IJCRR - 13(2), January, 2021
Pages: 80-84
Date of Publication: 16-Jan-2021
Print Article
Download XML Download PDF
Study of Bipolar Hemiarthroplasty of Hip Joint in Rural Teaching Set Up
Author: Jainish Patel, Munir Upadhyay, Aditya K. Agrawal, Prasanna Shah, Yash Mutha, Paresh Golwala
Category: Healthcare
Abstract:Background: With increasing orthopaedic expertise in the rural centres, there has been the development of tertiary care centres in rural areas wherein a high-end surgery such as hip joint replacement can be done. Bipolar hemiarthroplasties, performed at rural teaching set up are evaluated for comparison of similar surgeries performed at sophisticated, high-end corporate hospitals. Objective: To compare outcome at the rural teaching setup, with large series at a high-end teaching or corporate hospitals from published literature. It also would enable us to recognize short-comings at tertiary teaching set up in rural areas, and innovation to circumvent these shortcomings and evaluate and access the benefits of these alternative resources and innovation for a better bipolar hip arthroplasty outcome. Methods: In the present study 30 cases of bipolar hemiarthroplasty were taken. Clinical outcome and functional results were evaluated by using the Harris hip score. Results: Out of 30 cases 11 were females and 19 males. With most common indicators are fracture neck femur and avascular necrosis of femoral head where the acetabular surface was not involved. We have evaluated the functional outcome by Harris hip score at the final follow up period. We have achieved 80% of excellent results as the functional outcome of the patient. Conclusion: The clinical and functional outcome of Bipolar hemiarthroplasty done at our rural teaching set up, with experienced surgeons, adequate manpower etc. are comparable to the high end sophisticated established urban teaching centres and corporate hospitals. We have used Harris Hip Score to analyze the results and 90% had good results.
Keywords: Bipolar Hemiarthroplasty, Harris Hip Score, Fracture neck femur, Avascular necrosis of femoral head, Clinical and functional outcomes, Hip prosthesis
Full Text:
INTRODUCTION
The incidence of a Joint Replacement Surgery has increased exponentially over the past few decades. There is a surge in joint replacement surgery in the last few decades across all developing countries due to increased longevity of life and an increasingly ageing population. India the second-most populous country in the world can be broadly divided into two groups, one residing in urban and the other in rural areas. Till recent times, hip joint replacement surgeries were restricted to urban areas with well-equipped state of the art hospitals and experienced trained surgeons. However, with increasing orthopaedic expertise in rural centres, there has been the development of tertiary care centres in rural areas wherein such a high-end surgery can be done. These tertiary care teaching centres where good manpower is available but still improving in development of high-end infrastructure like modular operating units. The literature has shown predictable, consistent, and reproducible results following replacement surgeries, but all these studies were done in highly sophisticated and well-equipped hospitals.
Not all the patients have the extensive deformities of both the femoral head and acetabulum, for which a dual-assembly total hip prosthesis is required. In some patients, then, it would appear appropriate to make use of a system that embraces the low friction principle, but yet does not require removing or distorting the acetabulum, which, in a good number of cases does not need to have a total hip replacement. This led to the development of "bipolar" type of hip replacement, the credit for which goes to James E. Bateman.1 Modular hip systems provide not only for the selection of the various sizes of the stem but now also allow independent sizing of various portions of the head and neck.
This single assembly type of unit is well tolerated within the body, and clinical progress has been most encouraging. Patients walk early and without pain and a high degree of stability has been maintained. Therefore, this study of hip replacement surgeries which is bipolar hemiarthroplasty, performed at our teaching hospital in a rural setup was undertaken. This would enable us to compare outcomes at the rural teaching setup, with large series at high-end teaching or corporate hospitals from published literature. This will allow us to rectify short-comings at tertiary teaching set up in rural areas, and innovation to circumvent these shortcomings and evaluate and access the benefits of these alternative resources and innovation for a better outcome of bipolar hip arthroplasty.
MATERIAL AND METHODS
The present study was carried out in the department of orthopaedics with approval obtained before the study from the Ethical Committee of the institute (SVIEC/ON/MEDI/BNPG13/14507). This study includes patients who underwent bipolar hip joint hemiarthroplasty surgery at the Department of Orthopedic Surgery. The inclusion criteria included patients with fracture neck femur and avascular necrosis of femoral head willing to participate in the study, all cases of bipolar hemiarthroplasty surgery irrespective of gender and medical condition of the patient. The exclusion criteria included short term follow-up cases of surgery less than six months and patients not willing for study. The statistical analysis was done using SPSS software (Illinois, Chicago) and p-value less than 0.05 was considered statistically significant.
All the patients in our study were admitted in the outpatient department or casualty. A detailed history is taken and specific evaluation was done regarding life expectancy, incurable disease, general condition to tolerate the elective procedure. X-rays of the pelvis with both hips was done. In AVN patients MRI was done. After all preoperative investigations and pre-anaesthetic check-up, the patient was taken to OT. All surgeries were performed under full aseptic condition and in laminar airflow theatre. The patients were kept in the lateral position and surgery was performed by posterior Moore’s approach. Patients were followed up for a longer duration from 6 months up to 3 years. On follow up the patient was evaluated according to Harris hip score for clinical and functional outcome. Under normal circumstances, static and active quadriceps exercise and ankle pump were begun on the same day within the comfort followed by high sitting on the second postoperative day.
Patients were mobilized depending upon the advice of the surgeon and compliance of the patient to follow our advice. Patients who underwent cemented hemiarthroplasty were advised weight bearing as soon as pain permits whereas in uncemented hemiarthroplasty we initiated weight-bearing between 4 weeks to 5 weeks. Patients were instructed not to squat, sit cross-legged or indulge in active sports and advised to use western-style toilets.
RESULTS
In the present study, we studied 30 cases of operated bipolar hemiarthroplasty (24 uncemented + 6 cemented). The primary aim of the study was to critically evaluate the results regarding clinical, radiological and functional parameters.
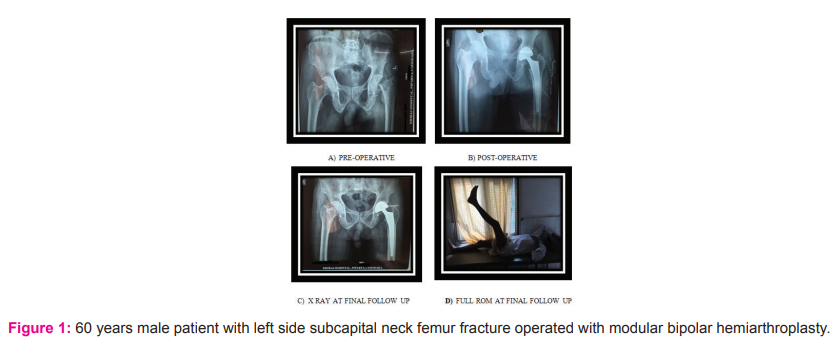
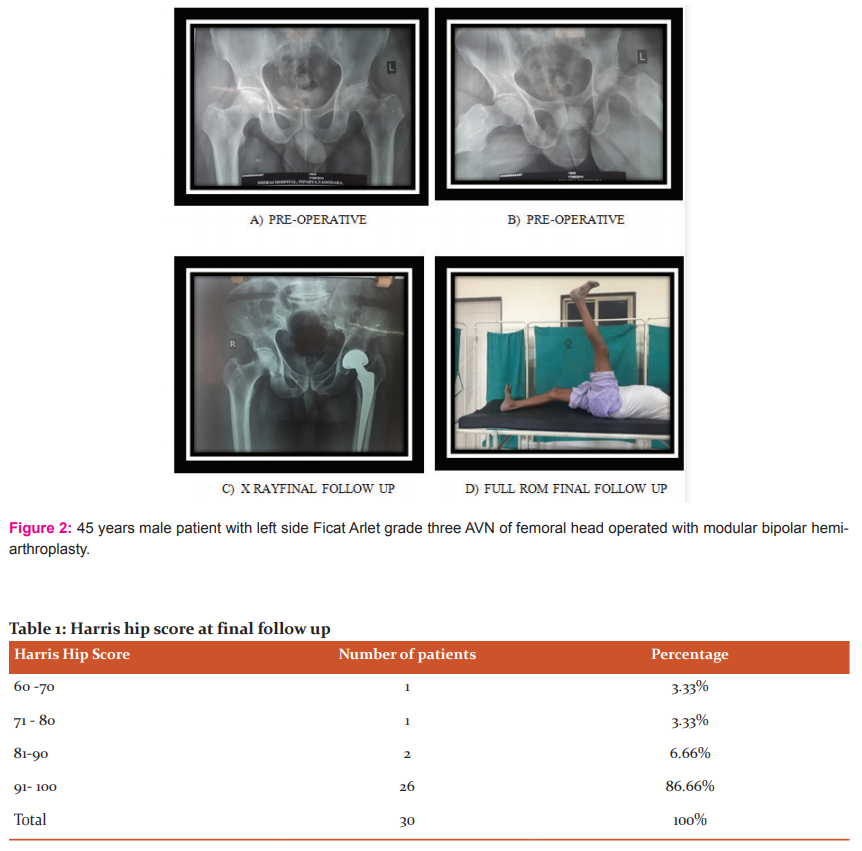
In our study, the age group ranges from 25 – 81 years, among them 8 patients were among 35 – 44 years age group and second common age group were 65 – 74 years. In our study male to female ratio was 2:1.In this study, we included 15 patients of fracture neck femur and 15 patients of AVN (3 patients grade2 & 12 patients grade3FicatArlet). In our study 43.4% of patients were heavy worker which were mainly farmers and labourers, 30% were moderate worker mostly females (housewife), 26.6% were lightworker (shop keeper).In our study, 1 superficial infection and 1 dislocation were noticed which was managed by debridement and close reduction respectively.
We had started weight-bearing walking among 6 patients of cemented bipolar within a week of surgery according to patients’ compliance. 26 patients of uncemented bipolar were made to walk after 1 month of surgery and 2 patients were made to walk after 45 days of surgery due to complication and persistent pain, both of them were walking with limp. Among all patients, 28 patients could walk more than 1 km without pain. 2 patients had limb length discrepancy (one with shortening of one cm compensated with shoe raise on the affected side and one with lengthening of one cm compensated with shoe raise of the unaffected side). On a series of X-ray evaluation, it was found that three patients had trochanteric osteoporosis on long term follow up while 27 patients did not show any limb length discrepancy. The outcome was evaluated according to Harris hip score and results were with good to excellent results in 93.32 % cases as shown in Table 1. So, 28 patients had satisfactory outcome and 2 patients had a fair outcome. All patients were able to return to work except one.
DISCUSSION
The joint replacement surgeries have surged exponentially over the past decade due to increased longevity of life and increasing ageing population. Most of the patient who underwent this surgery belonged to urban and economically well of population. However with an increase in economic development and penetration of insurance facilitates in the rural area and increased longevity of life, there is a sharp increase in the incidence of joint replacement surgeries in rural population.
Generally, good clinical results have been reported with the use of bipolar prosthesis and its current indications have expanded to include: The primary surgical management of non-infective hip joint arthritis secondary to avascular necrosis, rheumatoid arthritis, ankylosing spondylitis, osteoarthritis and in fresh, pathological, iatrogenic, and non-union femoral neck fractures. Bipolar prosthesis confers following advantages over a conventional Austin Moore's prosthesis like wide range of movements, intrinsic stability at two bearing interfaces thus, reducing the chances of dislocation of the hip, decreased incidence of complications like acetabular erosion, protrusion acetabuli, femoral stems loosening, increased longevity of the prosthesis.
However, there are certain shortcomings in rural areas like no high tech hospitals, lack of expertise (super specialist joint replacement surgeons are not available). These joint replacement surgeries are limited to urban corporate hospitals and patient need to travel a long distance from their residence to urban area for surgery. This lead to infrequent, inadequate follows up due to the long distance of travel and expense involved for a visit to the urban centre. But with increasing orthopaedic expertise there has been the development of tertiary care teaching centres in rural areas wherein such a high-end surgery can be done. These centres have the infrastructure and technically skilled manpower with experienced surgeons.
We have studied 30 cases of bipolar hemiarthroplasty at tertiary care hospital. These cases were compared with studies conducted by other authors done at sophisticated urban centres, where there is no constrain of material and money. Various aspects of the procedure have been observed and discussed in detail. The average age of the patients was 52.76 ± 8.5 years, with a range of 25 to 85 (CI 95%). Majority of the patients were in the age group 35 – 44 years & the second common group was 65-74 years. The average age varies from 54 to 80 years in varius studies conducted previously.1-5 The common age incidence in my study is less as compared to the reported series probably due to the young patients suffering from AVN of the femoral head (acetabulum is not involved), we did bipolar hemiarthroplasty as the life expectancy of these patients are not that high as they are having sickle cell disease. This will give them good functional hip throughout their lifetime. As common age group in AVN cases is 35-44years with the average age of 39.4yrs. In fracture neck of femur, the average age is 66 years ranging between 65-74 years.
In this series, it was observed that out of the 30 patients 11 were female (36.7%) and 19 were male (63.3%). In the literature, a lot of variation is reported, female being more common than male. Percentagen of females in diferent studies was in the range of 80-90%.3-5 Fracture neck is common in older females due to hormonal imbalance in the postmenopausal age and associated osteoporosis. However, in this study males were predominant as compared to females. This is probably due to the high incidence of younger patients with AVN and more males are venerable to RTA.
Out of thirty patients, fifteen cases were of avascular necrosis of femoral head, of which three were due to sickle cell disease, one was due to long term use of steroid (asthmatic), three were alcohol-induced and in rest eight cause of AVN could not be detected. All cases were grade 2 or 3 according to Ficat Arlet classification. We did bipolar arthroplasty in some grade 2 because of less possibility of reversal of AVN by other methods or surgery as in sickle disease and a case of steroid-induced AVN where the patient can’t discontinue steroid due to severe asthma.
The majority of patients had no complication that was 28 patients (93.33%). One patient was noticed with the infection that was treated with debridement and appropriate antibiotics given according to the culture and sensitivity of discharge. And 1 patient (3.3%) had dislocation which was treated by close reduction and traction in abduction and de-rotation bar for 3 months. In the published series, the infection rates were 2.8% and 2.1%.3,5. Nottage and McMaster reported wound breakdown in 3.9%, deep wound infection was 3.9% and superficial in 3.33% which is comparable to our series.6 A dislocation rate of 2.4% si also observed by Lesrange, 1900. Our results are quite similar to the published series.
In Nottage and Mc Master6 one patient (3.33%) developed deep vein thrombosis after 7th day, which was treated successfully with S/C heparin after monitoring PT and PTT. Even though we have not used prophylactic anticoagulants, we have not encountered any thromboembolic phenomena like deep vein thrombosis probably due to the early mobilization of the patients. In this series study the average Harris Hip Score is 89.43 outcome was an excellent result in 24 (80%) patients, a good result in three cases(10%), fair in one case (3.3 %) and poor in two cases 6.6%.
In the reported series of Giliberty7 had 92% satisfactory results with a mean Harris hip score of 84.81 points, Mannarino et al.8 had mean Harris hip score of 84.7 points, Lausten et al.9 found 75% excellent to good results, Lestrange5 had 70.8% excellent to good results. Nottage and Mc Master (1990)6 had a mean Harris hip score of 83 in the bipolar group and Amite et al11 had 90.6% excellent to good results in bipolar and Marya et al.2 had excellent to good results in 85% while We have got 90% satisfactory results ( excellent results in 80% and good result in 10% of the cases) with an average Harris Hip Score of 89.43, which is quite similar to the above-mentioned series.
CONCLUSION
The clinical and functional outcome of Bipolar hemiarthroplasty done at our rural teaching set up, with experienced surgeons and adequate manpower are comparable to the high end sophisticated established urban teaching centres and corporate hospitals, which are very costly. The results of the present series were achieved with strict adherence to operation theatre discipline at all time like a team. We have used Harris Hip Score to analyze the results and 90% had good results. As this study was time-bound, the sample size was small, which will not reflective of the entire rural population. Despite these limitations in our study, we have several unique strengths like cost is meagre as compared to urban centres. Patients feel homely in the rural setup, as our set up and have no problem in follow up and travel as and when required. However, more studies in larger groups need to be done to establish the above facts and may reduce the cost with much better results.
Conflict of interest – None.
Source of funding – None.
Ethical Approval – Taken from an institutional ethics committee.
Acknowledgement – We would like to thank the patients and clinical & administrative staff of the hospital for their contribution to the study.
References:
1. Garrahan WF, Madden EJ. The long-stem bipolar prosthesis in surgery of the hip. Clin Ortho Related Res. 1990 Feb (251):31-7.
2. Marya SK, Thukral R, Hasan R, Tripathi M. Cementless bipolar hemiarthroplasty in femoral neck fractures in the elderly. Ind J Orth. 2011 Jun; 45: 236-42.
3. LaBelle LW, Colwill JC, Swanson AB. Bateman bipolar hip arthroplasty for femoral neck fractures. A five-to ten-year follow-up study. Clin Ortho Related Res. 1990 Feb (251):20-5.
4. Gallinaro P, Tabasso GI, Negretto RE, del Prever Brach EM. Experience with bipolar prosthesis in femoral neck fractures in the elderly and debilitated. Clin Orthopaed Related Res. 1990 Feb (251):26-30.
5. Lestrange NR. Bipolar arthroplasty for 496 hip fractures. Clin Orthopaed Related Res. 1990 Feb 1; 251:7-19.
6. Nottage WM, McMaster WC. Comparison of bipolar implants with fixed-neck prostheses in femoral-neck fractures. Clin Orth Related Res. 1990 Feb (251):38-43. Dudani B, Shyam AK, Arora P, Veigus A. Bipolar hip arthroplasty for avascular necrosis of femoral head in young adults. Ind J Orth. 2015 Jun;49:329-35.
7. Giliberty RP. Bipolar endoprosthesis minimizes protrusio acetabuli, loose stems. Orthop Rev. 1985; 14:27.
8. Mannarino F, Maples D, Colwill JC, Swanson AB. Bateman bipolar hip arthroplasty: A review of 44 cases. Orthopaedics. 1986 Mar 1;9(3):357-60.
9. Lausten GS, Vedel PE, Nielsen PM. Fractures of the femoral neck treated with a bipolar endoprosthesis. Clin Orthopaed Related Res. 1987 May (218):63-7.
11. Amite P, Malhotra R, Bhan S. Conversion of failed hemiarthroplasty to total hip arthroplasty: a short to a mid-term follow-up study. Indian journal of orthopaedics. 2008 Jul; 42(3):294.
|






 This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License