IJCRR - 13(3), February, 2021
Pages: 83-87
Date of Publication: 03-Feb-2021
Print Article
Download XML Download PDF
Oral Health Conception in Parents of Indian Cerebral Palsy Children: A Self administer Questionnaire Study
Author: Sanat Kumar Bhuyan, Ruchi Bhuyan, Sidhant Bhuyan, Akankshya Sahu
Category: Healthcare
Abstract:Introduction: Special child are at high risk of chronic physical, developmental, behavioural conditions and they necessitate more amount of oral health treatment required by normal children. Objective: To evaluate the oral health conception Amida carers of cerebral palsy(CP) children. Methods: A self-administered questionnaire study of 99 carers of CP children's were registered. The survey was conducted in SVNIRTAR Olatpur, Cuttack, Odisha, India. Questions based on sociodemographic and conception and attitudes of carers towards oral health care. Results: The mean age of the carers was 40 years. 57.6% were female and mothers of the CP children. 42.4% were female and 33.3% of them were fathers of the children. The major oral health issues were bad breath (62.6%), decayed (64.6%), missing (60.6%), filled (56.6%), malocclusion (70.7%), and the severity of cerebral palsy Class I-III was seen in 74.7% of the children followed by Class IV-V in 25.3%. 32.3% were communicated verbally, 64.4% were non-verbally and 3% had no effective communication. 57.6% had poor oral health followed by 36.4% had moderate and 6.1% had good. Clinical treatment need revealed was an extraction of permanent teeth (50.5%), followed by filling (30.3%), pulpotomy and sealants primary teeth were 4% each, space maintenance (3%), fluoridation (2%), extraction of primary teeth (1%), all of the above treatment (3%) and no treatment required (2%). 66.7% of carers thought their children had medical problems where 33.3% thought oral health issues. Around 89.9% of carers used a toothbrush to clean the teeth where only 2% used an electrical brush and 8.1% used their fingers. Conclusions: Creating awareness among carers about tooth brushing and other factors and to make dental treatment more accessible may help to upgrade the oral wellbeing of special care needs children.
Keywords: Carers perception, Oral health, Dental treatment, CP children
Full Text:
INTRODUCTION
Knowledge frames the basis for most human activities and practices; and those with a better degree of information are relied upon to making more suitable conclusions and practices. Parents play a vital role in giving knowledge to their kids and the development of their habits and practices associated with good health. This is imperative in the case of mentally and physically challenged children, where parents take the maximum decision for them including both dietary habits and oral hygiene. Oral health is defined by one’s general health, as it influences someone’s capability to sense taste, smell, touch, chew, swallow, bite, speak, and smile.1 Child with special health care needs (CSHCN) has a high risk of chronic physical, developmental, behavioural conditions and they necessitate more amount of oral health treatment required by normal children.2 Generally CSHCN has poor oral status and dental caries, periodontal diseases, decayed teeth, missing teeth, delayed of both primary and permanent teeth, etc are frequently seen in this group of children.3
Cerebral palsy (CP) is a neurodevelopmental condition including a bunch of imperishable disorders of movement and position which affects the normal activity of the developing brain of an infant.4It is a non-progressive and non-communicable disorders5to be found in around 2-2.5 per 1000 live births.6 There is a high commonness of orofacial motor dysfunction of CP, which is normally created disturbances in sensation, communication, behaviour, and perception of CP patients and also children with CP be affected by multiple issues and various probable disabilities including mental health problems, difficulties in feeding, losses hearing and weakvisualization.4
Evidence is insufficient worldwide about the oral wellbeing conception in carers of CP children. In speedily changing socioeconomic situations; continuously observing and evaluating the CP carers regarding oral wellbeing conception is more essential in the present date. The objective of this survey is to assemble the most recent data on the oral wellbeing knowledge of CP patients carers and also raise awareness among their parents towards pediatric dental care and treatment.
MATERIALS AND METHODS
The survey was a self-administered questionnaire and managed to gather suitable details about CP patients and their carers. The survey was conducted by inSVNIRTAR Olatpur, Cuttack, Odisha, India. Ethical clearance was obtained from the institutional ethics committee. Carers of all CP patients enrolled in the centre and each carer was given an information sheet. Awareness of dental hygiene and dental caries management and different aspect of oral and dental health would be evaluated. The data obtained were recorded in an MS Excel sheet and a comprehensive analysis was done and results were formulated.
RESULTS
Demographic characteristics
The study population comprised of 99 carers of CP children and the outline of involved carers is given in Table 1. The mean age of the carer was 40 years and half of the carers were in between 30-50 years. 57.6% of the carers were female where 42.4% were male and all-female were mothers of the children. Of these male parents, 33.3% were fathers of the children, 5.1% had any other relation and 4% had no family relationship with the children.
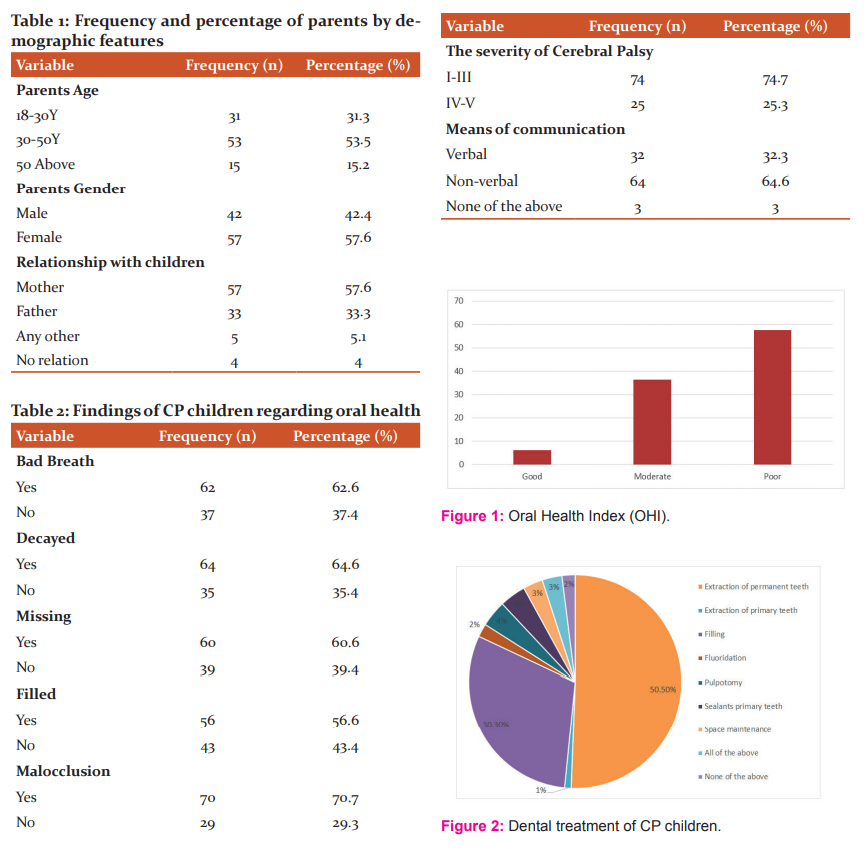
Some characteristics of CP patients are described in Table 2. The most frequent oral health issues were bad breath (62.6%), decayed(64.6%), missing (60.6%), malocclusion (70.7%), and the severity of cerebral palsy i.e. Class I-III was found in 74.7% of the kids followed by Class IV-V in 25.3%. While 32.3% were communicated verbally, almost 64.4% were non-verbally and 3% had no effective communication. Non-verbal communication means communicated to the patients by some sign language, use of pictures and cards, or writing. Oral health index (OHI) of patients showed that 57.6% had poor oral health followed by 36.4% had moderate and 6.1% had good (Figure 1).
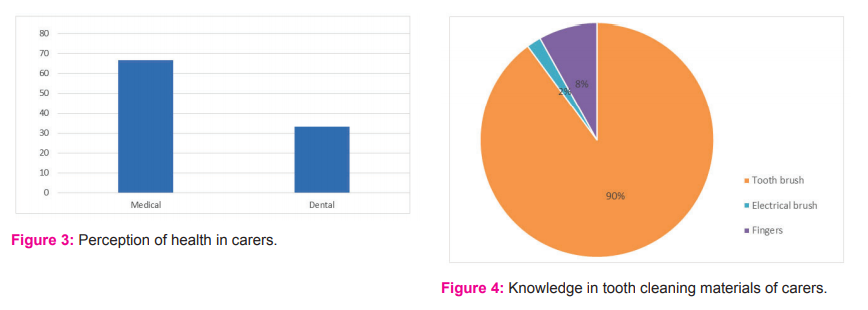
Consequently, the most frequent professed clinical treatment need revealing was the extraction of permanent teeth (50.5%), followed by filling (30.3%), pulpotomy and sealants primary teeth were 4% each, space maintenance (3%), fluoridation (2%), extraction of primary teeth (1%), all of the above treatment (3%) and no treatment required (2%) (Figure 2).
A greater percentage of carers considered that their CP patients had medical complications and dental problems. About 66.7% of carers thought that their children had medical problems where 33.3% thought oral health issues (Figure 3).
Tooth cleaning material is the most important aspect of CP patients. Picture 4 showed that approximately 89.9% of carers used a toothbrush to clean the teeth where only 2% used an electrical brush and 8.1% used their fingers (Figure 4).
DISCUSSION
CSHCN needs much care than normal children. They have poor oral health index, starting from nutrition to facial esthetics and overall physical as well as mental development. They are completely dependent on carers, whose attitudes and knowledge are much important in dispensing special care. In this survey, carers were dominatingly female and this finding is similar to the results of prior investigations on knowledge of carers.7,8,9 Due to this woman are remarked as primary carers of children.10,11
The major oral health problems were bad breath (44.6%) and decayed (64.6%) in this study, which is consistent with the previous study findings i.e. bad breath (44.6%) and decayed (33.6%).12 Furthermore we found 64.6% communicate non-verbally and 32.3% communicated verbally where 3% were non-communicated. A study by the Australian Research Centre for Population Oral Health reported that 21.3% communicated non-verbally while 30.3% had slight or no active communication.12
Pini et al. found Class I malocclusions in 48.9% with bad oral hygiene in 53.2% which is equivalent to this study.13 In this study we found 57.6% CP children with poor oral health hygiene. In the survey of 2011-2012 US National Survey of Children’s Health14, 84% of caregivers evaluated their children’s well-being as generally excellent while 84% of caregivers also evaluated their children’s well-being as generally excellent in the National Survey of Early Childhood Health.15 Another study by Daly et al. reported that 94% of parents rated their children’s health as excellent.1Abanto et al. reported that a lesser percentage of carers weighted their children’s oral wellbeing as super-excellent.16 In this study the Oral Health Index (OHI) of the CP children rated by their carers was found to be 57.6% as poor, 36.4% as moderate, and only 6.1% as good.
CP children are hard to handle and obstinate throughout the dental treatment and administration, so it is too challenging for dentists as it comprises of apprehension, fear from the unknown, and complications in communication.17 Effective communication should take attention while handling CP patients. CP children are abnormal in position and movement, so they need special seating and positioning adjustments. The dental chair should permit proper adjustment to give the CP patient constancy and support.17 Patients with more severity may allow treating on the parent's lap.18 Dentist should plan the appointment in the morning time to give enough period to CP’s parent for an appropriate interaction.19
Head position can be maintained in the midline by using Velcro straps and open mouth can be got by using mouth props.20 Steel mirror and finger guard are preferable to minimize the injury. Sharp instruments should be handled very cautiously to avoid any damage and injury.21 CP patients are face difficulties in rinsing mouth properly, so providing water spray and suction devices are necessary. If invasive procedures are needed then sedation and anaesthesia should give to patients for the treatment.22 Face or a nasal mask can be used in the mild case to prevent the nervousness and anxiety linked with IV supplement. Oxygen saturation must be checked by pulse oximetry and the airline must be guarded during procedures. Due to excessive salivation in CP patients and the use of water spray may increase the risk to swallow the dental materials used for the treatment, a throat shield must be used to defend the patient.23 The furthermost noteworthy aspect for effective treatment in CP children is the attitude and technique of dentists and the whole dental team.
The lack of awareness on the significance of oral wellbeing among carers is the reason for the severity of oral health conditions in children. Oral health disease co-exists with some disabilities and it is not measured as life-threatening by most of the populations. It is important to create awareness among carers and make intensive efforts to educate them regarding the consequence of dental wellbeing and the role it represents in over-all health.
CONCLUSION
The carers were not concern about the oral health problems which later affect the overall health conditions of the child and this might be due to a lack of awareness on the significance of oral wellbeing related to overall health status. The maximum number of the carers were not conscious about the deviancy in oral health and to treat it. So, creating awareness among carers about tooth brushing and other factors and making oral treatment more attainable may help to advances the oral wellbeing of CSHCN. The role of a pediatric dentist is more important to advances oral health problems and to cheer up the carers of CP children.
ACKNOWLEDGEMENT: We are thankful to the director of SVNIRTAR centre for allowing us to conduct the survey and data collection. We are also thankful to all parents and children for their cooperation in the study
Source of funding- None
Conflict of interest –None
References:
-
Daly JM, Levy SM, Xu Y, Jackson RD, Eckert GJ, Levy BT, Fontana M. Factors associated with parents’ perceptions of their infants’ oral health care. J Prim Care Comminity Health 2016;7(3):180-187.
-
Hegde AM, Shetty AA, Lolayekar N, Nair DJ, Nair HS. Prevalence of Malocclusion among Children with Special Health Care Needs and the Awareness of Their Parents towards Pediatric Orthodontic Care. J Adv Med Med Res 2018;6:1-7.
-
Altun C, Guven G, Akgun OM, et al. Oral health status of disabled individuals attending special schools. Eur J Dent 2010;4(4):361-366.
-
Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M, Damiano D, et al. A report: The definition and classification of cerebral palsy April 2006. Dev Med Child Neurol 2007;109:8?14.
-
Sehrawat N, Marwaha M, Bansal K, Chopra R. Cerebral palsy: A dental update. Int J Clin Pediatr Dent 2014;7:109?118.
-
Jan MM. Cerebral palsy: Comprehensive review and update. Ann Saud Med 2006;26:123?132.
-
Abanto J, Ortega AO, Raggio DP, Bönecker M, Mendes FM, Ciamponi AL. Impact of oral diseases and disorders on oral?health?related quality of life of children with cerebral palsy. Special Care Dentis 2014;34(2):56-63.
-
Baghdadi ZD. Effects of dental rehabilitation under general anesthesia on children’s oral health-related quality of life using proxy short versions of OHRQoL instruments. Sci World J 2014;5(1):41.
-
Kumar S, Kroon J. Lalloo R.,A systematic review of the impact of parental socio-economic status and home environment characteristics on children's oral health-related quality of life. Health Qual Life Outcomes 2014;12(1): 41.
-
American Psychological Association, 2015, Family caregiving, viewed 12 July 2015, from http://www.apa.org/about/gr/issues/cyf/caregiving-facts.aspx.
-
Hlabyago KE. Ogunbanjo GA. The experiences of family caregivers concerning their care of HIV/AIDS orphans. South Afr Fam Pract 2009;51(6), 506-511.
-
Pradhan A. Oral health impact on the quality of life among adults with disabilities: Carer perceptions. Austr Dent J 2013 Dec;58(4):526-530.
-
Pini DM, Frohlich PC, Rigo L. Oral health evaluation in special needs individuals. Einstein (Sao Paulo). 2016;14(4):501-507.
-
The Child and Adolescent Health Measurement Initiative. The National Survey of Children’s Health. 2011. http://childhealthdata. org/learn/NSCH. Accessed August 25, 2020.
-
Halfon N, Olson L, Inkelas M, et al. Summary statistics from the National Survey of Early Childhood Health, 2000. Vital Health Stat 2002;15(3):1-27.
-
Abanto J, Carvalho TS, Bönecker M, Ortega AO, Ciamponi AL, Raggio DP. Parental reports of the oral health-related quality of life of children with cerebral palsy. BMC Oral Health 2012;12(15):124-126.
-
Jan MM. Neurological examination of difficult and poorly cooperative children. J Child Neurol 2007;22:1209-1213.
-
Santos MT, Manzano FS. Assistive stabilization based on the neurodevelopmental treatment approach for dental care in individuals with cerebral palsy. Quintessence Int 2007;38:681-687.
-
Dean JA, Avery DR, McDonald RE, editors. Dentistry for the child and adolescents. 9th ed. Missouri (USA): Elsevier publication; 2011.
-
American Academy of Pediatric Dentistry. Definition of special health care needs. Pediatr Dent 2016;38:16.
-
Sehrawat N, Marwaha M, Bansal K, Chopra R. Cerebral palsy: A dental update. Int J Clin Pediatr Dent 2014;7:109?118.
-
Wongprasartsuk P, Stevens J. Cerebral palsy and anesthesia. Paediatr Anaesth 2002;12: 296-303.
-
Solomowitz BH. Treatment of mentally disabled patients with intravenous sedation in a dental Clinic outpatient setting. Dent Clin North Am 2009;53:231-242.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License