IJCRR - 13(2), January, 2021
Pages: 106-112
Date of Publication: 16-Jan-2021
Print Article
Download XML Download PDF
An overview of the Implant Therapy: The Esthetic Approach
Author: Kashish Mangal, Mithilesh M. Dhamande, Seema Sathe, Surekha Godbole, Rupali M. Patel
Category: Healthcare
Abstract:Many have mastered the skills of implant placement, but the art of rehabilitating the patient with anaesthetic prosthesis is the most important aspect of the treatment. While dealing with implants placed in the anterior region of the oral cavity in patients which in a way can be termed as the limelight area for esthetics, incorporating various factors for esthetics become imperative. This article aims to concise the majority of these factors under one umbrella. For this article, a thorough online search on this topic was carried out for collection and evaluation of available data. Before the surgery, the patient should be thoroughly evaluated using appropriate records like study models and necessary investigations like radiographs and CBCT scan should be obtained to assist in appropriate planning of the case. The patient's soft and hard tissue profile has to be evaluated, any discrepancy in which should be suitably addressed. After the pre-surgical evaluation, the technique of implant placement should be finalised by the patient's clinical conditions and requirements. The implant should be placed in an ideal manner to create near to natural esthetic profile. Any aberrations in the soft tissue occurring should also be anticipated and managed to reduce the number of surgeries required in the creation of the esthetic appearance. Once the placement has been done a suitable abutment should be selected and the entire focus should be given to creating a natural emergence profile for the future implant prosthesis. The result should be a natural life-like esthetic profile of the patient.
Keywords: Implant esthetics, Provisionalization, Emergence profile, Implant position
Full Text:
Introduction
With the increase in technological advancement, a good number of population has now become more aware regarding the available dental treatments and its importance. Not only this but the significance of teeth in the esthetics and appearance of a person has also been more accepted and understood by people. When a patient loses their anterior teeth, the most preferred option by patients has been fixed prosthesis because of various reasons out of which esthetics is prime.
Esthetics can be defined as “the theory and philosophy that deal with beauty and the beautiful, especially concerning the appearance of a dental restoration, as achieved through its form and/or colour; those subjective and objective elements and principles underlying the beauty and attractiveness of an object, design, or principle.1 This becomes truer when the clinician is dealing with the anterior zone which is the prime esthetic focal point of any person.
Dental implants were first introduced by Brånemark in the 1900s.2 Since then there have been countless advancements in this treatment modality ranging from its type, design, material as well as associated techniques. Currently, the market is flooded with a huge array of options available.3 A few of these have specifically been designed keeping the esthetic demands of the treatment.4-6 Though awareness in the population about implants as the preferred treatment is limited but the willingness to know more has been reported.9
Many have mastered the skills of implant placement, but the art of rehabilitating the patient with anaesthetic prosthesis is the most important aspect of the treatment. Detailed information regarding managing the anterior esthetics specifically for implant-retained fixed dental prosthesis [FDP] is relatively less. The existent difference between natural teeth and a dental implant governs various factors which need an additional consideration of anterior implant-retained FDP.2,10,11 This article deals with the implant esthetics and factors associated with it while specifically dealing with the anterior zone. For ease of clinical correlation and understanding, three different phases of the treatment have been identified with their respective imperative factors to be considered for optimum implant esthetics (Table 1).
Pre-Surgical Phase
When a patient enters the clinic with the expectation of rehabilitating his lost anterior teeth, the best treatment that can be given to him starts with an impeccable treatment planning before implant placement. It includes –
Study Model Evaluation
The study models in any and every prosthodontic treatment are indispensable. These important diagnostic tools enhance the predictability of the treatment & enabling proper treatment planning with a 3D working representation of the patient to the clinician.13 This overall visualization of the patient’s oral cavity helps in planning a holistic treatment for the patient.
The analysis of obtained models can give the clinician a wide range of information including the occlusal & arch relation, interarch space, number & position of adjacent teeth, appreciation of the edentulous ridge as well as planning of future implant placements to be done.
Radiographic Evaluation
Bone quality governs the success of implants. It is a primary factor in successful osseointegration of implants. Before the decision of implant placement is made, it is always imperative to assess the bone condition in which the said treatment is planned to estimate the prognosis. This bone quality is assessed with the help of roentgenographs or radiographs.
With the help of Cone Beam Computed Tomography (CBCT), we can now have a very accurate idea of the bony conditions which the clinician might encounter.14,15Software these days come along with additional features of assessing the Hounsfield units of the imaged bone which when compared with the Mischclassification for bone can give a precise idea for the prognosis of the treatment.9,10
Soft & Hard Tissue Evaluation
Esthetics is a harmony which exists between the teeth and its surrounding hard and soft tissues. Therefore, assessment of the adjacent structures is also necessary. Firstly, the gingival biotype i.e. thickness of the gingiva in faciopalatal/ faciolingual direction is to be assessed. It can be divided into two types- thin and scalloped or thick and flat. When the gingiva measures less than 1.5mm it is deemed as thin and scalloped biotype and when it has a dimension more than 2mm it is called thick and flat. Normal thickness of gingiva ranges from 1.5-2 mm. An unfortunate chance of visibility of an unesthetic titanium ‘shadow’ may be seen with thin biotype along with increased vulnerability for gingival recession. Thus, various esthetic prosthetic implant options like esthetic abutments or different implant placement technique or varied implant design might be considered.
Secondly, an assessment of the keratinized band of gingiva has to be made. A minimum requirement of 2 mm has been suggested for optimum peri-implant esthetics. Thirdly, the available bone height and width has to be checked in absence of which various grafting and augmentation techniques like vertical augmentation, en bloc grafting, particulate grafting, distraction osteogenesis. might have to be employed.16,17
Surgical Phase
Under this head, first comes the evaluation of best possible esthetic implant placement modality. After it, the ideal implant placement has to be ensured by the implantologist following which comes the management of soft tissue.11,12
Available Treatment Modalities
The ultimate aim of a treatment offered by any dentist is to give the patient the best possible results. With the inputs of various creative and great minds over the years, now we have a variety of treatment modalities to choose from as per the patient’s requirement. The two modalities which stand out in this are – Guided implant surgery and Immediate implant placement. These both techniques have been advised and reported with better results when dealing with implant placement in the patient’s esthetic zone.
Both of these techniques work best when applied together but can also be employed separately. Guided implant surgery refers to implant placement with the help of a custom made surgical stent for the patient with the help of their CBCT scans and respective analysis made on the scan. The data is then processed via computer-aided designing and computer-aided manufacturing (CAD-CAM) machinery to fabricate a replica of the image assessment and planned implant. The most important advantage that this technique offers is the precise implant placement in the patient and thus optimum esthetics.18-20 Immediate implant placement works best when we are dealing with the anterior zone provided the appropriate method of temporization is used. This provides the patient with not only an immediate replacement and thus protect them from any social or personal awkwardness regarding edentulousness but also the extracted tooth provides optimum guidance for optimum implant placement.21,22
Ideal Implant Positioning
Another important factor to consider while ensuring the best possible esthetics for a patient is the appropriate implant placement. A faulty placement may not only lead to esthetic but also prosthetic complications.
-
Mesio-distal positioning
The implant should be placed with at least 1.5mm of the distance between the implant and adjacent teeth on each side. In cases of multiple implant placement, a minimum of 3mm inter-implant distance should be maintained (Figure 1).23
-
Labio-palatal positioning
This dictates the angulation at which the implant will be placed in the alveolar bone. The labio-palatal positioning holds utmost importance when dealing with anterior zone since it helps in developing the emergence profile of future implant prosthesis. The ideal positioning of the implant in this direction is advised to be following the facial contours of the adjacent teeth. A minimum of 1-1.5mm of buccal bone and 0.8mm of palatal bone should be spared while placing the implant (Figure 2). 24
Not only the amount of bone but the type of future implant prosthesis which is planned also dictates the labio-palatal positioning of the implant. It has been advised that if the prosthesis has to be cement-retained then the placement has to exactly in the centre of the long axis of the said prosthesis. When a screw-retained prosthesis is planned, the implant may have to be positioned slightly palatal to the long axis of the prosthesis to ensure palatal access to the screw channel. An improper implant placement or a too buccal placement may lead to inadequate buccal bone present to envelope the implant. This may further result in severe complications like dehiscence or fenestrations.11
-
Apico-incisal Positioning
An implant placed rightly in the axial or apical-incisal direction will give the clinician sufficient space to develop an adequate emergence profile for the future implant prosthesis. It has been suggested that the implant ideally should be placed 2-3mm apically to an imaginary line connecting the deepest portions or the zenith of gingival contours of the adjacent teeth. When the natural adjacent landmarks are missing and multiple implants are to be placed then the implant head can be positioned at the alveolar crest within the circumference of the tooth to be restored. The 2-3mm of pico-incisal distance will give the clinician sufficient space around the implant, otherwise called a running room, within which the contours of restoration can be developed (Figure 3).12-14
It is an obvious fact that the cross-sectional diameter of a natural tooth and the head of an implant has a huge variation. To compensate this & provide the patient with a near to natural esthetics, this running room is essential. In this, the clinician can gradually increase the bulk of material to create optimum peri-implant esthetics.15
Soft Tissue Management
As rightly said by Professor Dr. Jan Lindhe “The bone sets the tone, the soft tissue is the issue”, dealing with the peri-implant soft tissue for a complete esthetic appearance is of great significance. The major value here has to be given to the development of suitable interdental papilla, the absence of which may lead to the highly unesthetic black triangles. If the implant were to be placed appropriately in its apical-coronal direction, then according to Tarnow, with 5mm of the distance between the crest of the bone and contact point of teeth and prosthesis should observe a 100% papilla fill. As the distance increases a reduction in papillary fill is observed which may further complicate the situation and require surgical or prosthetic intervention for correction.25–28
Post-surgical Phase
After the implant has been placed, and it is the time for restoration, the post-surgical management of implant esthetics come into the picture. In this, the primary focus will be on professionalization, development of emergence profile, abutment selection followed by the definitive prosthesis and follow-up.
-
Provisionalization
Provisionalization or temporisation refers to rehabilitating the patient with a short-lived treatment option until definitive restoration can be put into its place.29 They help not only in improving the quality of life for the patient undergoing implant therapy by enhancing his esthetics but also serves as a template for designing the definitive prosthesis. The provisional prosthesis can be given soon after the tooth extraction or during the socket healing and site development. It can also be utilized before implant placement or during the phases of osseointegrationor after the second stage surgery. In such case, the provisional prosthesis will help in supporting the soft tissue to build an appropriate emergence profile and help in assessment of esthetics and phonetics prior to fabrication of the definitive restoration.30
Broadly, provisional restorations can be classified as removable or fixed. Under the umbrella of temporary prosthesis, the clinician has various options like an existing prosthesis that the patient already uses or a removable partial denture, a vacuum formed retainer, a chairside or laboratory made resin bonded bridge,conventional FDP, provisional prosthesis supported by immediately loaded transitional implants or implant-supported provisional prosthesis. The choice of provisional prosthesis should be made considering the type of treatment modality planned. For example, in cases where the surgical site has been modified with augmentation or grafting which necessitated a longer unhindered healing period, a provisional prosthesis which can withstand for the prescribed duration without hampering the healing and also enable modifications as and when required should be preferred. In cases of immediate implant placement, if an immediate temporary restoration/ prosthesis is planned, then it should be constructed such that support to the peri-implant tissue is provided. With this, the provisional prosthesis would help in preserving the already existing soft tissue curtain of the extracted natural tooth.4,30-31
-
Development of Emergence Profile
Emergence profile is the contour of the implant restoration as it emerges from the gingiva. Creating a natural emergence profile holds utmost importance in implant esthetics. This can be done with ideal/ optimum implant placement and usage of proper temporary restoration for the patient.32-33 In optimal intraoral conditions where no major corrective procedures are required, the provisional prosthesis can be employed for the creation of an almost natural emergence profile.30The temporary restoration aids by the virtue of its diameter which is gradually increased beneath the gingival envelope, in other words within the running room. If the apical-incisal positioning of the implant is faulty resulting in an inadequate running room, the emergence profile of the restoration may be compromised.
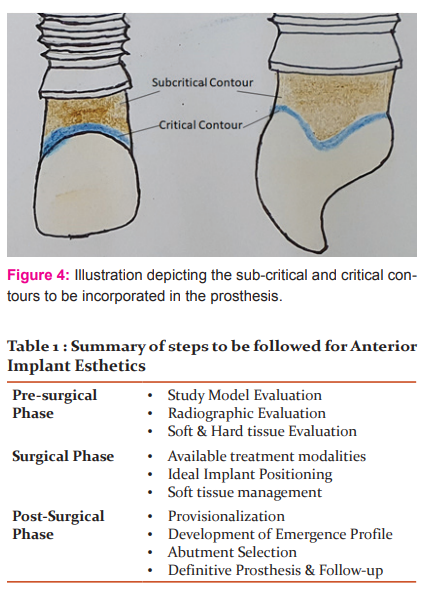
Every restoration within this running room should possess sub-critical and critical contours (Figure 4). These contours have to be incorporated in the prosthesis as per the requirement of the patient’s peri-implant conditions. Critical contour refers to the area of implant prosthesis and an underlying abutment which is immediately apical to the gingival margin of the restoration. The facial/labial profile of the critical contour plays a significant role in the location of the zenith of the associated gingival curtain which directly affects the apparent clinical length of the crown. Also, the interproximal profile of critical contour governs the shape of the prosthesis (triangular/ square). Modification in critical contour can affect the level of gingival zenithlabially.34
The second is sub-critical contour which exists only when an optimum running room has been given. This is the area of implant prosthesis which lies immediately coronal to the implant-abutment interface. Modification in the profile of this contour [convex, concave or flat] can have a significant effect on the overlying gingival envelope. If made convex it will support the gingival curtain, the concave profile may help in gaining increased tissue volume and in ideal conditions it can be maintained flat. The interproximal modification of this subcritical contour is said to help in enhancing the papilla fill inter proximally up to 0.5 – 1 mm.35
-
Abutment Selection
The future of the prosthesis depends on the type of abutment selected. Currently, numerous options are available for the clinician ranging from different materials to different angulations and types of retention. Based on the type of retention, screw or cement-retained abutments may be chosen. Both of them have respective pros and cons, but their selection is also relative to the implant placement and vice-versa as stated earlier. If the abutment screw channel arises on the labial aspect of the prosthesis, then it will require further management to create an esthetic appearance which may not be completely acceptable to the patient.
In cases where prior soft tissue evaluation was done and the patient had a thin gingival biotype with a high probability of a titanium shadow display, esthetic implant options will have to be considered.36 This is also true in cases whereas a result of improper implant placement titanium hue is visible. With the recent advances in biomaterials, there are diverse options available to handle such situations. These include Zirconia abutments, hybrid abutments, polyetheretherketone (PEEK) abutments etc.37-39
If the patient presents with an improperly placed implant or an implant with abnormal angulations, then utilization of angulated abutments or customized abutments may be required to fulfil the esthetic requirements of the patient. Variety of pre-angulated abutments are available with manufacturers these days ranging from 17 degrees to 35 degrees. But when the favourable esthetic profile cannot be established with the angulated abutments as well, the clinician might have to opt for customized abutments. Here, the options include castable abutments as well as the newer CAD-CAM abutments which widens the horizons with different biomaterials to be milled using various types of machinery for accurate fit and esthetics.34,40
Definitive prosthesis and Follow-up
The task of construction of anaesthetic definitive or final restoration for anterior implants becomes much easier when appropriate temporization has already been employed. This provisional restoration, after thorough assessment for esthetics which includes the creation of emergence profile, phonetics and function, could directly be replicated to form the definitive restoration. With the technological benefit of CAD-CAM, this provisional restoration can directly be scanned and a replica of the same can be obtained. This helps the clinician by eliminating the errors which might occur due to multiple impression, duplication and laboratory procedures.26
After the definitive prosthesis has been delivered, the patient can be evaluated for the esthetics and function imparted by the restoration by using various scales and indices available. With the help of such indices along with patient satisfaction and clinician’s evaluation, the success of prosthesis and thus the treatment can be verified and justified.
Conclusion
The rehabilitation of the esthetic zone by implant-retained FDP is one of the most demanding and complex treatments due to the necessity to obtain an optimum esthetic result. Through osseointegration, restoration of function and soft and hard tissue esthetics dictate implant success, the patient's satisfaction is a key element of the success of implant therapy. With the concurrent paradigm shift in the approach of dental implantology making it more prosthetically driven, the necessity of a synergistic harmonious interdisciplinary approach between implant placement, soft tissue management and the prosthetic rehabilitation holds the key towards a happy and satisfied patient and clinician. To achieve this, a treatment governed by the guidelines for esthetic rehabilitation, specifically designed for implant rehabilitation should be imparted to the patient. This article outlines these guidelines with details about their clinical implication to help clinicians decide the best treatment course for the patient.
Conflict of interest: Nil
Acknowledgment: Authors acknowledge the immense help received from the scholars whose articles are cited and included in references to this manuscript. The authors are also grateful to authors/editors/publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.
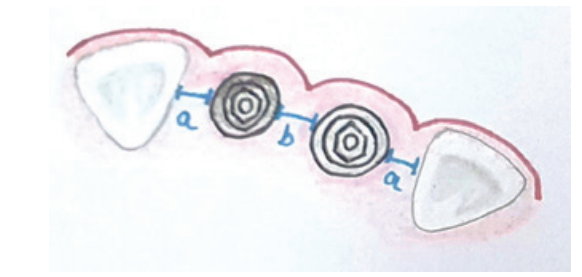
Figure 1 : Illustration showing mesiodistal positioning of implant. a= 1.5mm distance between implant and adjacent teeth; b= 3 mm inter-implant distance.
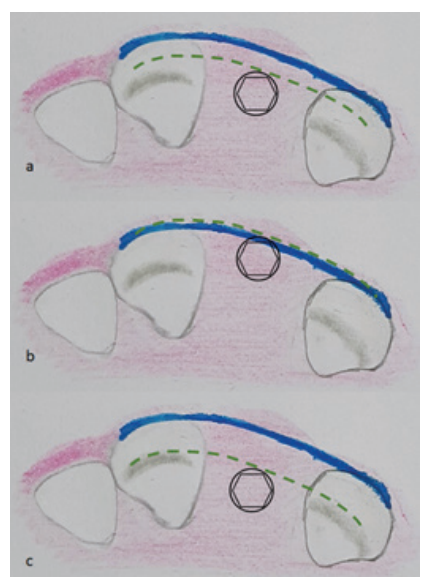
Figure 2: Illustration showing labio-palatal positioning of the implant. The green line denotes the level of implant head, the blue line represents the natural labial contour of natural teeth. a) Optimum space is present between the implant head and tooth contour whereas in b) implant is placed too close to the buccal contour and c) too much distance exists between the labial contour and implant making it difficult to rehabilitate with good esthetics.
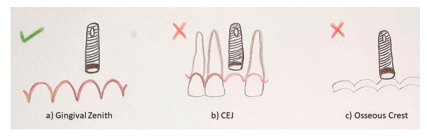
Figure 3 : Illustration depicting correct apico-coronal implant position. Ideally it should be placed 2-3mm beneath the gingival zenith to allow for adequate running room for prosthetic build-up.
References:
1. Ferro KJ. The Glossary of Prosthodontic Terms 9. J Prosthodont 2017 May;
2. Rajput R, Chouhan Z, Sindhu M, Sundararajan S, Chouhan RRS. A Brief Chronological Review of Dental Implant History. Int Dent J Stud Res 2016 Oct;4(3):105-107.
3. Hong DGK, Oh J. Recent advances in dental implants. Maxillofac Plast Reconstr Surg. 2017 Dec;39(1):33.
4. Kan JYK, Rungcharassaeng K, Liddelow G, Henry P, Goodacre CJ. Peri-implant tissue response following the immediate provisional restoration of scalloped implants in the esthetic zone: A one-year pilot prospective multicenter study. J Prosthet Dent 2007 Jun;97(6): S109–118.
5. Starch-Jensen T, Christensen AE, Lorenzen H. Scalloped Implant-Abutment Connection Compared to Conventional Flat Implant-Abutment Connection: a Systematic Review and Meta-Analysis. J Oral Maxillofac Res 2017;8(1).
6. Wöhrle PS. Nobel Perfect? Esthetic Scalloped Implant: Rationale for a New Design. Clin Implant Dent Relat Res 2003;5(s1):64-73.
7. McAllister BS. Scalloped Implant Designs Enhance Interproximal Bone Levels. Int J Periodontics Restorative Dent 2007;27(1):9-15.
8. Gadhia MH, Holt RL. A New Implant Design For Optimal Esthetics and Retention of Interproximal Papillae. Implant Dent 2003 Jun;12(2):164-169.
9. Revankar RP, Sathe S, Borle AB, Godbole S, Pande S, Khungar P. Evaluation of Knowledge, Attitude and Awareness of patients regarding dental implants in Central India. Int J Dent Sci Innov Res 2019 Jun;2(3):285–291.
10. Misch CE. Dental Implant Prosthetics. 2nd ed. Elsevier Mosby; 2015:46–65.
11. El Askary AES. Advances in Esthetic Implant Dentistry. 3rd ed. Wiley Blackwell; 2019.
12. Prem R, Acharya BG, Mathews J, Ambadas, Jagtap P, Bhavsar B. Indications for dental implant treatment- A clinician’s point of view. Int J Curr Res Rev 2014 Nov;6(21):29–33.
13. Hupp JR. Introduction to Implant dentistry?: A student guide. J Oral Maxillofac Surg 2017 Feb;75(Supplement 2):106.
14. Diwakar NR, Kamakshi SS. Recent advancements in dental digital radiography. Nagaraj T, editor. J Med Radiol Pathol Surg 2015;1:11-6.
15. Jayachandran S. Digital imaging in dentistry: A review. Contemp Clin Dent 2017;8(2):193.
16. Ferrari M, Carrabba M, Vichi A, Goracci C, Cagidiaco M. Influence of Abutment Color and Mucosal Thickness on Soft Tissue Color. Int J Oral Maxillofac Implants 2017 Mar;32(2):393–399.
17. Agrawal DR, Jaiswal P. Different Techniques of Harvesting Connective Tissue Graft: An Update. Int J Curr Res Rev 2020 Aug;12(15):16–25.
18. Motta M, Monsano R, Velloso GR, de Oliveira Silva JC, Luvizuto ER, Margonar R, et al. Guided Surgery in Esthetic Region: J Craniofac Surg 2016 May;27(3):e262–265.
19. Fürhauser R, Mailath-Pokorny G, Haas R, Busenlechner D, Watzek G, Pommer B. Esthetics of Flapless Single-Tooth Implants in the Anterior Maxilla Using Guided Surgery: Association of Three-Dimensional Accuracy and Pink Esthetic Score: Esthetics of Guided Flapless Single-Tooth Implants. Clin Implant Dent Relat Res 2015;17:e427–433.
20. Kulkarni PN, Bulbule NS, Kakade DM, Hakepatil NV. Radiographic Stents and Surgical Stents in Implant Placements: An Overview. Int J Curr Res Rev 2019 Jun;11(2):11–5.
21. Agarwal DS, Devkar ND, Vibhute AR, Walke PD. Immediate Placement of Dental Implants: An Overview. J Dent Allied Sci 2018;7(2):5.
22. Bhola M, Jacobs L, Kolhatkar S. Immediate implants for aesthetic success: New guidelines. J Int Clin Dent Res Organ 2015;7(3):138.
23. Higginbottom F, Belser U, Jones JD, Keith SE. Prosthetic Management of Implants in the Esthetic Zone. Int J Oral Maxillofac Implants 2004;19 Suppl:62-72.
24. Batra R, Kalra S, Batra H. Implant esthetics. Indian J Dent 2012 Jan;3(1):15–20.
25. Ishikawa T, Salama M, Funato A, Kitajima H, Moroi H, Salama H, et al. Three-Dimensional Bone and Soft Tissue Requirements for Optimizing Esthetic Results in Compromised Cases with Multiple Implants. Int J Periodon Restor Dent 2010;30(5): 23-26.
26. Tarnow D, Elian N, Fletcher P, Froum S, Magner A, Cho SC, et al. Vertical Distance from the Crest of Bone to the Height of the Interproximal Papilla Between Adjacent Implants. J Periodontol 2003 Dec;74(12):1785–1788.
27. Tarnow DP, Magner AW, Fletcher P. The Effect of the Distance From the Contact Point to the Crest of Bone on the Presence or Absence of the Interproximal Dental Papilla. J Periodontol 1992;63(12):995-996.
28. Lambodharan R, Balaji V. Interdental papilla regeneration around implants: A novel window technique (2 years follow-up). J Pharm Bioallied Sci 2015;7(6):815.
29. Guirado JLC, Yuguero MRS, Zamora GP, Barrio EM. Immediate provisionalization on a New Implant Design for Esthetic Restoration and Preserving Crystal Bone: Implant Dent 2007 Jun;16(2):155–164.
30. Wang WC, Hafez TH, Almuflh AS, Ochoa-Durand D, Manasse M, Froum SJ, et al. A Guideline on Provisional Restorations for Patients Undergoing Implant Treatment. J Oral Biol 2015;2(2):7.
31. Santosa R. Provisional restoration options in implant dentistr. Aust Dent J 2007 Sep;52(3):234–242.
32. Daniel D, Manuel D. Creating emergence profiles in immediate implant dentistry. 2018:8.
33. Kutkut A, Abu-Hammad O, Mitchell R. Esthetic Considerations for Reconstructing Implant Emergence Profile Using Titanium and Zirconia Custom Implant Abutments: Fifty Case Series Report. J Oral Implantol. 2015;41(5):554–561.
34. Chu SJ, Kan JYK, Lee E, Jahangiri L, Nevins M. Restorative Emergence Profile for Single-Tooth Implants in Healthy Periodontal Patients: Clinical Guidelines and Decision making Strategies. Int J Periodon Restor Dent 2017;2(7):327-329.
35. Su H, Gonzalez-Martin O, Weisgold A, Lee E. Considerations of Implant Abutment and Crown Contour?: Critical Contour and Subcritical Contour. Int J Periodon Restor Dent 2015; 5(2):429-431.
36. Zaraus C, Pitta J, Pradies G, Sailer I. Clinical Recommendations for implant abutment selection for Single- Implant Reconstructions: Customized vs Standardised ceramic and metallic solutions. Int J Periodont Restor Dent 2017; 6(2): 347-351.
37. Ramenzoni LL, Attin T, Schmidlin PR. In Vitro Effect of Modified Polyetheretherketone (PEEK) Implant Abutments on Human Gingival Epithelial Keratinocytes Migration and Proliferation. Materials 2019 Apr;12(9):1401.
38. Chen J-Y, Pan Y-H. Zirconia implant abutments supporting single all-ceramic crowns in anterior and premolar regions: A six-year retrospective study. Biomed J 2019 Oct;42(5):358–364.
39. Najeeb S, Zafar MS, Khurshid Z, Siddiqui F. Applications of polyetheretherketone (PEEK) in oral implantology and prosthodontics. J Prosthodontic Res 2015;4:182-7
40. Wu T, Liao W, Dai N, Tang C. Design of a custom angled abutment for dental implants using computer-aided design and nonlinear finite element analysis. J Biomech 2010;43(10):1941-1946.
41. Fürhauser R, Florescu D, Benesch T, Haas R, Mailath G, Watzek G. Evaluation of soft tissue around single-tooth implant crowns: the pink esthetic score: Esthetic score. Clin Oral Implants Res 2005;16(6):639-644.
42. Belser UC, Grütter L, Vailati F, Bornstein MM, Weber HP, Buser D. Outcome Evaluation of Early Placed Maxillary Anterior Single-Tooth Implants Using Objective Esthetic Criteria: A Cross-Sectional, Retrospective Study in 45 Patients With a 2- to 4-Year Follow-Up Using Pink and White Esthetic Scores. J Periodontol 2009 Jan;80(1):140-151.
43. Torsten J. Regeneration of Gingival Papillae After Single-Implant Treatment. Int J Periodont Restor Dent 1997;17(4):327-333.
44. Cosyn J, Eghbali A, De Bruyn H, Collies K, Cleymaet R, De Rouck T. Immediate single-tooth implants in the anterior maxilla: 3-year results of a case series on hard and soft tissue response and aesthetics: Immediate single-tooth implants. J Clin Periodontol 2011 Aug;38(8):746-753.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License