The age ranges of the patients were 16 to 52 years with a mean age of 28.2 years. There were 15 patients (53.57%) were in the age range of 16 to 30 years and 13 patients (46.42%) in the age range of 31 to 52 years (Table 1). All were discharged from COVID-19 hospital and presented with the heaviness of the ear and hearing loss during six months of the study period. Out of the 28 patients, 19 (67.85%) were symptomatic and 9 (32.14%) had no symptoms except hearing loss (Table.2). Out of them, 11 patients presented with throat pain, cough, rhinorrhea, loss of smell, dysgeusia and hearing loss during the stay at the COVID hospital. Eleven patients presented with fever, cough, throat pain and hearing loss. Out of the 28 study patients, no respiratory symptoms were there but along with the presence of hearing loss. Out of the 28 patients, 22 were presented with unilateral hearing loss and 6 were presented with bilateral hearing loss. Out of 22 cases of unilateral hearing loss, 21 were with sensorineural hearing loss one patient presented with mild conductive hearing loss (Table.3). Out of 21 unilateral SNHL,17 (60.71%) presented with sudden onset. Out of the 17 cases of sudden sensorineural hearing loss, 11 (52.38%) were treated early and improved. Out of the 21 cases (75%) of unilateral sensorineural hearing loss, 9 cases (32.14%) presented with tinnitus and 3 (10.71%) had a history of vertigo immediately after development of the hearing loss with nausea and no vomiting. Out of 21 patients with unilateral SNHL, 13(61.90%) showed in the left ear and 8(38.09%) showed in the right ear. Out of 6 bilateral hearing loss, 3 were mild conductive and 3 were mild sensorineural hearing loss. Out of 24 cases of SNHL, 16 cases (66.67%) show high-frequency SNHL in pure tone audiometry. Tympanometry was done in all the participants. All the patients with SNHL were showing Type-A tympanogram whereas patients with conductive hearing loss showing Type-C tympanogram. Out of the 28 patients, 22 (78.57%) showed reduced amplitude of the TEOAEs. All the patients with sensorineural hearing loss were treated with oral prednisolone 1mg/kg/day in the tapering dose for three weeks along with vitamin B-complex and proton pump inhibitor daily.
DISCUSSION
COVID-19 is a contagious disease caused by a novel virus called severe acute respiratory syndrome coronavirus 2(SARS-CoV-2). This virus is a large, encapsulated positive-strand RNA virus (Figure 1). The coronavirus is classified into 4 genera such as alpha, beta, delta and gamma. Alpha and beta are usually caused the infection to human beings.4 The first case was reported in In Wuhan, China in late December 2019, the 1st case of COVID-19 was reported and spread worldwide.5 The symptoms of the COVID-19 infection may appear after 2 to 14 days following the exposure(based on the incubation period of COVID-19 virus). The clinical presentations of the COVID-19 patients are fever, cough, fatigue, gastrointestinal symptoms, sore throat, headache, olfactory and taste dysfunctions.6 The elderly patients and the persons with co-morbid conditions or immunocompromised conditions are prone to serious outcomes such as acute respiratory syndrome (ARDS) and cytokine storm.6 Three outcomes may happen in the disease process of the COVID-19 such as some become serious with respiratory distress, some improve with treatment and rest recovers with no medical intervention.7 Sometimes the COVID-19 patients present with otological manifestations. The eustachian tube is often blocked because of the infections at the nasal cavity and nasopharynx. The blockage of the eustachian tube cause blockage sensation in the ear and also ear pain. It leads to acute otitis media and manifests severe otalgia and fever. It also results in hearing loss due to persistent eustachian dysfunction.8 In this study, four patients were showing type-C tympanogram and conductive hearing loss. In COVID-19 infections, the nasopharyngeal infections lead to blockage of the eustachian tube because of the mucosal oedema of the nasopharyngeal end of the tube. It may cause negative pressure in the middle ear which may cause type-C tympanogram. Eustachian tube dysfunction often leads to glue ear formation and conductive hearing loss.9 Auditory or cochlear dysfunction in patients with coronavirus infection is little mentioned in the medical literature. The pathogenesis for COVID-19 infections leading to the hearing loss is not well established. Inner ear damage secondary to the viral infection is typically intra-cochlear but some viruses also damage auditory brainstem as well.
The pathophysiology for making injury of the peripheral auditory system includes the direct viral damage to the organ of Corti, stria vascularis and spiral ganglia. The viral damage to the cochlea is mediated by the patient’s immune system against virally expressed antigen/proteins as in cytomegalovirus and immunocompromised as in Human Immune deficiency virus and measles.10 In one report, brainstem involvement was found by a corona virus. 11 There are several reports regarding hearing loss by viral infections. Hearing loss due to viral infections can be congenital or acquired, unilateral or bilateral. Certain virus directly damages the inner ear and other induces the inflammatory responses which lead to damage of the inner ear whereas few viruses enhance the susceptibility of bacterial or fungal infections of the labyrinth, leading to hearing loss. Virus-induced hearing loss is often sensorineural, although conductive and mixed types of hearing loss may be found after infections of certain viruses. Sometimes, recovery of the hearing occurs spontaneously after viral infection.12,13 Typically viral infection causes a sensorineural type of hearing loss whereas a viral aetiology such as measles virus was documented for otosclerosis.14 The measles virus is an enveloped single-stranded RNA virus as SARS CoV-2 is transmitted through contact with respiratory secretions from the patient. Hearing loss was an important complication in measles virus infections before widespread vaccination.
HIV infection can cause conductive hearing loss through fungal and bacterial infections, which become common after immunosuppression by the virus.15 Hearing loss by viral infections may be mild or severe to profound and unilateral or bilateral. The mechanism of the hearing loss by viral infections varies greatly and ranges from direct damage to the labyrinthine or inner structures such as hair cells and organ of Corti as in measles to induction of the host immune-mediated damage to the inner ear.16 Viruses are often known to cause neurological complications like anosmia, facial nerve weakness and sudden sensorineural hearing loss.17 In the past SARS outbreak, coronavirus was documented for causing loss of the smell and taste because of the nerve injury.18 In this study, 11 patients were presenting loss of smell and loss of taste/dysgeusia along with hearing loss. The viral etiological agents have been associated with SNHL are herpes simplex virus, human immunodeficiency virus, hepatitis virus, rubella virus, measles virus, mumps virus, Lassa virus and enterovirus.18 The present pandemic of the COVID-19 is associated with SNHL as in this study. In this 24 patients presented with SNHL where 17 of them presented with sudden onset of SNHL. Sudden hearing loss is usually a frightening symptom which prompts the patient for an urgent consultation tot the health care provider. In the majority of the cases with sudden sensorineural hearing loss, the aetiology is idiopathic and if it is not diagnosed early and treated promptly may lead to persistent or permanent hearing loss and even with tinnitus and decreased patient quality of life (QOL).19 Intra-tympani steroid, systemic steroid and hyperbaric oxygen are different treatment options for sudden sensorineural hearing loss.20,21 In our cases of sudden sensorineural hearing loss, oral steroids were prescribed in tapering doses. Out of the 17 cases of sudden sensorineural hearing loss, 11 patients were treated promptly and improved to normal.
Tuning fork tests, pure tone audiometry, tympanometry and Otoacoustic emissions (OAE) were done to evaluate the hearing loss in our study patients with COVID-19. The type and degree of hearing loss were assessed by the tuning fork test and pure tone audiometry. In this study majority of the cases with SNHL (66.66%) show high-frequency hearing loss in pure tone audiometry. Tympanometry was done to assess the middle ear pathology. Otoacoustic emissions represent a form of energy produced from the outer hair cells of the cochlea. Otoacoustic emissions can be spontaneous (SOAEs), evoked by transient stimuli like clicks or tone bursts (TEOAEs). TEOAEs are not invasive and can be easily performed. For performing TEOAEs, the time is short, low cost and high sensitivity.22 In all the cases of SNHL, TEOAEs picked up the subtle deterioration in the outer hair cell functions of the cochlea. The high frequencies tones were also lower than normal in COVID-19 patients with SNHL. These outcomes may be attributed to the damaging effects of the SARS CoV- 2 viruses infection on the outer hair cells but the exact mechanism is still not clear. The outcome of this study also revealed that the absence of the major clinical symptoms may hide the unknown effect on the cochlea. Majority of the people infected with SARS CoV-2 virus with mild to moderate respiratory illness are recovered without special treatment.6 COVID-19 infections have a hazardous effect on the cochlear functions despite being the majority of the patients in this study are asymptomatic to mild symptoms. The mechanism for this deleterious effect on the cochlear hair cells requires further research. There is a large gap in the understanding of the etiopathogenesis, epidemiology, clinical presentations like hearing loss and human transmission of this disease. There should be continuous monitoring of the hearing loss and tracing of this COVID-19 is needed to ensure the detailed understanding of this inner ear pathogenesis. The most typical manifestations of chest CT were ground-glass opacities, patchy, cord-like, and nodular. Pleural thickening was found in some patients.
Computed tomography (CT) scan of the lungs is significant for early diagnosis and assessment of COVID-19 infection. The most typical presentations in CT scan of the chest include ground gland opacities, patch, cord-like and nodular appearance in the lungs. The pleural thickening is seen in some cases of COVID-19 patients. The CT findings of the lungs appear earlier than clinical symptoms and these findings hanged dynamically as the progression of the disease. So, the CT scan of the chest plays an important role in revealing the disease progression and severity of the disease.23,24 However, authors only included the observational study related to the incidence of the hearing loss of COVID-19 patients and not included the infectivity of the patients about RT-PCR and CT scan of the lungs. Our study surely helps for further study of the hearing loss and infectivity about the RT-PCR and CT scan of the chest with cord score. This study has a relatively small sample size due to rarity of the clinical outcome (hearing loss) in COVID-19 infections which may limit the outcome of the above interpretation. However, the clinical outcome of auditory dysfunction in this study will surely encourage further research.
CONCLUSION
Patients with OVID-19 infections have a higher chance of the hearing loss specifically sensorineural hearing loss. The exact role for pathogenesis of the hearing loss in COVID-19 infections is not well defined. We would like to recommend routine screening of all the COVID-19 positive cases with pure tone audiometry, tympanometry and Otoacoustic emission for early diagnosis of the hearing loss and prompt treatment or rehabilitation. Awareness regarding hearing loss in COVID-19 patients is often crucial in the current pandemic. Early identification of the COVID-19 patients with isolation and early initiation of the targeted treatment for the patients helps to reduce the incidence of the SNHL. For the proper understanding of the pathogenesis of the hearing loss in COVID-19 infections, a large study is required with follow up. Hearing health care providers or clinicians are now encountering a challenge for hearing loss in COVID-19 pandemic. Development of the vaccines may reduce the incidence of hearing loss.
Conflict of interest: Nil
Funding: No Funding sources were granted or used specifically for this work.
Author Contribution: SKS: Concept, data collection and data analysis; SRP: Data collection, data analysis, and drafting the manuscript.
References:
1. World Health Organisation fact sheet. Deaness and Hearing loss. In:World Health Fact Sheet ed. Geneva: World Health Organization; Feb. 2017. Available at www.who.int/mediacentre/factsheets/fs300/en.
2. Hong H, Wang Y, Chung HT, Chen CJ. Clinical characteristics of novel coronavirus disease 2019 (COVID-19) in newborns, infants and children. Pediatr Neonatol 2020;61(2):131-132.
3. Swain SK, Das S, Padhy RN. Performing tracheostomy in intensive care unit-A challenge during COVID-19 pandemic. Siriraj Med J 2020;72(5):436-442.
4. de Wilde AH, Snijder EJ, Kikkert M, vanHemert MJ. Host factors in corona virus replication. Curr Top Microbiol Immun 2018;419:1-42.
5. Wang W, Tang J, Wei F. Updated understanding of the outbreak of 2019 novel coronavirus (2019-nCoV) in Wuhan, China. J Med Virol 2020;92(4):441-447.
6. Hong CZ, Tan YY, Chen SD, Jin HJ, Tan KS, Wang DY, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak – an update on the status. Mil Med Res 2020;7:11.
7. Coronavirus disease 2019 (COVID-19) pandemic: Increased transmission in the EU/ EEA and the UK – seventh update, 25 March 2020. Stockholm: ECDC; 2020. Stockholm: Europ. Centre for Disease Prevention Control 2020.
8. Cui C, Yao Q, Di Zhang YZ, Zhang K, Nisenbaum E, Cao P, et al. Approaching otolaryngology patients during the COVID-19 pandemic. Otolaryngol Head Neck Surg 2020;1(2):234-237.
9. Fisher E, Youngs R, Hussain M, Fishman J. Glue ear in adults, paediatric sleep apnoea and the nose in exercise. J. Laryngol Otol 2016;130(5):417.
10. Abramovich S, Prasher DK. Electrocochleography and brain-stem potentials in Ramsay Hunt syndrome. Arch Otolaryngol Head Neck Surg1986;112(9):925-928.
11. Wege H, Watanabe R, Ter Meulen V. Relapsing subacute demyelinating encephalomyelitis in rats during coronavirus JHM infection. J Neuroimmunol 1984;6(5):325-336.
12. Adler SP. Congenital cytomegalovirus screening. Pediatr Infect Dis J 2005;24(12):1105-6.
13. Al Muhaimeed H, Zakzouk SM. Hearing loss and herpes simplex. J Trop Pediatr 1997;43(1):20-24.
14. Karosi T, Konya J, Petko M, Sziklai I. Histologic otosclerosis is associated with the presence of measles virus in the stapes footplate. Otol Neurotol 2005;26(6):1128-1133.
15. Chandrasekhar SS, Connelly PE, Brahmbhatt SS, Shah CS, Kloser PC, Baredes S. Otologic and audiologic evaluation of human immunodeficiency virus-infected patients. Am J Otolaryngol 2000;21(1):1-9.
16. Budzilovich GN, Lieberman AN. Herpes zoster oticus and facial paralysis (Ramsay Hunt syndrome). Clinicopathologic study and review of the literature. J Neurol Sci 1973;20(2):149-159.
17. Mateer EJ, Huang C, Shehu NY, Paessler S. Lassa fever-induced sensorineural hearing loss: neglected public health and social burden. PLoS Negl Trop Dis 2018;12:e0006187.
18. Suzuki M, Saito K, Min WP, Vladau C, Toida K, Itoh H, et al. Identification of viruses in patients with postviral olfactory dysfunction. Laryngoscope 2007;117:272-277.
19. Dallan I, Fortunato S, Casani AP, Bernardini E, Sellari-Franceschini S, Berrettini S, et al. Long-term follow up of sudden sensorineural hearing loss patients treated with intra-tympanic steroids: audiological and quality of life evaluation. J Laryngol Otol 2014;128:669-673.
20. Han X, Yin X, Du X, Sun C. Combined intratympanic and systemic use of steroids as a first-line treatment for sudden sensorineural hearing loss: a meta-analysis of randomized, controlled trials. Otol Neurotol 2017;38(4):487-495.
21. Swain SK, Achary S, Das SR.Vertigo in pediatric age: Often challenge to clinicians. Int J Cur Res Rev 2020;12(18):136-141.
22.Paludetti G, Ottaviani F, Fetoni AR, Zuppa AA, Tortorolo G. Transient evoked Otoacoustic emissions (TEOAEs) in newborns: normative data. Int J Pediatr otorhinolaryngol 1999;47(3):235-241.
23. Zhao W, Zhong Z, Xie X, Yu Q, Liu J.Relation between chest CT findings and clinical conditions of Coronavirus disease (COVID-19) pneumonia: a multicenter study. Am J Roentgenol 2020;214(5):1072-1077.
24. Ramasamy K. The War of United States of America with COVID-19. Int J Cur Res Rev 2020;12(16):18-28.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License